The COVID-19 pandemic changed the work routine of professionals at the family healthcare center (Núcleo de Atenção à Saúde da Família – NASF-AB), providing new conditions and work overload.
ObjectiveThe purpose of this study was to explore factors associated with work overload in NASF-AB professionals during the COVID-19 pandemic.
MethodsA cross-sectional study was carried out with NASF-AB workers in the city of Salvador, Bahia, Brazil, from May to August 2021. Working conditions and overload were assessed using the National Program for Improving Access and the Quality of Primary Care questionnaire (Programa Nacional de Melhoria do Acesso e da Qualidade da Atenção Básica – PMAQ) and the scale measuring burden of professionals in mental health services (Escala de Avaliação da Sobrecarga de Profissionais em Serviços de Saúde Mental – IMPACTO-BR), respectively. A multivariate linear regression model was used. A total of 68 health professionals participated in the study, including 19 physiotherapists, 13 occupational therapists, 10 social workers, 10 nutritionists, 9 psychologists and 7 physical education professionals.
ResultsThere was a significant association between overall overload and being female (p=<0.005), having spaces for reflection on the work process (p=0.027), and having difficulty moving around to conduct activities in the territory (p=0.002) for increasing the chance of work overload.
ConclusionsOur findings encourage workers’ health policies and closer ties and negotiation with local management, as well as the return of the institutional support figure for the effectiveness and resolution of actions in primary healthcare units.
La pandemia por COVID-19 cambió la rutina de trabajo de los profesionales del Núcleo de Atención a la Salud de la Familia (NASF-AB), proporcionando nuevas condiciones y sobrecarga de trabajo.
ObjetivoEl propósito de este estudio fue explorar los factores asociados a la sobrecarga de trabajo en profesionales de NASF-AB durante la pandemia por COVID-19.
MétodosSe realizó un estudio transversal con trabajadores de NASF-AB en la ciudad de Salvador, Bahía, Brasil, de mayo a agosto de 2021. Las condiciones de trabajo y la sobrecarga se evaluaron mediante el Programa Nacional de Mejoramiento del Acceso y la Calidad de la Atención Primaria. cuestionario (Programa Nacional de Melhoria do Acesso e da Qualidade da Atenção Básica [PMAQ]) y el cuestionario IMPACTO-BR, respectivamente. Se utilizó un modelo de regresión lineal multivariado. En el estudio participaron un total de 68 profesionales de la salud, entre ellos 19 fisioterapeutas, 13 terapeutas ocupacionales, 10 trabajadores sociales, 10 nutricionistas, 9 psicólogos y 7 profesionales de educación física.
ResultadosHubo asociación significativa entre sobrecarga general y ser mujer (p≤0,005), tener espacios de reflexión sobre el proceso de trabajo (p=0,027) y tener dificultad para desplazarse para realizar actividades en el territorio (p=0,002), para aumentar las posibilidades de sobrecarga de trabajo.
ConclusionesNuestros hallazgos alientan políticas de salud de los trabajadores, y el acercamiento y negociación con la dirección local, así como el retorno de la figura de apoyo institucional para la efectividad y resolución de acciones en las unidades primarias de salud.
In the context of the COVID-19 pandemic, new attributions and skills were required from workers due to the various changes experienced in society.1,2 This change in Brazil was accompanied by the aging process of the population and the increase in the prevalence of chronic-degenerative diseases with a large increase in the demand for care in primary healthcare (PHC) units and the consequent indispensability of collaborative and interprofessional action.3
Interprofessional work requires specific skills, such as communication between different actors, user-centered attention, clarity of roles, team dynamics, collaborative leadership and conflict resolution skills.4 Despite the fact that these skills are relevant to provide health care, studies indicate that there are difficulties in professional training, which can affect the employee's involvement with their work and increase the feeling of overload.5 In the context of PHC in Brazil, especially considering its complexity and broad capacity for action, the family health strategy – ESF of the unified health system – SUS proposes to reorganize primary care and understand health as a broad field of work from a biopsychosocial perspective.6
This proposal to integrate the field of health work was accompanied by the need to expand the action scope of the family health teams which were composed of doctors, nurses, technicians and dentists. This expansion took place nationwide through teams from the family healthcare and primary care centers – NASF-AB. The NASF-AB is responsible for supporting around eight family health (FH) teams and must be committed to promoting changes in the attitude and performance of FH professionals and among its own NASF-AB team, including intersectoral and interdisciplinary actions, promotion, prevention and rehabilitation.7
Considering the complexity of the process of this work, these workers are expected to have varied and complex knowledge in different fields of knowledge, whether technical, social, historical, political, among others; to intervene in different fields, as well as that these professionals act in a multi and interdisciplinary team and that they can mediate the necessary social changes, particularly in face with pandemic scenarios. The purpose of this study was to explore the factors associated with the overload of health professionals working at the NASF-AB in Salvador, Bahia, Brazil, during the COVID-19 pandemic.
MethodsThis is a cross-sectional study conducted with health professionals from the family healthcare center (Núcleo de Atenção à Saúde da Família – NASF-AB) in Salvador, Bahia, Brazil. The study was approved by the Ethics Committee for Research with Human Beings of the State University of Bahia, with number CAEE no. 39364120.3.0000.0057. All participants signed the informed consent form (ICF).
Characteristics of participantsNASF-AB workers were invited to participate in this study. All NASF-AB units in Salvador have the same composition, differing only in the number of professionals in each area. There are 12 multidisciplinary teams in Salvador, distributed in 12 health districts, supporting an average of 108 family health teams. Each family health team is responsible for around 3000 people. Working during the pandemic period context was considered as inclusion criteria, and those who were on vacation or on leave during the data collection phase carried out from May to August 2021 were excluded. Recruitment of the target sample was conducted based on initial disclosure via social networks and emails, as well as direct contacts with the management team.
A total of 80 professionals composed the NASF-AB during the data collection period. From this total, 12 workers were excluded from the sample due to vacation (n=2), absence from work (n=6) and refusals (n=4). Therefore, the final sample was 68 health professionals.
Procedures, measurements, variables and outcomeThe external assessment questionnaire of the third cycle of the National Program for Improved Access and Quality in Primary Care – PMAQ was used to assess working conditions. The PMAQ was previously used in other studies carried out in Brazil to evaluate the organization of the work process of the primary healthcare – PHC in Rio de Janeiro8 to provide evidence on the program to improve access and quality of PHC9 and to assess the effects of the PMAQ on hospitalizations for sensitive conditions to PHC.10
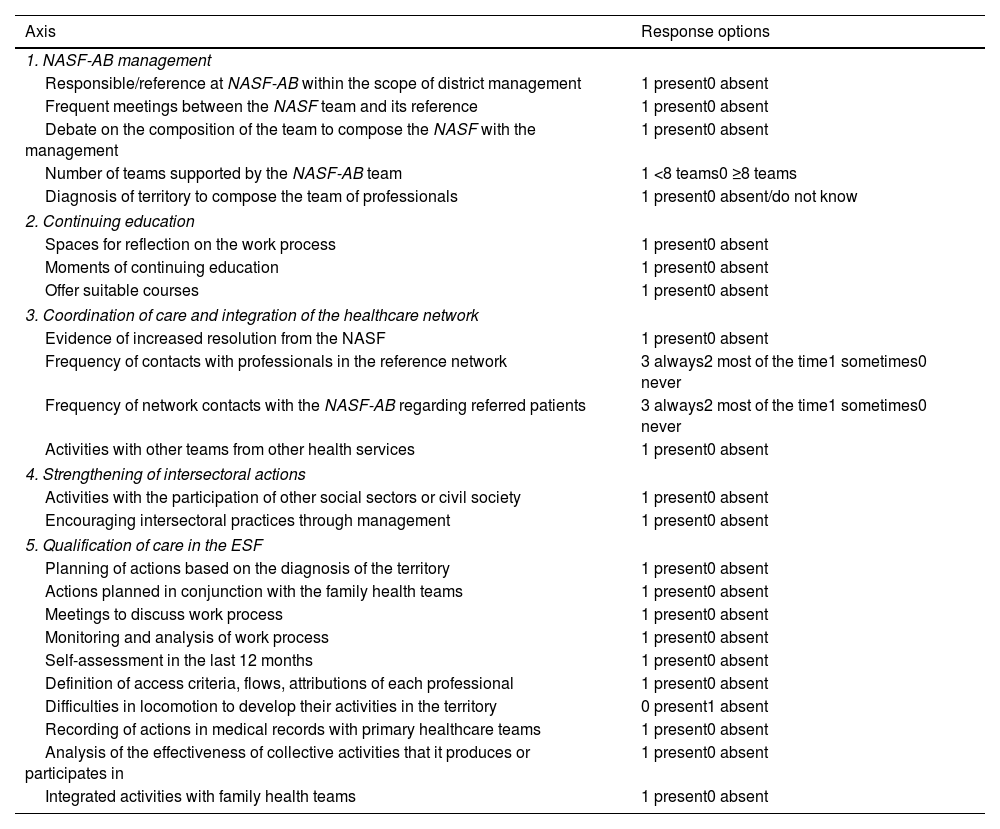
The original instrument has 108 questions about PHC. The five axes related to the management and work process of the NASF-AB were used in this study: (i) management of the NASF-AB at the municipal level (five questions); (ii) continuing education (three questions); (iii) coordination of care and integration of the healthcare network (four questions); (iv) strengthening of intersectoral actions (two questions); (v) ESF care qualification (10 questions)6 according to Table 1.
Questions used to assess working conditions in the NASF-AB.
| Axis | Response options |
|---|---|
| 1. NASF-AB management | |
| Responsible/reference at NASF-AB within the scope of district management | 1 present0 absent |
| Frequent meetings between the NASF team and its reference | 1 present0 absent |
| Debate on the composition of the team to compose the NASF with the management | 1 present0 absent |
| Number of teams supported by the NASF-AB team | 1 <8 teams0 ≥8 teams |
| Diagnosis of territory to compose the team of professionals | 1 present0 absent/do not know |
| 2. Continuing education | |
| Spaces for reflection on the work process | 1 present0 absent |
| Moments of continuing education | 1 present0 absent |
| Offer suitable courses | 1 present0 absent |
| 3. Coordination of care and integration of the healthcare network | |
| Evidence of increased resolution from the NASF | 1 present0 absent |
| Frequency of contacts with professionals in the reference network | 3 always2 most of the time1 sometimes0 never |
| Frequency of network contacts with the NASF-AB regarding referred patients | 3 always2 most of the time1 sometimes0 never |
| Activities with other teams from other health services | 1 present0 absent |
| 4. Strengthening of intersectoral actions | |
| Activities with the participation of other social sectors or civil society | 1 present0 absent |
| Encouraging intersectoral practices through management | 1 present0 absent |
| 5. Qualification of care in the ESF | |
| Planning of actions based on the diagnosis of the territory | 1 present0 absent |
| Actions planned in conjunction with the family health teams | 1 present0 absent |
| Meetings to discuss work process | 1 present0 absent |
| Monitoring and analysis of work process | 1 present0 absent |
| Self-assessment in the last 12 months | 1 present0 absent |
| Definition of access criteria, flows, attributions of each professional | 1 present0 absent |
| Difficulties in locomotion to develop their activities in the territory | 0 present1 absent |
| Recording of actions in medical records with primary healthcare teams | 1 present0 absent |
| Analysis of the effectiveness of collective activities that it produces or participates in | 1 present0 absent |
| Integrated activities with family health teams | 1 present0 absent |
NASF-AB: family healthcare center (Núcleo de Atenção à Saúde da Família); ESF: family health strategy (Estratégia de Saúde da Família).
Next, the scale measuring burden of professionals in mental health services (Escala de Avaliação da Sobrecarga de Profissionais em Serviços de Saúde Mental – IMPACTO-BR) was used to assess workload, translated into Portuguese.11 The IMPACTO-BR scale has construct validity and is suitable for monitoring the quality of mental health services.12 The scale demonstrated internal consistency (α=0.84), item homogeneity and accuracy.11 The original version of the scale used for mental health services contains 34 questions. However, it was used the reduced scale adapted for the NASF-AB work for this study. Question 27 was excluded, as it did not fit the reality of the work context in family health.12
The degree of team overload was calculated using the average of 18 items which compose the scale, ranging from 1 to 5 points, and the higher the value obtained, the greater the degree of team overload. Three subscales can also be calculated: (1) overload referring to the effects felt by the team on their physical and mental health; (2) overload in relation to the impact of work on the team's functioning; and (3) emotional repercussions of the overload felt by the team.
A sociodemographic questionnaire was applied to the participants to characterize gender, age and professional composition of the teams. All questionnaires were completed electronically via Google Forms by the participants.
Staff overload was considered the study's dependent variable. Working conditions assessed using the PMAQ questionnaire were considered independent variables, as well as gender, age and profession of participants.
Sample size and statistical analysisA minimal sample size was estimated in 66 health professionals from NASF-AB in Salvador trough the OpenEpi platform (https://www.openepi.com/), considering these parameters: (i) a population of 80 health workers, (ii) a prevalence of staff overload of 34%, (iii) an alpha of 5%, (iv) confidence interval of 95% for (v) an expected effect size of 1.0.
Data on frequencies, means, medians and standard deviations were presented to characterize the participants. The Kolmogorov–Smirnov test was applied to verify whether the dependent variable (overload) had a normal distribution, which was confirmed (p>0.05). Bivariate association analyzes (simple linear regression) were performed to identify variables potentially associated with worker overload. Variables which had a p-value <0.20 were included in a multiple linear regression model. The significance level adopted in the analyzes was 5%. Data were analyzed using Statistical Package for Social Science (SPSS) version 24.0 and STATA MP version 13.0.
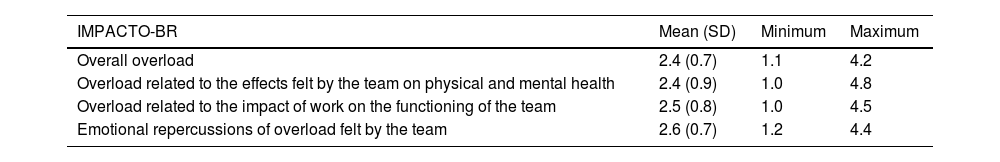
ResultsThe sample included 19 physiotherapists, 13 occupational therapists, 10 social workers, 10 nutritionists, 09 psychologists and 07 physical education professionals. Most were female (n=56; 82.4%) and the mean age was 40.5 years (SD=6.1) (non-tabulated data). As described in Table 2 the degree of overload of the NASF-AB team ranged from the mean of 2.4 (±0.7) to the mean of 2.6 (±0.7) in the IMPACTO-BR scale.
Mean and standard deviation for the degree of overload of the NASF-AB team evaluated using the IMPACTO-BR scale and its subscales.
| IMPACTO-BR | Mean (SD) | Minimum | Maximum |
|---|---|---|---|
| Overall overload | 2.4 (0.7) | 1.1 | 4.2 |
| Overload related to the effects felt by the team on physical and mental health | 2.4 (0.9) | 1.0 | 4.8 |
| Overload related to the impact of work on the functioning of the team | 2.5 (0.8) | 1.0 | 4.5 |
| Emotional repercussions of overload felt by the team | 2.6 (0.7) | 1.2 | 4.4 |
NASF-AB: family healthcare center (Núcleo de Atenção à Saúde da Família); SD: standard deviation; IMPACTO-BR: scale measuring burden of professionals in mental health services (Escala de Avaliação da Sobrecarga de Profissionais em Serviços de Saúde Mental – Brazil).
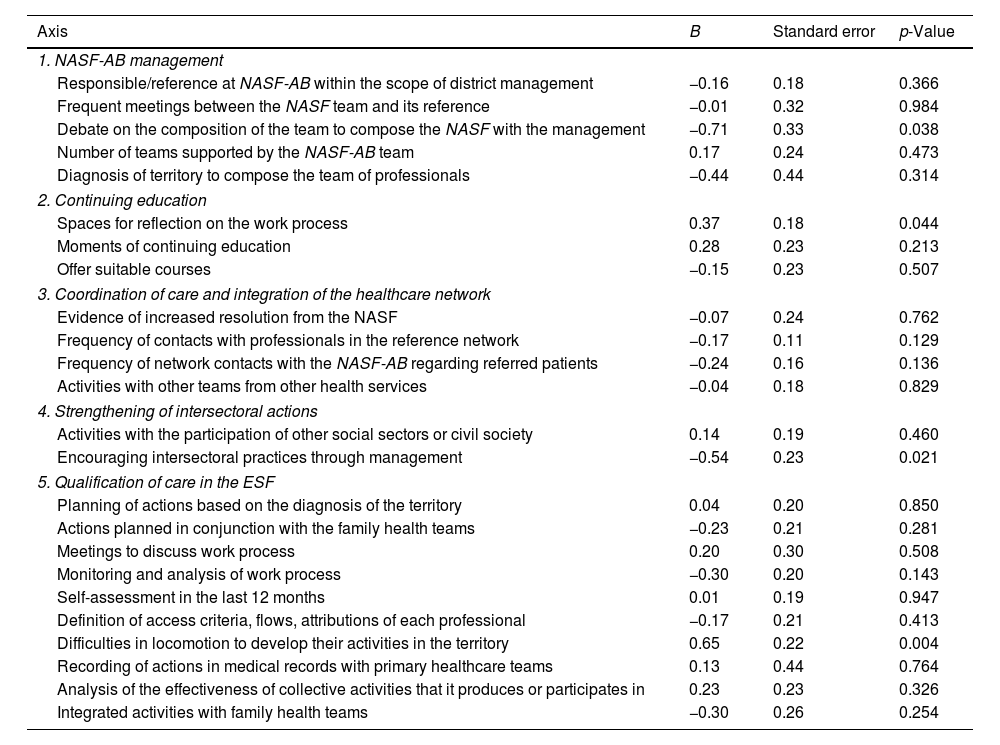
As described in Table 3 the variables of the composition of the team to compose the NASF together with the management, spaces for reflection on the work process, frequency of contacts with professionals in the reference network, frequency of contacts of the network with the NASF-AB about referred patients, stimulation of intersectoral practices through the management, monitoring and analysis of the work process and difficulties in moving around to conduct their activities in the territory are potentially associated with the overall overload of NASF workers (p<0.20). It was noted that the overall overload and the subscales have similar values, and the maximum value obtained was close to the maximum value of the scale (5 points).
Results of the bivariate analysis of the association between working conditions and workers’ overall burden.
| Axis | B | Standard error | p-Value |
|---|---|---|---|
| 1. NASF-AB management | |||
| Responsible/reference at NASF-AB within the scope of district management | −0.16 | 0.18 | 0.366 |
| Frequent meetings between the NASF team and its reference | −0.01 | 0.32 | 0.984 |
| Debate on the composition of the team to compose the NASF with the management | −0.71 | 0.33 | 0.038 |
| Number of teams supported by the NASF-AB team | 0.17 | 0.24 | 0.473 |
| Diagnosis of territory to compose the team of professionals | −0.44 | 0.44 | 0.314 |
| 2. Continuing education | |||
| Spaces for reflection on the work process | 0.37 | 0.18 | 0.044 |
| Moments of continuing education | 0.28 | 0.23 | 0.213 |
| Offer suitable courses | −0.15 | 0.23 | 0.507 |
| 3. Coordination of care and integration of the healthcare network | |||
| Evidence of increased resolution from the NASF | −0.07 | 0.24 | 0.762 |
| Frequency of contacts with professionals in the reference network | −0.17 | 0.11 | 0.129 |
| Frequency of network contacts with the NASF-AB regarding referred patients | −0.24 | 0.16 | 0.136 |
| Activities with other teams from other health services | −0.04 | 0.18 | 0.829 |
| 4. Strengthening of intersectoral actions | |||
| Activities with the participation of other social sectors or civil society | 0.14 | 0.19 | 0.460 |
| Encouraging intersectoral practices through management | −0.54 | 0.23 | 0.021 |
| 5. Qualification of care in the ESF | |||
| Planning of actions based on the diagnosis of the territory | 0.04 | 0.20 | 0.850 |
| Actions planned in conjunction with the family health teams | −0.23 | 0.21 | 0.281 |
| Meetings to discuss work process | 0.20 | 0.30 | 0.508 |
| Monitoring and analysis of work process | −0.30 | 0.20 | 0.143 |
| Self-assessment in the last 12 months | 0.01 | 0.19 | 0.947 |
| Definition of access criteria, flows, attributions of each professional | −0.17 | 0.21 | 0.413 |
| Difficulties in locomotion to develop their activities in the territory | 0.65 | 0.22 | 0.004 |
| Recording of actions in medical records with primary healthcare teams | 0.13 | 0.44 | 0.764 |
| Analysis of the effectiveness of collective activities that it produces or participates in | 0.23 | 0.23 | 0.326 |
| Integrated activities with family health teams | −0.30 | 0.26 | 0.254 |
Values in bold indicate potentially significant association (p<0.20); NASF-AB: family healthcare center (Núcleo de Atenção à Saúde da Família); ESF: family health strategy (Estratégia de Saúde da Família).
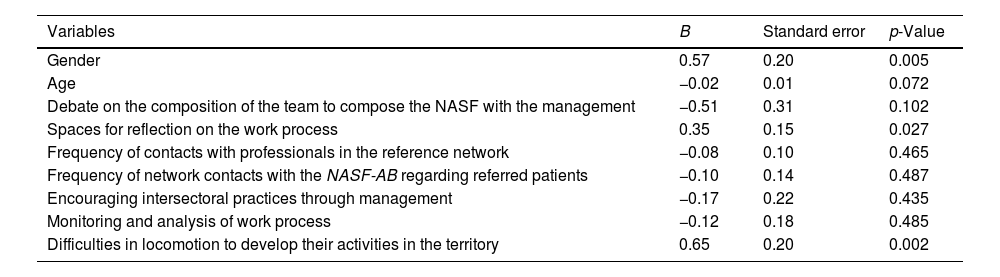
As described in Table 4, female professionals, those who reported having spaces for reflection on the work process and difficulty in moving around to conduct their activities in the territory showed more overload. The coefficient of determination obtained for multivariate regression analysis was 0.44.
Results of the multivariate analysis of the association between working conditions, gender, age and the overall overload of workers.
| Variables | B | Standard error | p-Value |
|---|---|---|---|
| Gender | 0.57 | 0.20 | 0.005 |
| Age | −0.02 | 0.01 | 0.072 |
| Debate on the composition of the team to compose the NASF with the management | −0.51 | 0.31 | 0.102 |
| Spaces for reflection on the work process | 0.35 | 0.15 | 0.027 |
| Frequency of contacts with professionals in the reference network | −0.08 | 0.10 | 0.465 |
| Frequency of network contacts with the NASF-AB regarding referred patients | −0.10 | 0.14 | 0.487 |
| Encouraging intersectoral practices through management | −0.17 | 0.22 | 0.435 |
| Monitoring and analysis of work process | −0.12 | 0.18 | 0.485 |
| Difficulties in locomotion to develop their activities in the territory | 0.65 | 0.20 | 0.002 |
NASF-AB: family healthcare center (Núcleo de Atenção à Saúde da Família).
It was identified that gender, having spaces for reflection on the work process and the difficulty of moving around to conduct activities were the factors associated with the overload of NASF-AB workers according to the multivariate analysis.
The overload associated with gender in this study was in line with the other studies conducted during the COVID-19 pandemic, in which female workers were at great risk to psychological distress.13,14 It is possible to infer that the space of care, even with the transition from common sense to scientific knowledge carried out over the years, was and is mostly composed by females, as observed in this study. The double responsibility of women (domestic and work) also increases their physical load and reduces rest time, leading to adverse effects15 and psychological distress. The stress caused by work against COVID-19 could increase the overload and affect the general health conditions of these workers.16,17
This work by the multidisciplinary group presupposes work with the different dimensions of the social determinants of health and encompasses a series of knowledge centers in constant mutation; a movement which workers need to do at all times to draw up community and specific health plans and that need constant adjustment, thereby generating daily stress.18,19
All of these obvious changes promoted to contain/stop the proliferation and contamination of the SARS-COV2 virus in the population greatly marked health professionals, configuring in (overall) work overload, occupational stress, a decrease in activities that enhance leisure and satisfaction and may have boosted the feeling of overload in frontline health workers, including in the context of the NASF-AB.1,20
This can occur through inadequate supply of work inputs, sanitary transport and weakening of communication between the NASF-AB team, FH team and management. These inadequate working conditions interfere with the working conditions of the NASF-AB and FH team, alter the resolution of actions and present themselves as barriers to conclude articulated practices between these teams.21
A possible alternative would be a work proposal that promotes reorientations of the practices of these teams to make them more integrated,21 and in the reorientations of practices which, in short, require new political positions by management, for example: reduction in the number of teams supported, expansion of continuing education for primary healthcare, better organization and work management, among others.21 As suggestion for a better organization of the management of the practice in the primary healthcare, a Spanish study22 pointed out an electronic appointment system implemented during the period of the COVID-19 pandemic. The acceptance of the population was around 85%, which enhanced the primary healthcare organization.22
However, it is observed that a mitigating posture of the SUS can occur under different causes, from the lack of material and human inputs, and even prioritizing actions centered on the quantitative of procedures. The findings of this study are consistent with those found by Lancman et al.,5 in which it is observed that unfavorable working conditions, such as lack of input, lack of materials for work, limitation of outpatient room, in addition to making it difficult to perform the work itself, become relationship barriers between the teams and between these and management.
These issues are also endorsed by the lack of the safety care observed in another Brazilian study23 that analyzed the relationship between job satisfaction and psychosocial symptoms related to work in hospital health workers. Despite the fragilities observed in the work environment, these professionals were able to disseminate a safety of culture among patients when they feel safe at work. According to the authors23 work overload and inadequate management of the system are factors against the ideal perception of safety culture and safety care.
Therefore, it can be extended to the results of this study. Such fragility can have repercussions and even be a reflection of the non-protagonism of management, and to some degree it may represent non-prioritization of NASF-AB activities, since communication is a crucial element for the performance of primary care.21 The scenario is composed of a lack of dialog and lack of prioritization of actions by management.
The overall overload in the spaces for reflection can also be expressed through the difficulty in establishing assertive communication between the members of the NASF-AB team and the FH teams, and therefore the emergence of existing conflict between these teams. It turns out that the lack of protagonism of the management to mitigate the existing conflicts can be a way to make the discourse reverberate that the family health strategy itself does not fulfill its objectives.
Due to all these difficulties, and others studied, as well as the disarticulation of the NASF-AB team with the FH team and local management21 also point to a fragmented work process when studying a municipality in Bahia. This difficulty in articulating the work actions themselves was also reported by Lancman et al.5 when analyzing the work process of the NASF-AB team in São Paulo, as they report that the teams made the communication process and relationship difficult, and this factor increased the dissatisfaction and the feeling of overload of the NASF-AB professionals with the work produced.
Several authors21,24,25 endorse these findings when referring that communication at work can be an important point for interpersonal relationships and the effectiveness of workers’ actions. Even when considering the panorama of Brazilian society in which there is aging, as well as the progression of chronic-degenerative diseases, the need to implement health actions is perceived in an integral and multifaceted way3 especially with regard to the execution of family health care activities and the NASF-AB with the premise of matrix support and preventive activities.25 It turns out that relevant skills for effectively carrying out these actions presuppose interprofessional activities, meaning collaborative activities, which in turn impute the need for adequate communication and agreement to resolve the actions of the services.25
Faced with a service whose organization is fragmented and with a communication deficit between the management and the family health and NASF-AB teams, as well as non-prioritized actions of these teams by the management, this can lead to repercussions on a lower response capacity to the health demands of that locality, in dissatisfaction for the workers present there, and in turn their feeling of grief and overload as well. Added to this situation, the COVID-19 Pandemic scenario, in which not only the recurrent weaknesses were exposed, but in which it was necessary to gather extra strength to find answers to the health problem now presented.
In view of the context of extreme social inequality, the potential for contamination of low-income populations, making these pandemic signs even more alarming, and which we believe are capable of promoting overload on workers.1,26–28 This in turn brings to light the relevance of the work of PHC and even the NASF-AB, emerging on the front line for controlling and overcoming the pandemic. Therefore, the pandemic has potentiated these chronic and structural problems which in turn may have reverberated in the revictimized feeling of overload among workers and intensified the cycle/speech of precariousness of public services. This study presented results that have a direct impact on work relationships and workers’ health. More studies are recommended to strength the associations observed in this study, particularly considering the medium- and long-term impacts of the pandemic.
Ethical approval and consent to participateThe study followed all ethical recommendations for research with human beings according to the Declaration of Helsinki and was duly approved by the Ethics Committee for Research with Human Beings of the State University of Bahia (CEP/UNEB), with number CAEE no. 39364120.3.0000.0057. All participants signed the informed consent form (ICF) prior to data collection.
FundingNo funding was received for conducting this study.
Authors’ contributionsCCFL and JLCN contributed to the study conception and design. Material preparation and data collection were performed by CCFL. Data analysis were performed by CCFL, JLCN, TdeOS and HMSFM. The first draft of the manuscript was written by CCFL and JLCN and all authors commented on previous of the manuscript. All authors read and approved the final manuscript.
Consent for publicationNot applicable.
Competing interestsThe authors declare that they have no competing interests.
Data availabilityThe data to support the findings of this study are available upon reasonable request from the corresponding author. Restrictions apply to the availability of the data, due to the sample and information gathered.
The authors thank the workers for participated in this study.