Determinants of psychosocial adjustment in newly diagnosed Multiple Sclerosis (MS) patients include not only disease-related factors but also cognitive-behavioral factors. This study aimed to investigate the level of depression and anxiety symptoms and to examine the role of cognitive distortions in the development of depression and anxiety in newly diagnosed MS patients.
Methods63 MS patients and 58 healthy controls 18–65 years of age were included. Hamilton Depression Scale (HAM-D), Hamilton Anxiety Scale (HAM-A), Dysfunctional Attitudes Scale (DAS), Automatic Thoughts Questionnaire (ATQ) were administered to the sample.
ResultsMS patients had significantly higher HAM-D and HAM-A scores (p<0.05). HAM-D and HAM-A scale scores were correlated with each other in the MS patients group (p<0.05). ATQ scores were significantly higher in the MS group than healthy controls (p<0.01). HAM-D and HAM-A scores were also both correlated with ATQ and DAS scores in MS patients group (p<0.05). There is a statistically significant difference for marital status and ATQ scores between the MS patients group with significant depressive symptoms (according to HAM-D cut off point above 17) and those without significant depressive symptoms (p<0.05). ATQ is the only independent variable that predicts the depression levels (OR=1.12 CI=1.068–1.176; p<0.001) in stepwise regression analysis. The overall disclosure percentage of the model to 52%.
ConclusionsAutomatic thoughts are a vulnerability factor for the development of depressive symptoms in newly diagnosed MS patients. Psychological stress affects not only MS patients with advanced-stage but also newly diagnosed MS patients.
Multiple Sclerosis (MS) is a common neurological disease that begins in young adulthood, requiring long-term adherence to disease-modifying therapies and other medical procedures from the time of diagnosis, and interrupting work, social and private life goals.1 In addition to the functional losses that it creates in daily life from the time of diagnosis, it also leads to significant psychosocial difficulties because of the uncertainties about the future and the disease-related unpredictable course.2 Therefore, encountering high rates of psychopathological conditions such as depression, anxiety, and a decrease in quality of life is not surprising in individuals with MS.3,4
Although it is determined that psychological well-being and quality of life are adversely affected in advanced stages of MS, MS has a significant negative effect on mental status in the diagnosis period when the physical losses associated with the disease are much less.1 It has been reported that mental distress is an important factor in the clinical picture in individuals with MS during the diagnosis period and that individuals in the early stage of the disease experience high levels of depression and anxiety.5,6 The evaluation of psychological components related to how the person experiences the disease, which has an impact on the disease adaptation in the early post-diagnosis period, is important for the healthy management of the long-term adaptation process.7
The role of many psychosocial factors in the adaptation process, such as ways of coping with MS, perceived stress level, coercive life events, and social support, is relatively well defined.8 Also, it is increasingly understood that individual psychological factors, including cognitive-behavioral factors, play a role in the adaptation process in MS as well as disease-related factors.9,10 In the study of Dennison et al. subjecting the psychological factors associated with the adaptation process in MS patients, they reported that cognitive distortions and maladaptive cognitions related to symptoms play a role in the adaptation process. Therefore, both general and disease-specific dysfunctional thoughts and behaviors are important in understanding the variables related to the adaptation process in individuals with MS.2
Current evidence targeting to understand the psychopathologies in MS within the cognitive model reveals that cognitive distortions, stable and generalized attributional styles, and negative affective memory errors are associated with higher depression in this patient population.11 Besides, it is reported that cognitive-behavioral interventions that include techniques such as identifying dysfunctional cognitions associated with emotional distress in MS patients and creating alternative thoughts and assisting the patient's adaptation process helps the individual's adaptation process with the disease.10 Cognitive-Behavioral Therapies (CBT) have the potential to improve many aspects of the experience of living with MS. CBT interventions are reported to be an effective method in reducing the symptoms of depression, mainly.10,12 Dennison et al. stated that the identification of psychological factors in the process of adaptation to MS at the stage when symptoms of emotional distress occur before the psychiatric diagnoses appear would be more beneficial in terms of better understanding and management of the adaptation process in both short and long term.11 Therefore, the identification of cognitive-behavioral factors associated with early psychological stress may be a guide for CBT interventions, which is an effective method in the treatment of anxiety and depression in MS.2,9 In addition, considering the difficulty in the differential diagnosis of depression, insomnia, anorexia, and memory disorders in individuals with MS, the identification of specific cognitive factors such as depressive beliefs of the patient will help in the differential diagnosis.13
Smith et al. highlighted that although these two disorders are strongly related in the psychopathologies developing in the chronic pain population, not all the chronic pain patients develop depression and in the group of individuals with the same disease who develop depression, a detailed evaluation related to cognitive model may lead to the aspect that more cognitive distortions are associated with depression.14 Similarly, although MS and depression are strongly associated,3 considering that not every MS patient develops depression, maladaptive cognitive factors may predispose to the development of psychopathologies such as depression and anxiety in individuals with MS, as in some other medical disorders.
This study aimed to investigate and determine the role of maladaptive cognitive factors associated with the development of mental distress characterized by depression and anxiety symptoms in patients with newly diagnosed MS during the adaptation process. Negative automatic thoughts and dysfunctional attitudes were assumed to be predisposing risk factors for depression and anxiety in newly diagnosed individuals with MS.
Material and methodsParticipantsThis was a cross-sectional, prospective, case-control study of examining the role of the cognitive distortions in the development of depression and anxiety in newly diagnosed MS patients.
Patients were recruited from the Neurology Unit of Bakırköy Research and Training Hospital for Neurology, Neurosurgery and Psychiatry, Istanbul, Turkey between July 2015-June 2016. Our sample was consisted of 63 patients who were diagnosed with MS based on Mc Donald diagnostic criteria15 and 58 age- and gender-matched healthy controls. Patients who had diagnosed as MS within the past six months and between 18 and 65 years of age were included to the study. Patients who have experienced a relapse in the previous month, had steroid use in the previous week, a past or current diagnosis of psychiatric disorder other than depression and anxiety were excluded. In total, 68 patients who met the inclusion criteria went on with a clinical interview and 2 refused to participate, 1 had psychotic disorder and 2 had the history of synthetic cannabinoid use in the last week. The patients who had psychotic comorbidity and substance use history were also excluded because of the possible misleading effects on the evaluation of the depression and anxiety. Consequently 63 MS patients were included to the final analysis. All the patients were diagnosed with relapsing remitting MS. 58 psychiatrically healthy control subjects who were selected from randomly among volunteer staff of Bakırkoy Research and Training Hospital were recruited during the same period. The current and past psychiatric history of the participants were obtained based on self-report information.
This study was approved by the Prof. Dr. Mazhar Osman Research and Training Hospital for Psychiatry, Neurology, and Neurosurgery Ethics Committee with Decision no. 501, dated 08 Dec 2015. Ethics Committee. Before participation, all subjects were informed about the design, methods, and purpose of the study, and written informed consents were obtained.
ProcedureThe test battery consisting of Sociodemographic Data Collection Form, Hamilton Depression Rating Scale (HAM-D), Hamilton Anxiety Scale (HAM-A), Dysfunctional Attitudes Scale (DAS), Automatic Thoughts Questionnaire (ATQ) were administered. The level of the disability related to MS was evaluated with the Expanded Disability Status Scale (EDSS). Patients with EDSS score up to 4 were included, and all of the patients. Patients in this range of scores are still mobile and able to walk at least 20m without assistance.
Measurement instrumentsHamilton Depression Rating Scale (HAM-D): HAM-D is a 17-item instrument administered by the clinician to assess the severity and level of depression.16 The validity and reliability studies of the Turkish version have been carried out by Akdemir et al.17 In our study, the HAM-D cut-off score was set as 14. Assessment of depressive symptoms with HAM-D may vary in the literature in terms of the cut-off score.18 While the high sensitivity of the HAM-D scale to measure somatic symptoms poses a disadvantage for our study population, the advantage is that HAM-D is a clinician-assessed scale.
The study of Raimo et al. investigating the psychometric properties of HAM-D in the evaluation of depressive symptoms in MS patients, HAM-D was found less differentiative on symptoms such as insomnia and other somatic symptoms for MS patients similar to other neurological diseases such as Parkinson's and dementia. The study reported that HAM-D was a practical and appropriate measurement tool for clinical and research use in MS, and the cut-off point of 14.5 and above had good sensitivity and specificity to evaluate depressive symptoms in the MS population.19
Also, considering the conducted studies in our country's population,20 14–18 points range in the Hamilton Depression Scale addressed ‘moderate severity” and above,17 and the cut-off score was taken as 14 for evaluating participants with significant depressive symptomatology.
Hamilton Anxiety Scale (HAM-A): HAM-A is a 14-item tool developed by Hamilton et al. in order to determine the level and symptom distribution of anxiety.21 The HAM-A assesses the level of emotional as well as somatic symptoms related to anxiety. The validity and reliability studies of the Turkish version have been performed by Yazici et al.22
Dysfunctional Attitudes Scale (DAS): DAS is a Likert type, self-administered 40-item instrument that assesses the dysfunctional beliefs and presumptions. It has been developed as a means to measure the presumptions and beliefs that can be associated with depression.23 Higher scores show an increased frequency of non-functional attitudes. The reliability and validity of the Turkish version have been shown by Şahin and Şahin in 1992.24
Automatic Thoughts Questionnaire (ATQ): This instrument measures the negative automatic thoughts that have been developed to assess the most frequent negative thoughts and negative self-judgment patterns that are thought to be associated with depression.25 The validity and reliability of the Turkish version have been shown by Şahin and Şahin in 1992.26
Expanded Disability Status Scale (EDSS): This instrument is used for determining the severity of disability associated with MS and assesses eight different domains.27
Statistical methodStatistical analyses were performed using SPSS v.21 software. The suitability of the variables according to the normal distribution, was examined using visuals (histogram and probability graphs) and analytical (Kolmogorov Smirnov and Shapiro–Wilk tests). Mann Whitney-U test was used in the statistical evaluation of the abnormally distributed numerical data between the two sample groups; Student's t-test was used for the statistical evaluation of the numerical data that fit the normal distribution between two sample groups.
The relationship between numerical variables was evaluated using Spearman Correlation Analysis when at least one of the variables did not fit into the normal distribution. Chi-square test and Fisher's test were used to compare categorical variables between the groups.
Logistic regression analysis was used to examine the independent predictors affecting the presence of depression in MS patients. ATQ, DAS score variables with p value <0.25 and gender and age were included in the logistic regression model. In the model, gender was taken as the nominal variable (coded as male=1, female=0), and age and scale score variables were included in the model as numerical variables. The absence of strong correlations between the independent variables was tested. Hosmer–Lemeshow test was used for model fit. In all analyze, the statistical significance level was accepted as p <0.05.
ResultsA total of 68 MS patients were interviewed, and five patients were excluded from the study for the following reasons; two patients refused to give written informed consent, one patient had psychotic symptoms, and two patients had a history of using synthetic cannabinoids. Data of 121 participants (63 MS patients and 58 healthy controls) were analyzed. The mean age was 30.98 (±7.71) for the MS patient group, and 32.07(±8.06) for the control group.
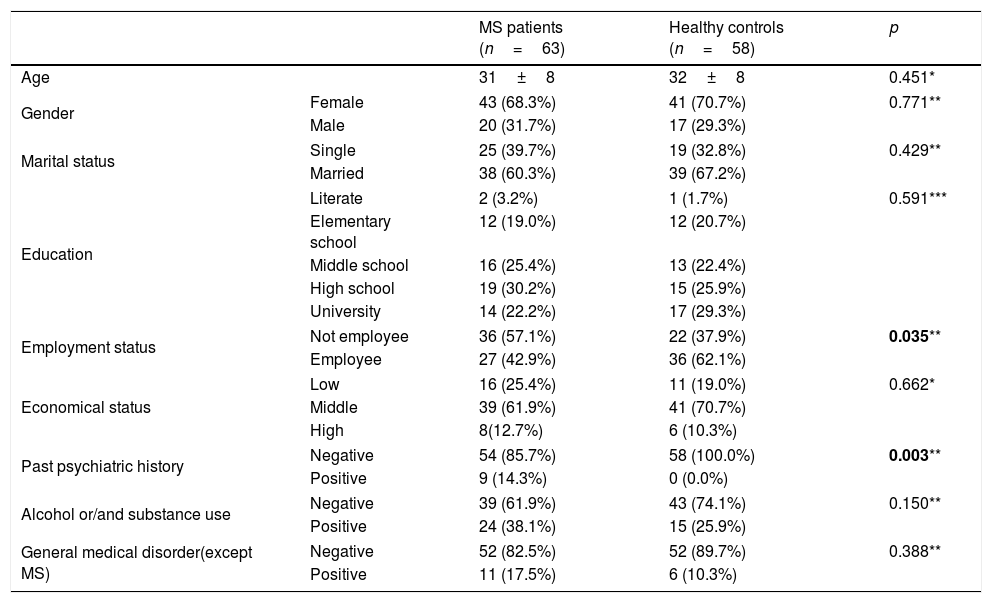
Patients and control subjects were not significantly different in terms of sociodemographic characteristics (p>0.05) except past psychiatric history and occupational status. Table 1 summarizes the sociodemographic characteristics of the participants.
Socio-demographic characteristics of the groups.
| MS patients (n=63) | Healthy controls (n=58) | p | ||
|---|---|---|---|---|
| Age | 31±8 | 32±8 | 0.451* | |
| Gender | Female | 43 (68.3%) | 41 (70.7%) | 0.771** |
| Male | 20 (31.7%) | 17 (29.3%) | ||
| Marital status | Single | 25 (39.7%) | 19 (32.8%) | 0.429** |
| Married | 38 (60.3%) | 39 (67.2%) | ||
| Education | Literate | 2 (3.2%) | 1 (1.7%) | 0.591*** |
| Elementary school | 12 (19.0%) | 12 (20.7%) | ||
| Middle school | 16 (25.4%) | 13 (22.4%) | ||
| High school | 19 (30.2%) | 15 (25.9%) | ||
| University | 14 (22.2%) | 17 (29.3%) | ||
| Employment status | Not employee | 36 (57.1%) | 22 (37.9%) | 0.035** |
| Employee | 27 (42.9%) | 36 (62.1%) | ||
| Economical status | Low | 16 (25.4%) | 11 (19.0%) | 0.662* |
| Middle | 39 (61.9%) | 41 (70.7%) | ||
| High | 8(12.7%) | 6 (10.3%) | ||
| Past psychiatric history | Negative | 54 (85.7%) | 58 (100.0%) | 0.003** |
| Positive | 9 (14.3%) | 0 (0.0%) | ||
| Alcohol or/and substance use | Negative | 39 (61.9%) | 43 (74.1%) | 0.150** |
| Positive | 24 (38.1%) | 15 (25.9%) | ||
| General medical disorder(except MS) | Negative | 52 (82.5%) | 52 (89.7%) | 0.388** |
| Positive | 11 (17.5%) | 6 (10.3%) | ||
Among the patient group, 14 (22.24%) were receiving medications for MS, while 46 (73%) were medication-free. Of the patients who were on MS medications, one was receiving treatment with interferon beta-1a, 1 with interferon beta-1b, 5 with glatiramer acetate, 7 with recombinant interferon beta-1a. The average time to diagnosis was 7.6 (±10.72) weeks, while the average duration of time since the onset of MS-related symptoms was 6.91 months (±17.487 months).
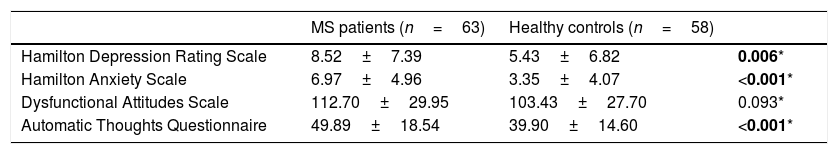
MS patients had significantly higher HAM-D and HAM-A scores than controls (p<0.05). Mean HAM-D scores were 8.52±7.39, and HAM-A scores were 6.97±4.96 in MS patients group (Table 2).
Comparison of depression, anxiety, dysfunctional attitudes and automatic thoughts scores of MS patients group and healthy controls.
According to the cut-off score of HAM-D (≥14), the rate of depressive symptoms was 25.4% in the MS group and 15% in the healthy control group.
While we did not find a statistically significant difference between the groups for DAS scores, ATQ scores were significantly higher in the MS group (p<0.01) (Table 3).
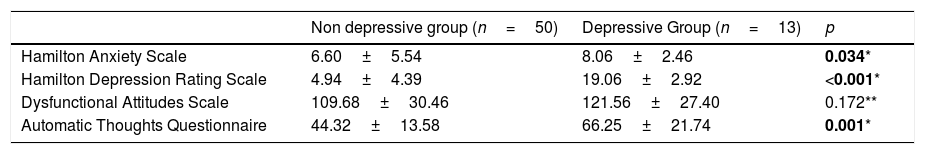
Comparison of the depression, anxiety, dysfunctional attitudes and automatic thoughts scores of the depressed and non-depressed MS patients groups.
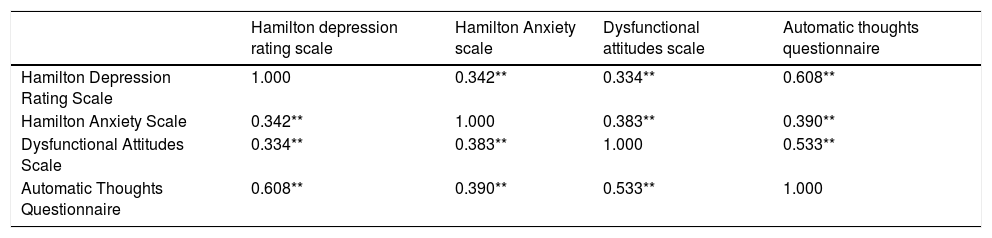
HAM-D and HAM-A scale scores were correlated with each other in the MS patients group (p<0.05). HAM-D and HAM-A scores were also both correlated with ATQ and DAS scores in MS patients group (p<0.05) (Table 4).
Correlation matrix of the depression, anxiety, dysfunctional attitudes and automatic thoughts in MS patients group.
| Hamilton depression rating scale | Hamilton Anxiety scale | Dysfunctional attitudes scale | Automatic thoughts questionnaire | |
|---|---|---|---|---|
| Hamilton Depression Rating Scale | 1.000 | 0.342** | 0.334** | 0.608** |
| Hamilton Anxiety Scale | 0.342** | 1.000 | 0.383** | 0.390** |
| Dysfunctional Attitudes Scale | 0.334** | 0.383** | 1.000 | 0.533** |
| Automatic Thoughts Questionnaire | 0.608** | 0.390** | 0.533** | 1.000 |
We found a statistically significant difference in marital status and ATQ scores while comparing the patients with significant depressive symptoms and those without significant depressive symptoms in the MS group (p<0.05). There is also significant difference in ATQ scores while comparing the participants with significant depressive symptoms (66.56±18.66, n=9) and those without significant depressive symptoms (35.00±6.12, n=49) in the control group (p<0.05).
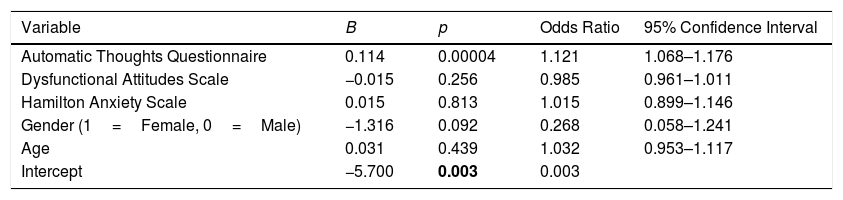
Gender, age, HAM-A, ATQ, and DAS scores were taken in stepwise regression analysis as independent variables sequentially. We found ATQ is the only independent variable that predicts the depression levels and increases depression risk 1.12 times (OR=1.12 CI=1.068–1.176; p<0.001), overall disclosure percentage of the model to 52%. The results of the logistic regression analysis were summarized in Table 5.
The results of the logistic regression analysis.
| Variable | B | p | Odds Ratio | 95% Confidence Interval |
|---|---|---|---|---|
| Automatic Thoughts Questionnaire | 0.114 | 0.00004 | 1.121 | 1.068–1.176 |
| Dysfunctional Attitudes Scale | −0.015 | 0.256 | 0.985 | 0.961–1.011 |
| Hamilton Anxiety Scale | 0.015 | 0.813 | 1.015 | 0.899–1.146 |
| Gender (1=Female, 0=Male) | −1.316 | 0.092 | 0.268 | 0.058–1.241 |
| Age | 0.031 | 0.439 | 1.032 | 0.953–1.117 |
| Intercept | −5.700 | 0.003 | 0.003 |
Nagelkerke R2=0.517.
In our study, the relationship between depression and anxiety symptoms in newly diagnosed MS patients was examined with sociodemographic characteristics, automatic thoughts, and dysfunctional attitudes, and the results were compared with the findings of healthy controls.
The 2:1 female–male ratio that we found is consistent with the findings of previous studies on gender distribution in MS.20 The MS group did not differ significantly in terms of the unemployment rate and duration (p>0.05). This situation can be explained by the fact that our sample consisted of newly diagnosed MS patients, and the patients were not notably affected by the disease-related facts yet.
The study of Fantoni-Quinton et al., which examined the effect of MS on working life and the strategies that should be taken in order for the patient to continue working, reported that the average time between diagnosis of MS and the inability to work due to disease was 24 years.28 Apart from our findings, Pearson et al. reported that MS had a significant effect on the working status, which was also valid in the early stages of the disease.29 Our findings are in line with the results of studies reporting that early functionality is not affected in MS.
In the MS group, the previous psychiatric history was significantly higher compared to the control group (p<0.05). Psychiatric symptoms may accompany MS from the onset.5 Especially because of the difficulties caused by somatic symptoms regarding differential diagnosis, individuals with MS who are yet not diagnosed can have psychiatric diagnoses priorly.13 In our randomized sample, the statistically significant difference disappears regarding the past psychiatric history between patients with and without depressive symptoms in the MS group. This finding might indicate that the significant difference concerning the psychiatric history between the MS and the control group might be related to differential diagnosis difficulties caused by coincident symptomatology in the psychiatric history of the patient, rather than the possibility that the existence of the medical history is a factor predicting the present psychopathology.
According to our findings, depression and anxiety symptoms were significantly higher in the MS group compared to the healthy controls (p<0.05). The study by Giordano et al. investigating anxiety and depression in MS patients found that anxiety symptoms were widespread and persistent in the period following the explanation of the diagnosis but decreased over time, and depressive symptoms were less common but more stable. These findings highlight the importance of timely detection of these symptoms in individuals with MS in terms of both predicting the development of depression in the long term and carrying out all therapeutic interventions, including psychological interventions.30
Janssen et al. conducted a study with MS patients who have been diagnosed in the last two years and their relatives, and reported that both patients and their relatives experienced clinically high levels of anxiety and emotional stress characterized by depression and more reduced quality of life which was a stimulating finding for the treatment team in terms of the need for psychological support.6 Moreover, they reported that high levels of anxiety occurring after diagnosis did not indicate anxiety and difficulty for this period alone; it was also predictive for the anxiety and psychological distress during the patient's follow-up. Therefore, they emphasize that a simple and effective strategy such as screening and detecting anxiety symptoms in the diagnosis process in MS patients will give the chance to detect and eliminate the negative psychological effects of the disease such as depression, anxiety, and other emotional distress symptoms in the following period.31
The sample of our study consisted of individuals diagnosed with MS in the last six months, and our findings suggest significantly higher levels of depression and anxiety in MS patients compared to healthy controls, which is in line with the findings of these studies. Our findings emphasize the importance of the evaluation of the psychological difficulties that are important for the course of the disease in MS patients during the diagnosis period, as it is in the later stages of the disease, in order to allow the planning of existing symptomatology treatments in this early period.
In the MS group, the ATQ scores of the participants with depression were significantly higher than those without depression (p<0.05). Lefebvre and Smith et al. reported that cognitive distortions were associated with depression in the pain population, just as the association in psychiatric depression patients. However, this relationship found in the Lefebvres back pain group, states that maladaptive cognitive structures such as cognitive distortions present in the person may be effective in the development of depression by interacting with the stress caused by acute back pain.32,33 In another study by Smith et al. examining the relationship between cognitive distortions, depression and disease severity in individuals with rheumatoid arthritis and investigated the development of depression in this patient group regarding Beck's model, they found that cognitive distortions, both general and arthritis-related, were significantly related to depression independent of the disease severity.34 In addition, in the study by Smith et al., consisting of advanced rheumatoid arthritis patients, cognitive distortions play an essential role in the development of depression along with ‘desperation’.35 Our findings suggest that cognitive distortions involving negative automatic thoughts are associated with the development of depressive symptoms in newly diagnosed MS patients as a maladaptive cognitive component. This finding is in line with the findings of studies showing the role of maladaptive cognitive factors in depression occurring in other general medical diseases and points out the importance of the detection of maladaptive cognitive factors during the diagnostic period while assessing the emotional distress. When ATQ scores of the participants with significant depressive symptoms and those without significant depressive symptoms in the control group have been compared, ATQ scores of the participants with depression were also significantly higher than those without depression (p<0.05). The one of the well-known cognitive factors associated with depression involve the maladaptive thinking styles and the automatic negative thoughts.36 Moreover the negative automatic thoughts are the most frequent negative thoughts and negative self-judgment patterns that are thought to be associated with depression.25 The findings of our study which reveal the role of negative automatic thoughts in the development of depressive symptoms in newly diagnosed MS patients extends the prior empirical and theoretical work by examining these constructs in a patient population that has not previously been investigated.
According to the results of our study, no statistically significant difference was found between the groups with and without depression in the MS group regarding DAS scores (p>0.05). In the literature, there are studies reporting that dysfunctional attitudes play a role in the development of depressive symptomatology in individuals with medical diseases as in the general population. The study of Ma et al. conducted on 245 type 2 diabetes patients, found that dysfunctional attitudes which is a cognitive factor predisposing to depression, were associated with glycemic control and stated that screening of dysfunctional attitudes would allow the detection and timely intervention of diabetic patients who are at high risk of developing depressive symptomatology.37
The study investigating the role of dysfunctional attitudes and rumination in the development of non-somatic depressive symptomatology in newly diagnosed cancer patients in the Asian population by Lam et al. found that dysfunctional attitudes and rumination had a bidirectional mediating role in the development of depressive symptoms.38 According to the results of our study, unlike other general medical diseases reported in the literature, dysfunctional attitudes in newly diagnosed MS patients were not associated with the development of depressive symptomatology.
Olinger and Kuiper defined the role of dysfunctional attitudes in the development of depression within an interactive model and reported that dysfunctional attitudes predispose to depression by interacting with stressful life events.39 In terms of the evaluation of the depressive formation, Dobson and Breiter reported that ATQ was a more specific and descriptive measure for the cognitive assessment of depression compared to DAS.40 Considering our findings suggesting that negative automatic thoughts are more common in the MS group with depressive symptoms, the lack of dysfunctional thoughts related to the development of depression in MS may be due to the characteristics of the instruments used.
The model in which gender, age, HAM-A, ATQ, and DAS scores were included in regression analysis as independent variables, respectively, the only independent variable increasing the depression risk was found as ATQ (p<0.001) and it is found that each 1 unit increase in the ATQ score increased the depression risk 1.12 times (OR=1.12 CI=1.068–1.176). The model explained 52% of the total variance.
Dennison et al. investigated the adaptation process in early MS patients within the context of a cognitive-behavioral model and examined the effect of cognition and behaviors together with the factors related to the severity of the disorder and the cognitive-behavioral responses including the dysfunctional beliefs and behavioral responses to the disease. They found that these factors predict the psychological and functional distress more strongly than those related to disease severity.2 The study of Shnek et al., investigating the predictive role of learned helplessness, self-efficacy, and cognitive distortions in the development of depression in MS and spinal cord injury patients, reported that only learned helplessness and self-efficacy were predictive for depression for both groups when evaluated together with cognitive distortions. However, they expounded this finding as cognitive distortions had an indirect effect on depression by causing feelings of helplessness and low self-efficacy, and thus may be mediating the development of depression.9
Comorbid psychiatric symptomatology is not a rule for newly diagnosed MS patients. Depression and anxiety symptoms appear in some of the patients, while others do not reveal these symptoms. This situation may be determined by the cognitive-behavioral response of the individual to the disease rather than disease-related factors.2 Our findings which reveal the role of cognitive distortions regarding the automatic thoughts in the development of depression in MS patients, point out the importance of the focusing on cognitive elements of the psychological response to the disease which are easy to detect and modify as well as the biological factors.
In the comparative study by Kwon and Oei, the role of non-functional attitudes and automatic thoughts in the development of depression was examined. They reported that non-functional attitudes had a modulating role, and maladaptive cognition had a mediating role in the development of depression within the framework of Beck's cognitive model. They also defined the process leading to depression by a vicious cycle model in which maladaptive cognitions were predisposing for depression, and depression was affecting maladaptive cognitions.41 Our findings reveal the predictive role of maladaptive cognitions, including automatic thoughts in the symptoms of depression in MS patients, but suggest that dysfunctional attitudes are not associated with depressive symptomatology. Furlong and Oei examined the change in automatic thoughts and dysfunctional attitudes by CBT application in depression and found that automatic thoughts had a stronger relationship with the change in both cognitive and somatic depressive symptoms compared to dysfunctional attitudes.42 Similarly, Persons and Burns reported that the change in automatic thoughts is strongly correlated with the change in mood during the individual CBT process.43 In the light of these data, our findings suggesting that automatic thoughts are risk factors for the development of depressive symptoms in individuals with MS could be a guide for psychological interventions for depression in MS.
As a result, the findings of our study support the evidence in the literature, which concludes that the presence of psychological distress characterized by anxiety and depression symptoms in MS patients who are in the adaptation process during the diagnostic period similar to the later stages of the disease.
In addition, our study reveals that, as in some other general medical disorders, predisposition in cognitive structuring is a risk factor in the development of depression symptoms and maladaptive cognitive elements, including automatic thoughts, predict the development of depressive symptoms in MS patients.
Unlike the factors related to disease severity in MS, the detection of cognitive-behavioral variables, which are modifiable elements, will be useful in psychological interventions in the process of adaptation to MS.2 On this basis, the findings of our study regarding clinical applications highlights the priority of detecting automatic thoughts during BDT which is a psychological treatment method with proven efficacy12 as well as the maladaptive cognitive element's guiding role in identifying risks for the development of depression symptoms and establishing treatment protocols.
There are many limitations in our study. Firstly, the small sample size and the cross-sectional design limits the generalization of the findings on the whole MS population and to make causal inferences from the results. Future longitudinal research would be useful for consolidating these findings. Secondly, the lack of including the neurological clinical variables related to the disease in the assessment limits the interpretation of the effects of these variables on the psychological distress during adaptation period to MS.
On the other hand, according to our knowledge, our study is the first study to investigate the relationship between symptoms of depression and maladaptive cognitive factors in early MS. Further studies, including long-term follow-up studies with larger sample sizes, will contribute to the identification factors that predispose to early psychological distress in individuals with MS and help determine treatment strategies.
Ethical considerationsThe study protocol was approved by Prof. Dr. Mazhar Osman Research and Training Hospital for Psychiatry, Neurology, and Neurosurgery Ethics Committee with Decision no. 501, dated 08 Dec 2015.
FundingThere was no funding for this work.
Conflict of interestThe authors have no conflict of interest to declare