The use of devices that provide continuous positive pressure in the airway has shown improvement in various pathologies that cause respiratory failure. In the COVID 19 pandemic episode the use of these devices has become widespread, but, due to the shortage of conventional CPAP devices, alternative devices have been manufactured. The objective of this study is to describe the use of these devices, as well as their efficacy.
Material and methodsData are collected from patients admitted for Pneumonia due to COVID 19 at the IFEMA Field Hospital. Data are collected from 23 patients with respiratory failure and need for ventilatory support.
ResultsStudy carried out on a total of 23 patients, dated admission to IFEMA. Alternative CPAP was used in five patients (21.7%), while ventilatory support with a reservoir mask or Ventimask Venturi effect was used in the remaining 18 patients (78.3%). A progressive increase in saturation is observed in those patients in whom alternative CPAP was used (from 94% on average to 98% and 99% on average after 30 and 60 min with the mask, respectively), although this change was not significant (p = 0.058 and p = 0.122 respectively). No significant change in RF was observed at the beginning and end of the measurement in patients who used alternative CPAP (p = 0.423), but among those who did not use alternative CPAP (p = 0.001). A statistically significant improvement in the variable oxygen saturation / fraction inspired by oxygen is observed in patients who used alternative CPAP (p = 0.040)
ConclusionThe use of these devices has helped the ventilatory work of several patients by improving their oxygenation parameters. To better observe the evolution of patients undergoing this therapy and compare them with patients with other types of ventilatory support, further studies are necessary.
El uso de dispositivos que aportan presión positiva continua en la vía aérea ha demostrado mejoría en diversas patologías que producen insuficiencia respiratoria. En el episodio de pandemia por COVID 19 el uso de estos dispositivos se ha generalizado, pero, debido a la escasez de dispositivos convencionales de CPAP, se han fabricado dispositivos alternativos. El objetivo de este estudio es describir el uso de estos dispositivos, así como su eficacia.
Material y métodosSe recogen datos de pacientes ingresados por Neumonía por COVID 19 en el Hospital de campaña de IFEMA. Se recogen datos de pacientes con insuficiencia respiratoria y necesidad de soporte ventilatorio.
ResultadosEstudio realizado sobre un total de 23 pacientes, con fecha ingreso en IFEMA. Se empleó CPAP alternativa en cinco pacientes (21,7%), mientras que en los 18 pacientes restantes (78,3%) se usó soporte ventilatorio con mascarilla reservorio o Ventimask efecto Venturi. Se observa un aumento progresivo de la saturación en aquellos pacientes en los que se empleó CPAP alternativa (de 94% de promedio a 98% y 99% de promedio tras 30 y 60 minutos con la máscara, respectivamente), aunque este cambio no resultó significativo (p = 0,058 y p = 0,122 respectivamente). No se observó un cambio significativo de frecuencia respiratoria al inicio y final de la medición en pacientes que usaron CPAP alternativa (p = 0,423) pero si entre los que no la usaron (p = 0,001). Se observa una mejoría estadísticamente significativa en la variable Saturación de oxigeno / Fracción inspirado de oxígeno en los pacientes que usaron CPAP alternativa (p = 0,040)
ConclusiónEl uso de estos dispositivos ha ayudado al trabajo ventilatorio de varios pacientes mejorando sus parámetros de oxigenación. Para observar mejor la evolución de los pacientes sometidos a esta terapia y compararlos con pacientes con otro tipo de soporte ventilatorio, son necesarios más estudios en los que se aleatorice su uso.
Applying continuous positive airway pressure (CPAP) results in the deployment or recruitment of partially or totally collapsed alveolar units, improves lung compliance, and increases transpulmonary pressure and functional residual capacity. This implies improved respiration, as well as gas exchange.1 At the haemodynamic level, applying CPAP results in decreased pre-load and post-load (by reducing venous return and left ventricular wall systolic pressure), with a slight decrease in systolic blood pressure and cardiac output in patients with normal heart function. In patients suffering from heart failure with increased pulmonary capillary pressure and hypervolaemia, the cardiac output may increase.2 When CPAP is compared to conventional oxygenation systems, it shows a significant reduction in the need for intubation (50-60%) as well as lower in-hospital mortality (40-47%), and it is considered the oxygen therapy system of choice for many pathologies.3 Recently, a study4 suggested that the use of a CPAP device would limit the spread of the virus into the room air. Its use has also been indicated to avoid or delay admission to the intensive care unit (ICU)5 and various publications have reported the usefulness of CPAP in acute lung oedema6–8 and its application in the emergency department.9
The European Society for Intensive Care Medicine has recommended the use of CPAP in patients with acute respiratory failure due to COVID-19.10,11 However, during the COVID-19 pandemic when the healthcare system has been under extreme demand, there have been times when there have not been enough conventional CPAP systems available on the market to treat these patients. To ensure ventilatory support to patients with acute respiratory failure secondary to COVID-19, various alternative systems were developed that were capable of producing CPAP.
The devices in use have been modified throughout this opening gambit against the disease. The most popular alternative devices were developed by professionals from the ICUs of the Príncipe de Asturias University Hospital and the Henares University Hospital. The elements used for their assembly are similar, namely:
- 1
Positive End-Expiratory Pressure (PEEP) valve
- 2
Antibacterial and antiviral filter
- 3
Dual-limb breathing bag
- 4
Conventional oxygen intake tube
- 5
Mask (Ventimask with closed vents, conventional CPAP interface or Decathlon diving mask©)
Figs. 1 and 2, show how the elements are assembled.
In the case of the first device, the T-piece connecting the various elements is manufactured with 3 D printers, specifically designed for this device. Manufacturing has been carried out by Hewlett Packard®.
The objective of this study is to verify the efficacy of these devices in the clinical and respiratory status of the patients to whom they are applied. Our hypothesis is that the use of these alternative devices improves the patient's ventilatory status more quickly than conventional oxygen therapy.
Material and methodsType of studyIt is a descriptive observational study in which clinical-epidemiological data are collected from patients of legal age who were treated at the IFEMA Field Hospital, with an admission date between 24 March and 28 April, for pneumonia due to SARS CoV-2 and who developed respiratory failure (oxygen saturation [SatO2] < 93 and oxygen saturation/fraction of inspired oxygen [SatO2/FiO2] < 300), and who required the use of a reservoir mask or a Venturi effect Ventimask, as well as alternative CPAP devices. The following variables were collected:
- -
Age
- -
Sex
- -
Comorbidity (obesity, chronic obstructive pulmonary disease [COPD], asthma, neuromuscular disease, arterial hypertension [HT], ischemic heart disease) and pulmonary thromboembolism (PTE).
- -
Time of evolution of the disease (days from the onset of symptoms)
- -
Type of alternative CPAP device prescribed
- -
Medication for COVID and time in days from the start of the same:
- o
lopinavir/ritonavir
- o
chloroquine
- o
azithromycin
- o
IL-6
- o
corticosteroids
- o
tocilizumab
- o
anakinra
- o
heparin
- o
other
- -
SatO2/FiO2 at the start of therapy
- -
SatO2 every hour after the start of therapy
- -
Respiratory rate (RR) at the start of therapy
- -
RR every hour after therapy
- -
Need for admission to ICU
No data were collected from patients with clinical circumstances that prevented the correct assessment of the use of these devices, such as:
- -
Unable to protect the airway: patient in a coma or agitated
- -
Recent gastrointestinal or upper airway surgery (<15 days), uncontrolled vomiting and active upper gastrointestinal bleeding (UGIB)
- -
Inability to control secretions
- -
Hemodynamic instability (established shock not controlled with vasoactive fluids and/or drugs) or uncontrolled malignant arrhythmia
- -
Seizure crisis
- -
Impossible to attach the mask
- -
Lack of knowledge of the technique
The compilation of the variables was obtained from the computer system where the patient clinical records were logged. There was no clear directive for the use of the alternative CPAP. It was used in cases of respiratory failure refractory to conventional oxygen therapy with a partial pressure of oxygen index (PaO2)/RR lower than 150.
Analysis of dataPatients were divided into two groups: those who were given conventional oxygen therapy exclusively; and those who were given alternative CPAP. The possible association between the patient characteristics (demographic data, risk factors, and drug treatment) and the use of alternative CPAP was studied using Pearson's chi-square test and/or Fisher's exact test, while possible differences in terms of biochemical parameters were analysed with the Student's t-test. The abovementioned analyses were carried out with the SPSS V.20 program (IBM Inc., Chicago, Il., USA), and statistically significant associations/differences were considered to exist when the p-value was below 0.05.
Furthermore, linear regression was used to compare the changes (difference between the initial and final values after the use of oxygen therapy) of SatO2, RR and the oxygen saturation analysis (SpO2)/FiO2 among patients who used CPAP and those who did not use this alternative. For this, the R lme4 package, version 3.4 (RCoreTeam, 2017) was used.12
Informed consentAll patients who met the inclusion criteria and agreed to participate in the study filled out an informed consent form. Said document collected the most important information of the study about the patient, the possible adverse effects, confidentiality and the right to withdraw at any time.
The study has received a positive opinion from the Clinical Research and Ethics Committee of the San Carlos Clinical University Hospital.
ResultsDescriptive analysisA total of 23 patients were recruited. 52.2% (n = 12) were males, and the sex of one patient was not available. The mean age was 63 years (standard deviation [SD] = 11.3), the youngest patient was 44 years old and the oldest patient was 85 years old.
The personal history of the patients was as follows: 52.2% (n = 12) had arterial hypertension, 13.0% (n = 3) had diabetes mellitus, 26.1% (n = 6) were obese, only 8.7% (n = 2) suffered from ischemic heart disease, 21.7% (n = 5) chronic kidney disease, 13% (n = 3) were smokers and 26.1% (n = 6) suffered from lung disease, this being, specifically, asthma in four patients, COPD in two, and obstructive sleep apnea syndrome (OSAS) in one patient.
The onset of symptoms in all recruited patients was between 16 March and 12 April.
The mean values of the biochemical parameters (and SD) were the following: D-dimer = 2,053 ng/dL (3,178.8); IL-6 = 29.3 pg/mL (21.0); ferritin = 1,052 µg/L (537.7).
The medicinal products used as treatment for COVID-19 were the following: hydroxychloroquine for 100% study patients; lopinavir/ritonavir 56.5% (n = 13); tocilizumab 60.9% (n = 14); corticosteroids 95.7% (n = 22); antibiotics were azithromycin in 82.6% (n = 19) and ceftriaxone in 13.0% (n = 3).
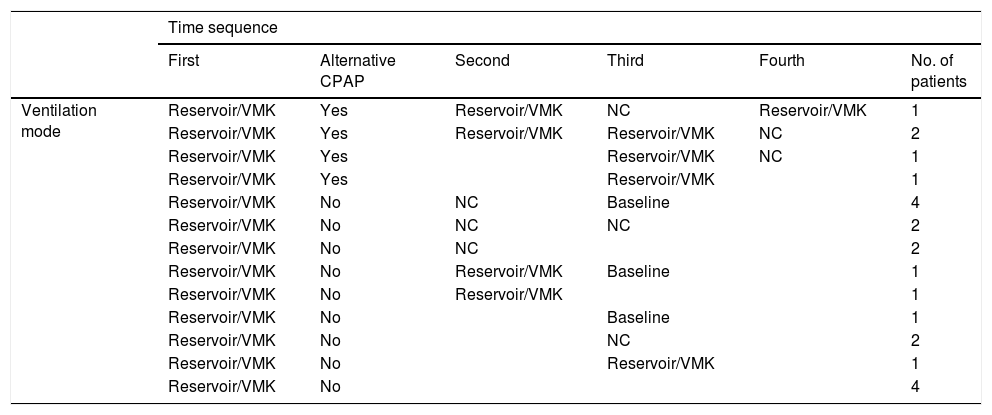
Alternative CPAP was used in five patients (21.7%), but was not used in the other 18 (78.3%). Table 1 shows the temporal sequence of the ventilatory support of the recruited patients.
Sequence of the use of the different ventilation modes in patients admitted to IFEMA and under study.
| Time sequence | ||||||
|---|---|---|---|---|---|---|
| First | Alternative CPAP | Second | Third | Fourth | No. of patients | |
| Ventilation mode | Reservoir/VMK | Yes | Reservoir/VMK | NC | Reservoir/VMK | 1 |
| Reservoir/VMK | Yes | Reservoir/VMK | Reservoir/VMK | NC | 2 | |
| Reservoir/VMK | Yes | Reservoir/VMK | NC | 1 | ||
| Reservoir/VMK | Yes | Reservoir/VMK | 1 | |||
| Reservoir/VMK | No | NC | Baseline | 4 | ||
| Reservoir/VMK | No | NC | NC | 2 | ||
| Reservoir/VMK | No | NC | 2 | |||
| Reservoir/VMK | No | Reservoir/VMK | Baseline | 1 | ||
| Reservoir/VMK | No | Reservoir/VMK | 1 | |||
| Reservoir/VMK | No | Baseline | 1 | |||
| Reservoir/VMK | No | NC | 2 | |||
| Reservoir/VMK | No | Reservoir/VMK | 1 | |||
| Reservoir/VMK | No | 4 | ||||
CPAP: continuous positive airway pressure; NC: nasal cannula; VMK: Ventimask.
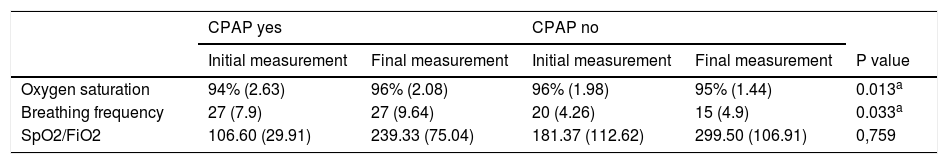
The overall mean initial SatO2 was 96% (2.25). The SatO2 prior to the use of CPAP in the patients in whom this alternative was used, was two percentage units lower (95% CI between -0.13 and 4.75) than the initial saturation registered in the rest of the patients (Table 2).
Initial and final measurements (mean and standard deviation) of oxygen saturation, respiratory rate and SpO2/FiO2 obtained in patients with CPAP and those who used other oxygen therapy, and the p-value obtained from the comparison of the evolution of these values in both groups by linear regression.
| CPAP yes | CPAP no | ||||
|---|---|---|---|---|---|
| Initial measurement | Final measurement | Initial measurement | Final measurement | P value | |
| Oxygen saturation | 94% (2.63) | 96% (2.08) | 96% (1.98) | 95% (1.44) | 0.013a |
| Breathing frequency | 27 (7.9) | 27 (9.64) | 20 (4.26) | 15 (4.9) | 0.033a |
| SpO2/FiO2 | 106.60 (29.91) | 239.33 (75.04) | 181.37 (112.62) | 299.50 (106.91) | 0,759 |
CPAP: continuous positive airway pressure; SpO2/FiO2: analysis of oxygen saturation/fraction of inspired oxygen.
A progressive increase in SatO2 was observed in those patients in whom alternative CPAP was used, from an initial average of 94% to a mean saturation of 98 and 99% after 30 and 60 min, respectively. After removal of the device, the mean saturation of these patients was 96% (2.08), while that recorded at the same time in non-CPAP patients was 95% (1.44), with the increase achieved with CPAP being significantly higher (p = 0.013).
Analysis of respiratory rateThe overall mean initial RR was 22 rpm (5.51). The CPAP group was seven units (95% CI between 0.1 and 12.0) higher than that registered in patients who did not go on to receive this alternative (Table 2).
After the use of the CPAP, the RR remained at values similar to the initial values (final mean =27 rpm, SD = 9.64), while the RR registered in the rest of the patients who did not go on to receive this alternative decreased to a mean of 15 rpm (p = 0.033) (Table 2).
SpO2/FiO2 analysisThe overall baseline SpO2/FiO2 was 164.38 (104.22). The CPAP group was 74.8 units (95% CI between 11.3 and 138.2), so it was lower than that registered in patients who did not go on to receive this alternative (Table 2). After the use of CPAP, the mean SpO2/FiO2 went up to 186.73 units, reaching a final value of 293.33 (75.04), similar to that reached in the rest of the patients who did not go on to receive the alternative (mean = 299.50, SD = 106.91), so both approaches were equally useful in restoring SpO2/FiO2 (p = 0.759) (Table 2).
Analysis of other variablesOne patient had a sensation of moderate dyspnea and two had mild dyspnea prior to being given the alternative CPAP, and the other two patients who used CPAP did not report a sensation of dyspnea.
The CPAP used in all cases had a valve in the lower part (alternative CPAP type A) and the PEEP averaged 9.50 cm H2O, with an SD of 1.12; mask tolerance was good in all five cases and, none of the patients with alternative CPAP required the administration of opioids.
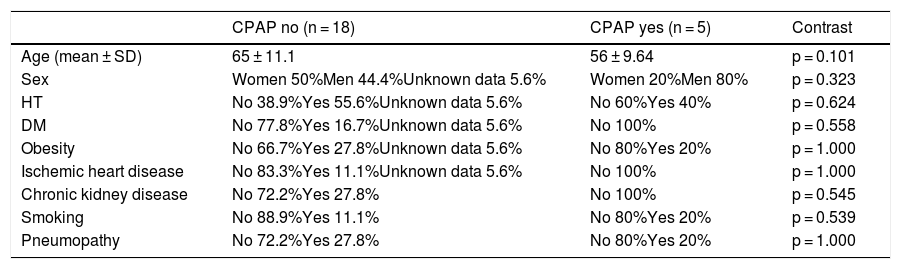
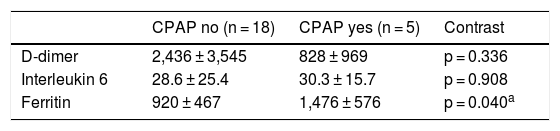
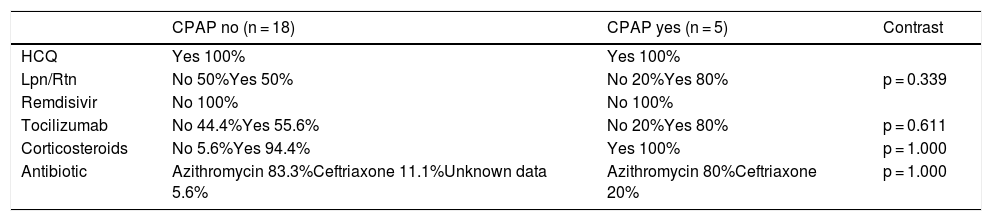
We found no significant differences in relation to the personal history between patients who received alternative CPAP and those who did not (Table 3). On the other hand, an association was observed between patients with high ferritin levels and the use of the alternative CPAP (Table 4). No association between the drugs used to treat the infection and the need for alternative ventilatory support was found (Table 5).
Comparison of patient characteristics in the CPAP group, and the group that did not use this alternative.
| CPAP no (n = 18) | CPAP yes (n = 5) | Contrast | |
|---|---|---|---|
| Age (mean ± SD) | 65 ± 11.1 | 56 ± 9.64 | p = 0.101 |
| Sex | Women 50%Men 44.4%Unknown data 5.6% | Women 20%Men 80% | p = 0.323 |
| HT | No 38.9%Yes 55.6%Unknown data 5.6% | No 60%Yes 40% | p = 0.624 |
| DM | No 77.8%Yes 16.7%Unknown data 5.6% | No 100% | p = 0.558 |
| Obesity | No 66.7%Yes 27.8%Unknown data 5.6% | No 80%Yes 20% | p = 1.000 |
| Ischemic heart disease | No 83.3%Yes 11.1%Unknown data 5.6% | No 100% | p = 1.000 |
| Chronic kidney disease | No 72.2%Yes 27.8% | No 100% | p = 0.545 |
| Smoking | No 88.9%Yes 11.1% | No 80%Yes 20% | p = 0.539 |
| Pneumopathy | No 72.2%Yes 27.8% | No 80%Yes 20% | p = 1.000 |
CPAP: continuous positive airway pressure; SD: standard deviation; DM: diabetes mellitus; HT: arterial hypertension.
Biochemical parameters (mean ± SD).
| CPAP no (n = 18) | CPAP yes (n = 5) | Contrast | |
|---|---|---|---|
| D-dimer | 2,436 ± 3,545 | 828 ± 969 | p = 0.336 |
| Interleukin 6 | 28.6 ± 25.4 | 30.3 ± 15.7 | p = 0.908 |
| Ferritin | 920 ± 467 | 1,476 ± 576 | p = 0.040a |
CPAP: continuous positive airway pressure; SD: standard deviation.
Treatment of SARS-CoV-2.
| CPAP no (n = 18) | CPAP yes (n = 5) | Contrast | |
|---|---|---|---|
| HCQ | Yes 100% | Yes 100% | |
| Lpn/Rtn | No 50%Yes 50% | No 20%Yes 80% | p = 0.339 |
| Remdisivir | No 100% | No 100% | |
| Tocilizumab | No 44.4%Yes 55.6% | No 20%Yes 80% | p = 0.611 |
| Corticosteroids | No 5.6%Yes 94.4% | Yes 100% | p = 1.000 |
| Antibiotic | Azithromycin 83.3%Ceftriaxone 11.1%Unknown data 5.6% | Azithromycin 80%Ceftriaxone 20% | p = 1.000 |
CPAP: continuous positive airway pressure; HCQ: hydroxychloroquine; Lpn / Rtn: lopinavir / ritonavir.
Based on our data, it appears that the use of the alternative CPAP improves the ventilatory status of patients with respiratory failure refractory to conventional oxygen therapy. In patients with acute respiratory distress syndrome, heterogeneity in the filling of the lung parenchyma leads to the appearance of both distended and collapsed areas. Protective ventilation strategies based on the use of low volumes have shown, in this context, an increase in survival. To distend the lung, in addition to using the PEEP, recruitment manoeuvres are used, although this is still under debate.13 To develop this PEEP, the use of non-invasive mechanical ventilation is ideal.9 However, the high number of patients with severe respiratory failure and the lack of non-invasive ventilation devices imposed the use of alternative CPAPs that were capable of producing this PEEP.
A priori, the patients who were given the CPAP did not have a different saturation than the rest. In the case series, it is observed that these devices were indicated for respiratory work, because the initial saturation levels were similar in both groups, but the respiratory rate differed, being much higher in the alternative CPAP group prior to its use. Even so, after a while, the SatO2 increased in the alternative CPAP group and decreased in the other group, contrary to the respiratory rate that remained on a similar level.
If we unite the SatO2/FiO2 variables, it is seen that there is significant improvement in the patients who were given the alternative CPAP. The usefulness of SatO2/FiO2 is comparable to PaO2/FiO2 (PAFi) for the diagnosis of respiratory distress.14,15 SpO2/FiO2 has proved to be comparable to PAFi in patients with ventilatory function deterioration and can be a reliable indicator of the need for escalating the ventilatory support. Patients with a relationship between the SatO2 and an FiO2 lower than 100 or 200 should be candidates for this type of therapy.
Another interesting fact is that no relationship was found between the use of ventilatory support and previous pathologies. If we look for a relationship in the laboratory levels of the patients whose ventilatory levels were worst, we find only one association, namely ferritin. Higher ferritin values prove to have a worse prognosis, as shown by other recently published studies.16
The most important limitations of the study are that the sample size was reduced due to the closure of the field hospital, and the heterogeneity in the retrospective data collection as dynamic changes were made in the hospital every day.
The use of these devices has helped to reduce the ventilatory work of several patients, improving their oxygenation parameters. More studies are needed to better observe the evolution of patients undergoing this therapy and to compare them with patients given another type of ventilatory support. The use of devices invented "on the fly" by healthcare professionals has been the result of well-understood improvisation and the need to adapt to the times we are living through. Recent articles17 have shown the same difficulties we encountered, and which have been overcome thanks to the contribution of many professionals from different healthcare levels. This is one more example of everything that has happened in recent weeks.
FundingThis article has not received funding.
Conflict of interestsThe authors declare that they have no conflict of interest.
Thanks toDr Federico Gordo of the HU Henares and Dr María Trascasa of the HU Príncipe de Asturias, and their teams, for sharing their alternative CPAP innovations with the IFEMA Field Hospital.
Please cite this article as: Mateos-Rodríguez A, Ortega-Anselmi J, Candel-González FJ, Canora-Lebrato J, Fragiel-Saavedra M, Hernández-Píriz A, et al. Métodos alternativos de CPAP para el tratamiento de insuficiencia respiratoria grave secundaria a neumonía por COVID-19. Med Clin (Barc). 2021;156:55–60.