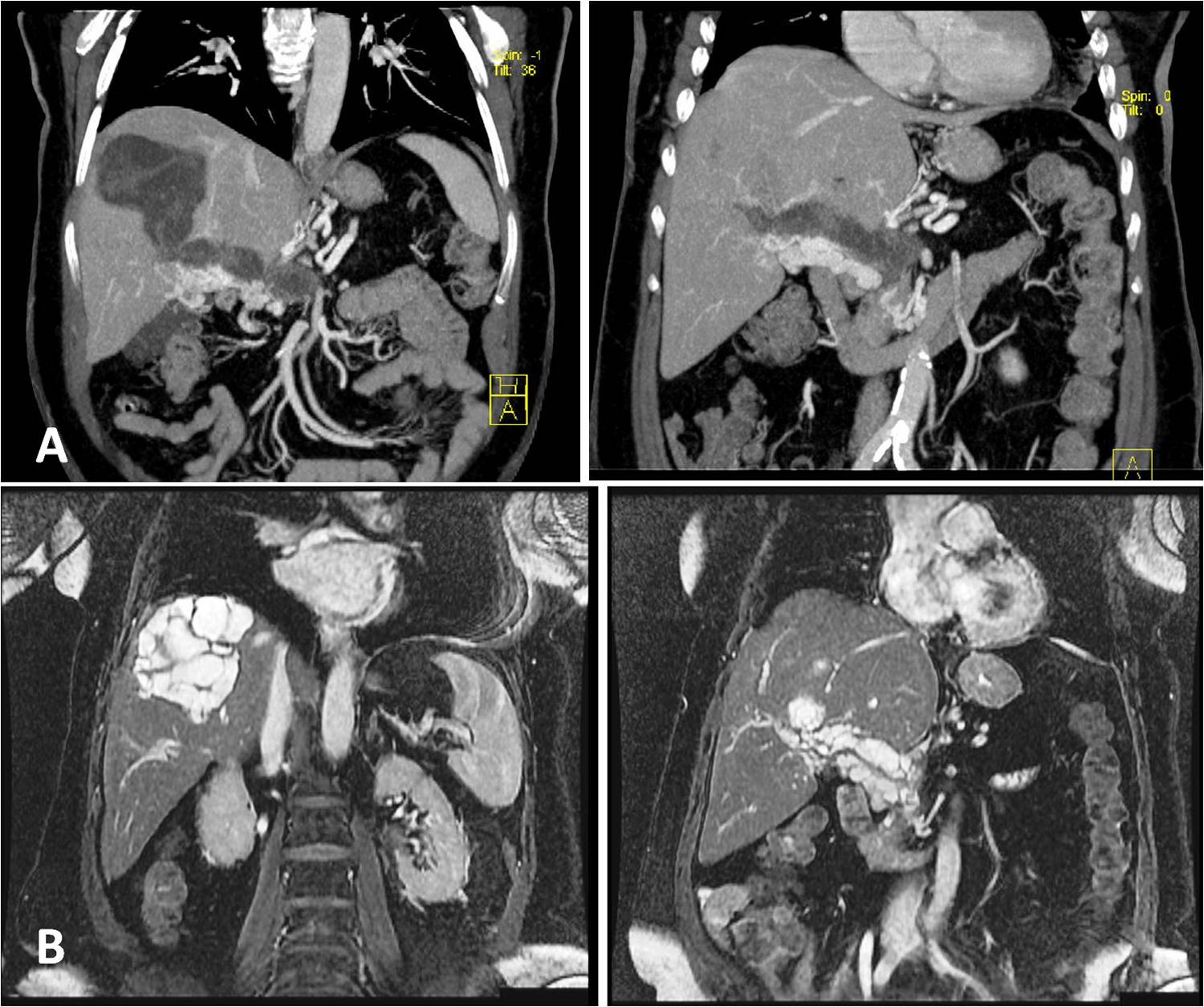
A 79-year-old-woman presented with a 4 month history of increasing epigastric and right upper quadrant abdominal pain, weight loss and abdominal distension. On physical examination she presented vague abdominal pain. The blood test was normal including hydatid serology but the ultrasonography reveal two hydatic cysts within the liver. The bigger one was located on hepatic segment VIII and the small one was adjacent to hepatic hilum. Both cysts were multivesicular and multiseptated (Gharbi ultrasound classification type III) and were extending into the portal hilum. A computed tomography (CT) scan showed multiple contrast material filling the portal lumen and the lack of flow within the portal venous system. There was also a network of collateral dilated and tortuous periportal veins which suggests portal cavernomatosis. Magnetic resonance imaging (MRI) confirmed the portal cavernous transformation, the two multilocular cysts that extent into the portal hilum and also confirmed a direct communication between these structures and the portal vein. The patient did not agree with the surgery. Also she refused to perform other investigations such an upper gastrointestinal endoscopy. Therefore she was discharged and followed up in the out patient clinic. A treatment with albendazole was prescribed however after a few months the follow up was discontinued because the patient moved to anoyher city (Fig. 1).
Hydatid cyst disease is worldwide zoonosis particularly seen in Mediterranean regions such as Spain. The classical hydatid disease is well known; however its complications and the unusual anatomical locations are not easily recognized. Patients are usually asymptomatic unless complications occur. Symptoms are produced by mass effect and depend on location and size of cysts, speed of growth and complications. Cyst rupture and infection are the most common complications. The liver is the most commonly affected organ, followed by the lungs. Symptoms include obstructive jaundice and abdominal pain. Communication with the bile duct often occurs. Diaphragmatic migration, thoracic involvement, peritoneal seeding or perforation into hollow viscera are other complications that may occur. Hematogenous dissemination can also happen but direct portal vein invasion by cysts is very rare.1 Portal vein invasion usually occurs when the lesion is located in the hilium.1,2 Typically the external compression of the portal system causes obstructed flow, thrombosis and secondary a network of collateral veins is developed producing the cavernomatosis.2,3 However cavernomatosis can also be a consequence of direct vein invasion. The mechanism of porto-cyst fistula seems to be an inflammation of the vessel wall because of the compression by the cyst. This vascular inflammation finally creates a communication between the vein and the cyst.4 The lumen is then occupied by daughter vesicles that are seen in the magnetic resonance as multiple contrast material.1,4
Abdominal ultrasound is the most widely used technique and is also used to monitor the efficacy of treatment. Most commonly used classifications related to sonographic appearance are classifications of Gharbi and the World Health Organisation Informal Working Group classification on echinococcosis (WHO-IWGE).1 CT is an important diagnostic modality with higher sensitivity and specificity in assessing complications. MRI is superior for demonstrating cyst wall defect and biliary communication.1 In our case the MRI was definitive in confirming the presence of these daughter vesicles invading the portal vein and a direct communication between the cysts and the vein. Familiarity with these atypical complications helps to make an early and accurate diagnosis.
The treatment of choice is surgery, including removal of the cyst and local instillation of scolicide solution. Hepatectomy can also be perform with low morbidity and mortality. In addition to surgery, administration of albendazole is recommended. Patients with portal hypertension have risk of variceal bleeding and other related-complitations therefore treatment should also consist of drugs decreasing the portal venous pressure or procedures to treat the portal hypertension.
To our knowledge only a few publications describe this rare complication. However although it's rareness it should be keep in mind because of its possible serious consequences.2,4,5
Conflict of interestThe authors declare that they have no conflict of interest.