A 62-year-old woman with a history of hysterectomy and oophorectomy for uterine cancer, left parathyroidectomy for Warthin's tumour and bladder neoplasia treated with transurethral resection (TUR), complaining of back pain.
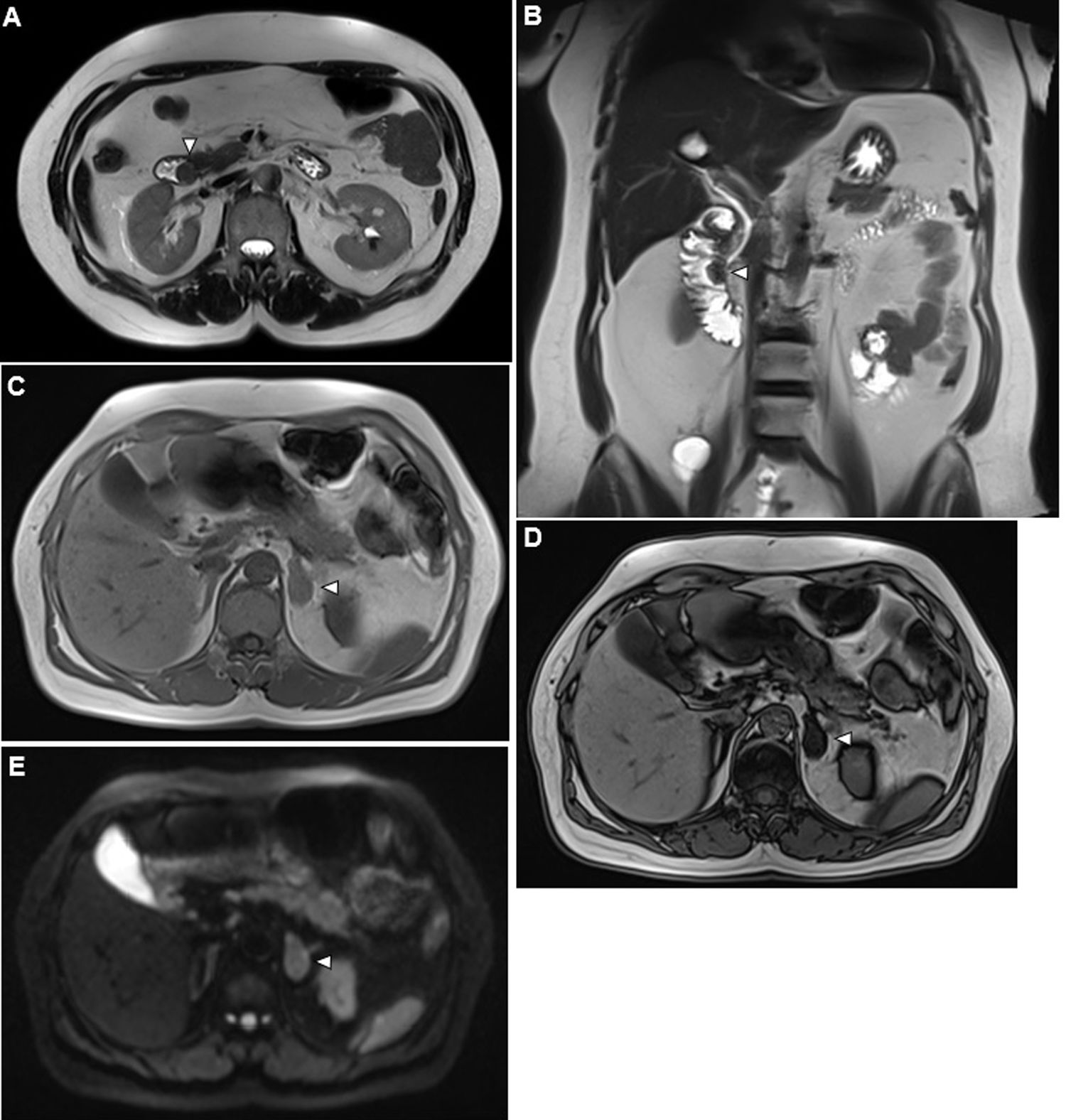
Abdominal CT (Fig. 1A/B) and abdominal MRI (Fig. 1C/D/E) were performed, showing a 29-mm left adrenal nodule, well defined, hypointense and homogeneous in all sequences, compatible with adenoma and an ampullary lesion of 15mm, solid hypointense in all sequences, compatible with ampullary tumour.
Axial (A) and coronal (B) T2 MRI shows a solid mass protruding inside the second duodenal portion at the location of the ampulla of Vater (arrowhead). This image is compatible with an ampullary tumour. MRI (C-D-E). A left adrenal lesion (arrowhead) is observed, showing signal drop between in-phase (C) and out-of-phase (D) images weighted in T1. This absence of signal indicates the presence of intracellular fat, considered diagnostic of adrenal adenoma. No restricted diffusion was demonstrated (E).
Both a liver function test and a hormonal study were normal, ruling out a hyperfunctioning adrenal lesion (dexamethasone suppression test, catecholamines, aldosterone and baseline renin activity).
Endoscopic ultrasound (EUS): ampullary adenoma with growth in the bile duct (N0). Biopsy: signet ring cell adenocarcinoma inside villous adenoma.
In the presence of a left adrenal lesion in a patient with confirmed ampullary malignancy, PET/CT was performed, which showed focal left adrenal uptake (SUVmax 4.6), without ampullary uptake. Fine-needle aspiration biopsy (FNAB) was performed for the adrenal lesion, with unsatisfactory cytology results.
Faced with focal adrenal uptake on PET/CT, without histological confirmation of metastasis in a patient suitable for surgical intervention, a left adrenalectomy was performed with a negative intraoperative study for malignancy, so the proposed oncological surgery was continued and a cephalic pancreatoduodenectomy was performed.
Histological report: left adrenal adenoma and ampullary signet ring cell adenocarcinoma in ampullary villous adenoma, with free margins (pT1aN0).
Up to 50% of all incidental adrenal masses in patients with known malignancy would harbour metastases.1 PET/CT is the standard in patients with solitary adrenal lesion and known malignancy, because most adrenal adenomas have low metabolic activity, while malignant adrenal lesions have high metabolic activity,1,2 with sensitivity and specificity of 97% and 91%, respectively.
According to the literature, focal adrenal uptake on PET/CT reaches a false positive rate of up to 20%.1,2 Currently, and with these data, there is no consensus on the best measure (adrenal SUVmax versus the adrenal-to-liver SUV ratio), nor on the SUVmax cut-off point, to distinguish between malignant and benign adrenal lesions.3
More studies are needed on the incidental findings of PET/CT in patients with pancreatic cancer. Its use should be considered in patients at high risk of metastasis. There is no specific literature focusing on adrenal metastases of cancer from benign prostatic hyperplasia (BPH).
Therefore, a focal adrenal uptake on PET/CT is highly suggestive of malignancy and more diagnostic studies are necessary. Adrenal biopsy should be considered,1,2 and in the event of inconclusive results, the risk and advantages of cancer surgery should be included in the decision-making and preoperative counselling with the patient and the treating oncologist.
Conflicts of interestThe authors declare that they have no conflicts of interest.
Please cite this article as: Manuel Vázquez A, Latorre Fragua R, Gijón de la Santa L, de la Plaza R, Ramia JM. Captación adrenal en PET/TC en paciente con neoplasia de páncreas: no siempre metástasis. Gastroenterol Hepatol. 2021;44:425–427.