To prospectively compare the accuracy in initial staging and end-of-treatment restaging of diffuse large B-cell lymphoma (DLBCL) between 64-slice multidetector computed tomography (64MDCT) and 18FDG positron emission tomography/computed tomography (18FGD PET/CT) with intravenous contrast injection.
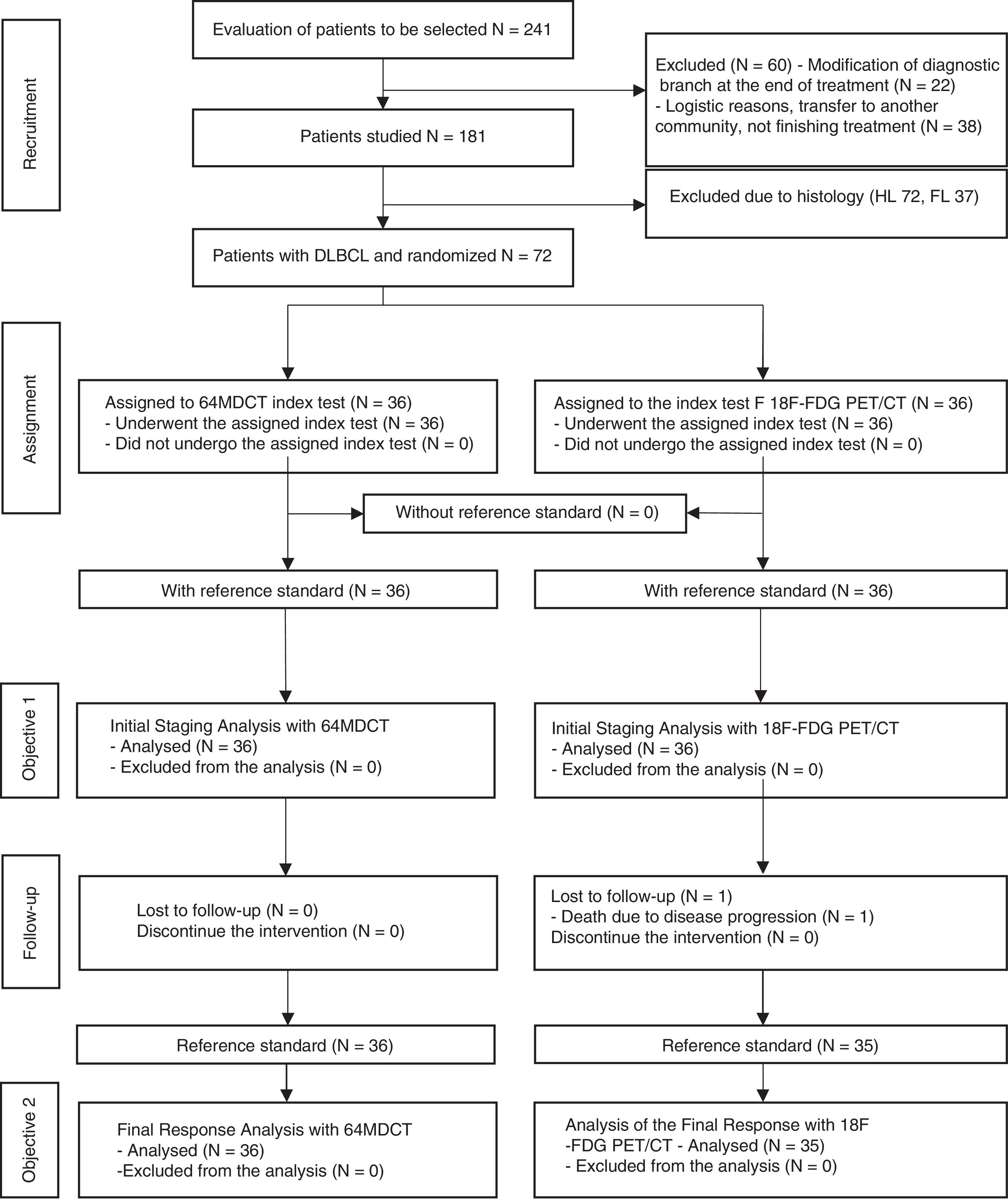
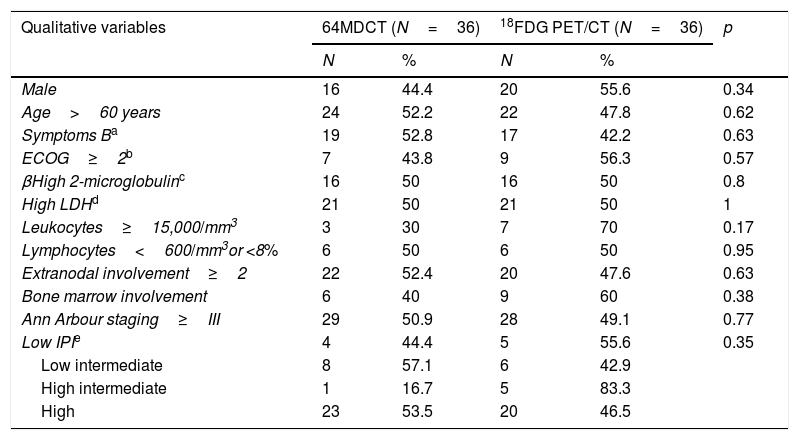
Material and methodsRandomized and blind controlled clinical multicentric trial that included biopsy-proven DLBCL patients. Seventy-two patients from five different hospitals in the region of Madrid, Spain, were enrolled in the study between January 2012 and June 2015. Thirty-six were randomly allocated to 18FDG PET/TC and the other 36–64MDCT for initial staging and end-of-treatment restaging. A nuclear medicine physician and a radiologist independently analyzed 18FDG PET/TC images and reached an agreement post hoc. 64MDCT images were separately evaluated by a different radiologist. Every set of images was compared to the reference standard that included clinical data, complementary tests and follow-up. The study was approved by participating centres’ ethics committees and written informed consent was obtained from all the participants.
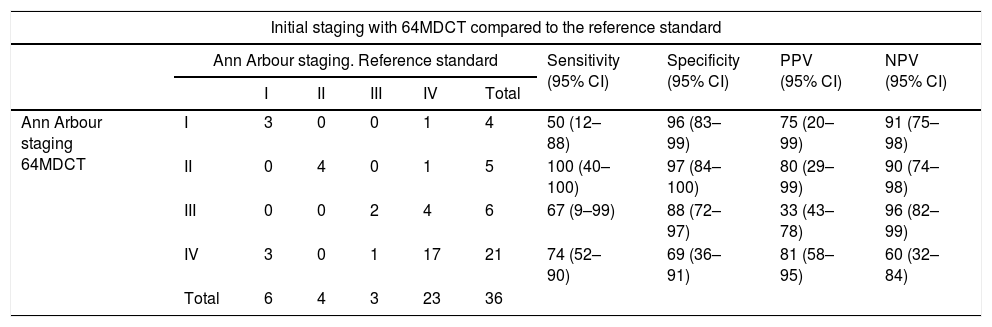
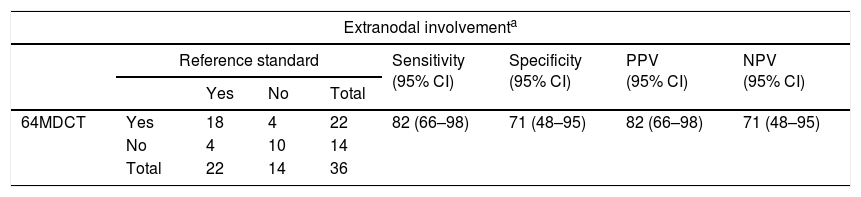
ResultsA good agreement was observed between both diagnostic techniques and the reference standard in initial staging [18FDG PET/CT (k=0.5) and 64MDCT (k=0.6)], although only the 18FDG PET/TC showed a good agreement with the reference standard for the end-of-treatment restaging (k=0.7).
ConclusionIn DLBCL, both 18FDG PET/TC and 64MDCT have shown good agreement with the reference standard in initial staging. Nevertheless, 18FDG PET/CT has shown to be superior to 64MDCT in end-of-treatment response assessment.
Comparar prospectivamente la exactitud diagnóstica de la tomografía computarizada de 64 detectores (TCMD64) y la tomografía por emisión de positrones/tomografía computarizada (18FDG PET/TC) con contraste intravenoso en pacientes con linfoma difuso de células grandes B (LDCGB) en la estadificación inicial y en la evaluación de la respuesta al final del tratamiento.
Material y métodosEnsayo clínico controlado multicéntrico que incluyó 72 pacientes de 5 hospitales de la Comunidad de Madrid entre enero de 2012 y junio de 2015, aleatorizados de forma ciega a una diferente prueba de imagen inicial y final, 36 a 18FDG PET/TC y 36 a TCMD64. Un médico nuclear y un radiólogo interpretaron la 18FDG PET/TC de manera independiente, llegando a un consenso post hoc. Por otro lado, un radiólogo ajeno interpretó la TCMD64 por separado. El patrón de referencia incluyó datos clínicos, pruebas complementarias y seguimiento. El Comité Ético de cada hospital aprobó el estudio y los sujetos firmaron su consentimiento por escrito.
ResultadosSe observó buena concordancia de ambas pruebas diagnósticas con el patrón de referencia en la estadificación inicial (18FDG PET/CT [k=0,5] y TCMD64 [k=0,6]), existiendo solo buena concordancia en la evaluación de la respuesta al final del tratamiento con la 18FDG PET/TC (k=0,7).
ConclusiónEn la estadificación inicial de pacientes con LDCGB existe un grado de acuerdo satisfactorio de la 18FDG PET/TC y la TCMD64 con el patrón de referencia, mientras que en la evaluación de la respuesta al final del tratamiento la 18FDG PET/TC es superior a la TCMD64.
Artículo
Comprando el artículo el PDF del mismo podrá ser descargado
Precio 19,34 €
Comprar ahora