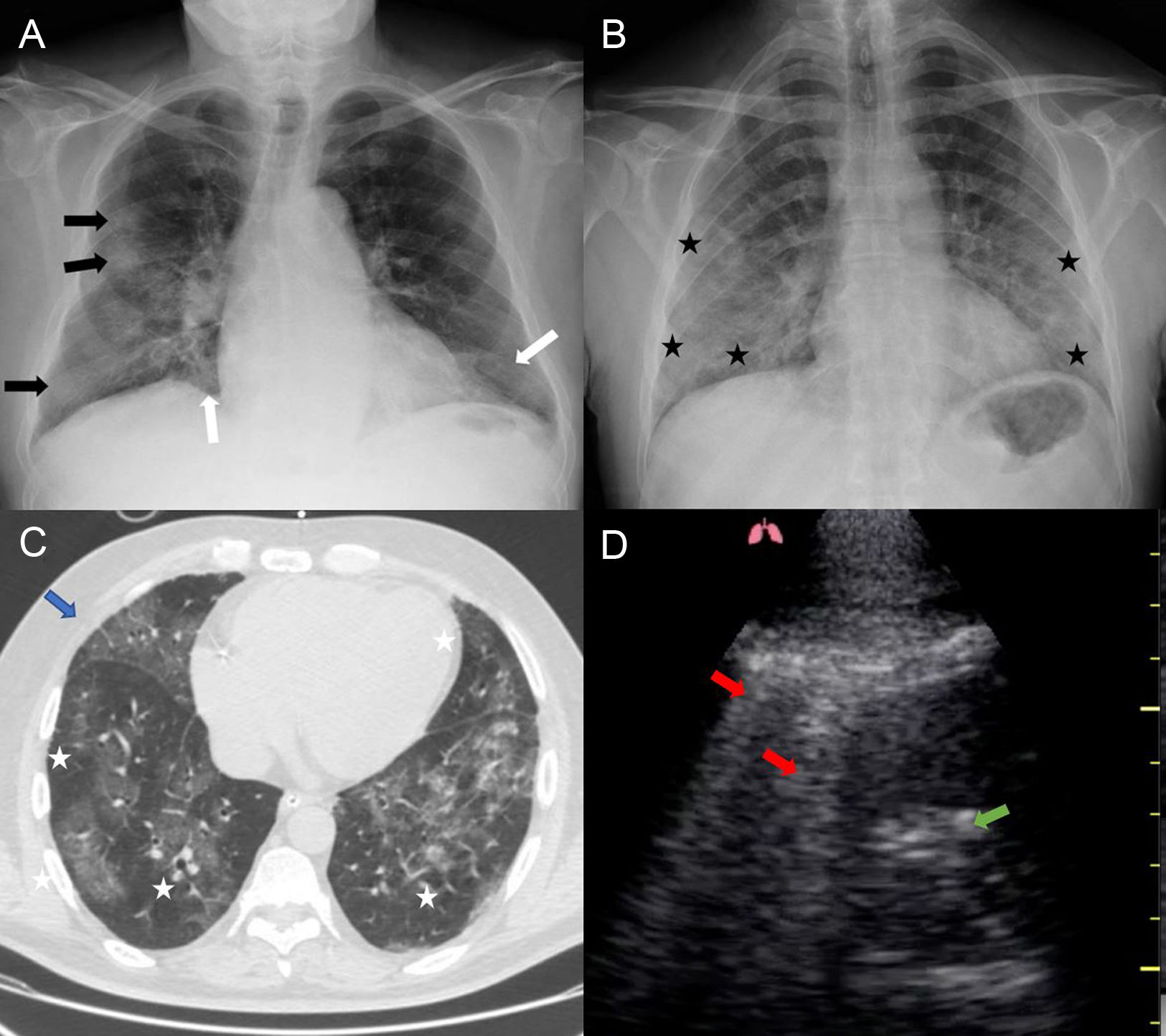
Radiological findings are of vital importance in the diagnosis of the SARS-CoV-2 coronavirus (COVID-19) due to the high rate of false negatives generated through microbiology. Below we describe the radiological characteristics shown by different patients:
Fig. 1A and B correspond to chest X-rays belonging to an 87-year-old male, afebrile, with dyspnoea and dry cough, positive PCR (Fig. 1A); and a 53-year-old male who presented with fever, cough and dyspnoea. Negative PCR with COVID-19 positive IgM and IgG antibodies (Fig. 1B). This test is the first imaging test to be performed, it is characterized by presenting patchy alveolar-interstitial opacities (black arrows) and diffuse (white arrows), with predominantly peripheral involvement and lung bases (black asterisks); keeping the hilar region intact in the initial stages.
The computed tomography (Fig. 1C) performed on a 55-year-old male who presented with dyspnoea and positive PCR shows diffuse density increases with a predominantly peripheral bilateral distribution “ground-glass” pattern (white asterisks), they tend to confluence (blue arrow), with greater involvement at lung bases. In early stages it tends to be patched although it can develop to confluence and consolidation (blue arrow). interlobular septal thickenings or bronchiectasis can be observed in later stages. Consolidation without “ground-glass”, cavitation, pleural effusion, and lymphadenopathy should make us suspect of another disease.
Ultrasonography (Fig. 1D) is proposed as an alternative for the diagnosis and monitoring of COVID-19, with greater sensitivity than X-ray, but low specificity, as it is the case with a 35-year-old male with a 3-day history of fever, X-ray without abnormalities. The most common findings are thickening and irregularity of the pleural line, diffuse B lines (red arrow) and consolidations (green arrow), with pleural effusion not being common in these patients.
FundingThe authors declare that they have not received funding to carry out this study.
Please cite this article as: López Zúñiga D, López Zúñiga MÁ. El diagnóstico COVID-19 a través de la imagen. Med Clin (Barc). 2020;155:140.