The main causes of failure of allogeneic hematopoietic stem cell transplantation (allo-transplant) in patients with acute myeloid leukemia (AML) and myelodysplastic syndromes (MDS) are relapse and transplant-related mortality. Different scores have been designed to predict the prognosis of these patients. The objective of this study was to assess which score or combination has better outcome predictive capacity.
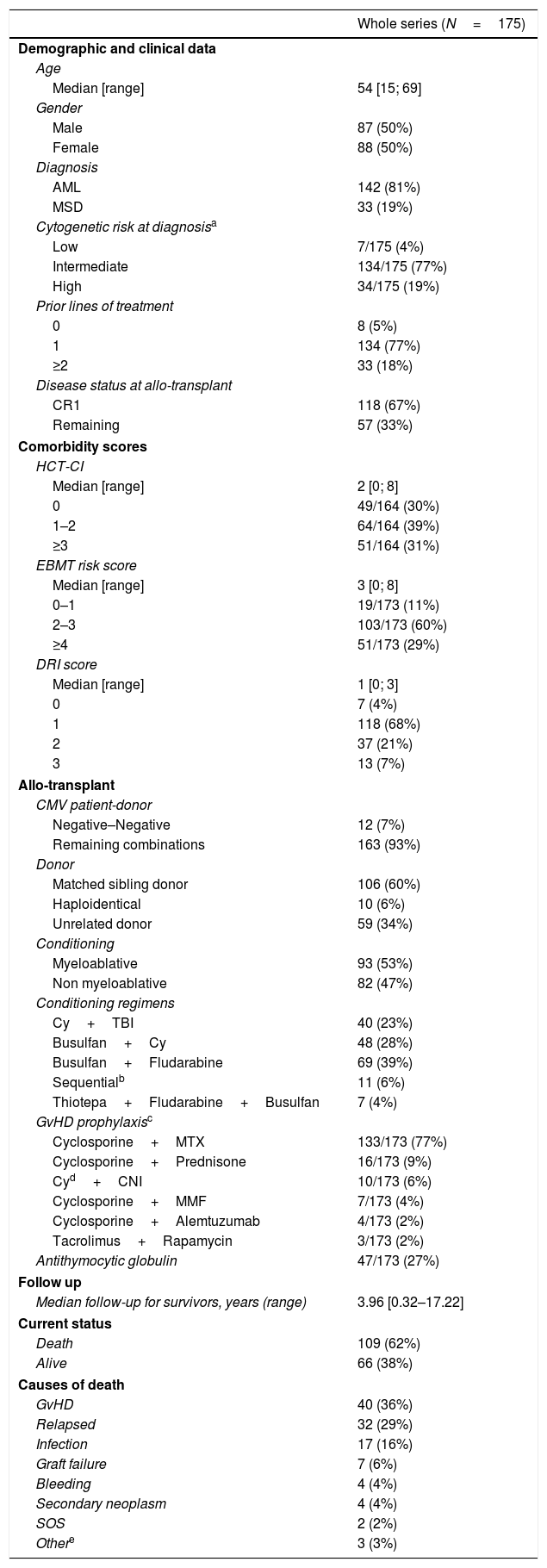
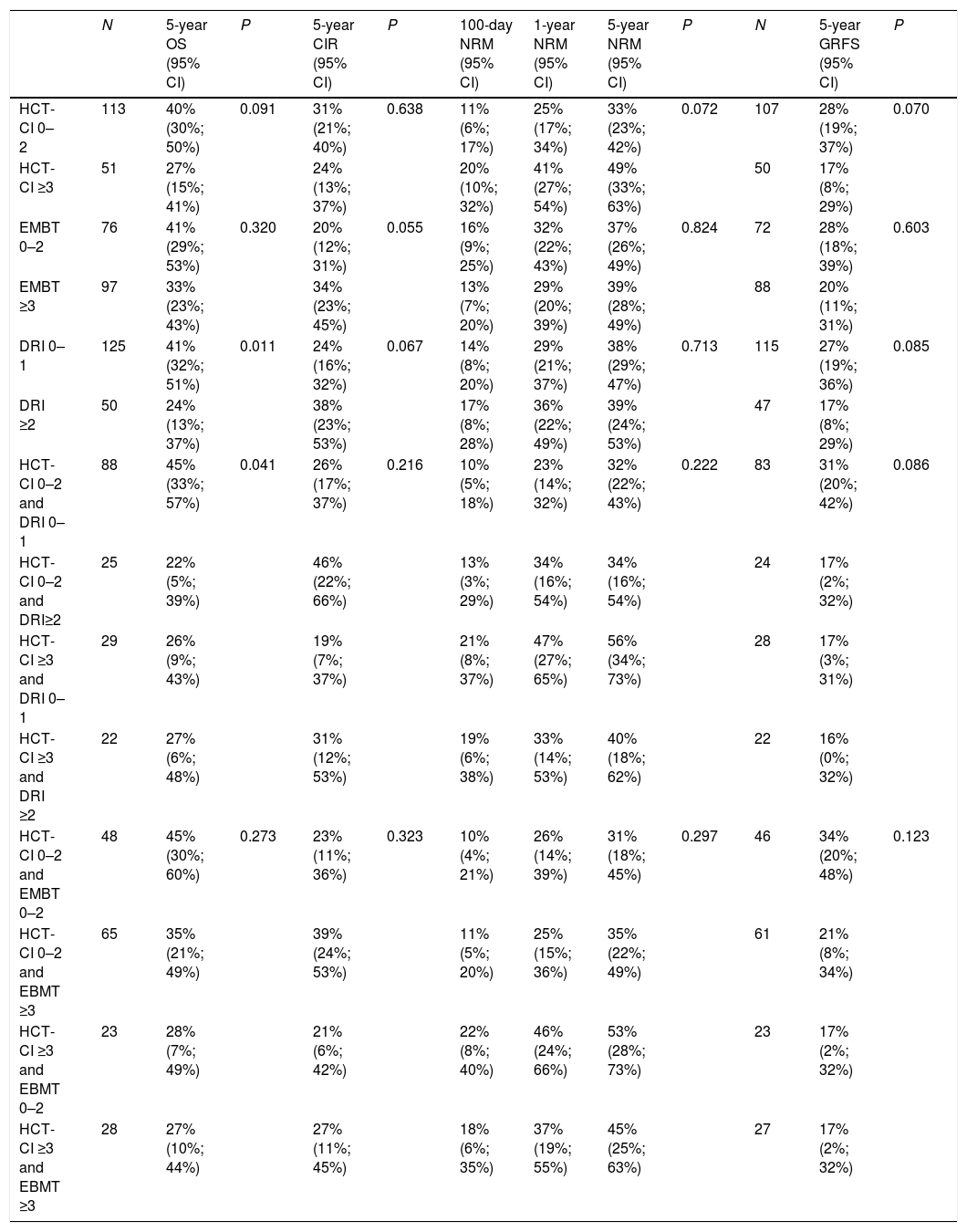
MethodsRetrospective analysis of patients with AML and MDS who received a first peripheral blood allo-transplant in a single center, between December 2001 and October 2019. Hematopoietic Cell Transplantation Comorbidity Index (HCT-CI), European Group for Blood and Marrow Transplantation (EBMT) and Disease Risk Index (DRI) scores were calculated. For each score and for the HCT-CI/DRI and HCT-CI/EBMT combinations, overall survival (OS), cumulative incidence of relapse (CIR), non-relapse-related mortality (NRM), and graft versus host disease-free relapse-free survival (GRFS) were analyzed.
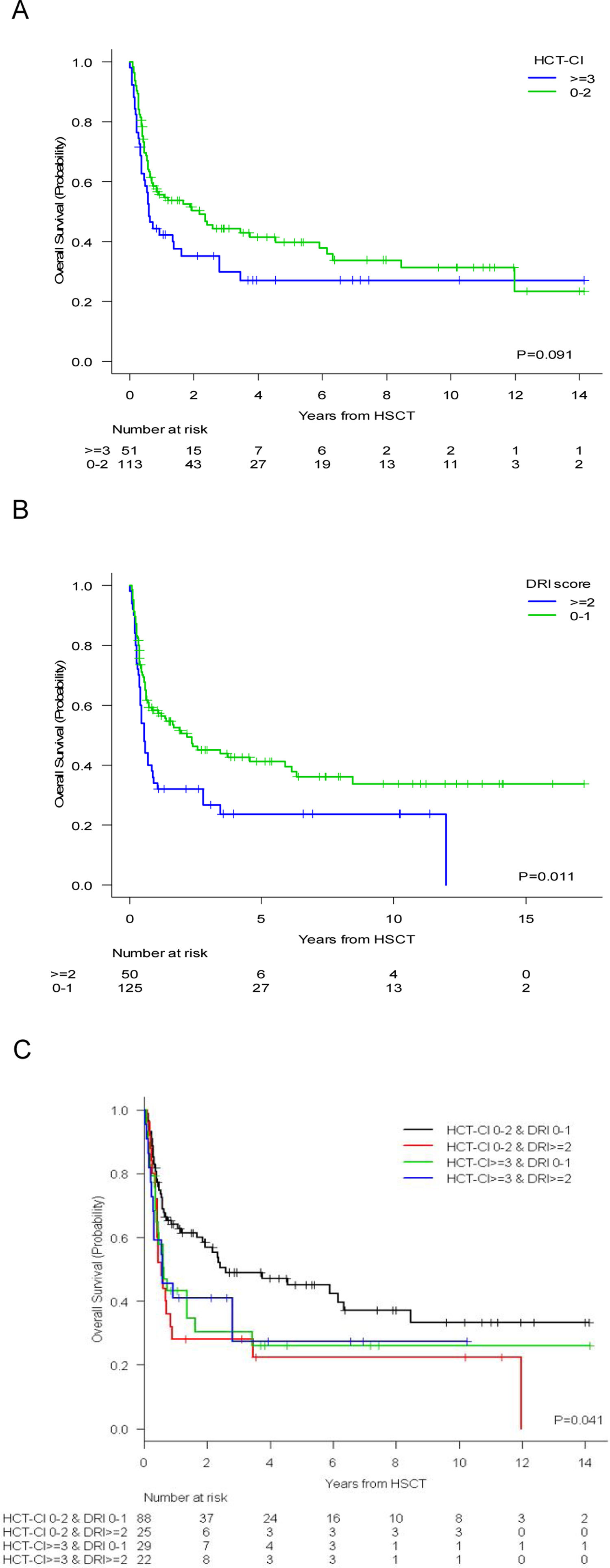
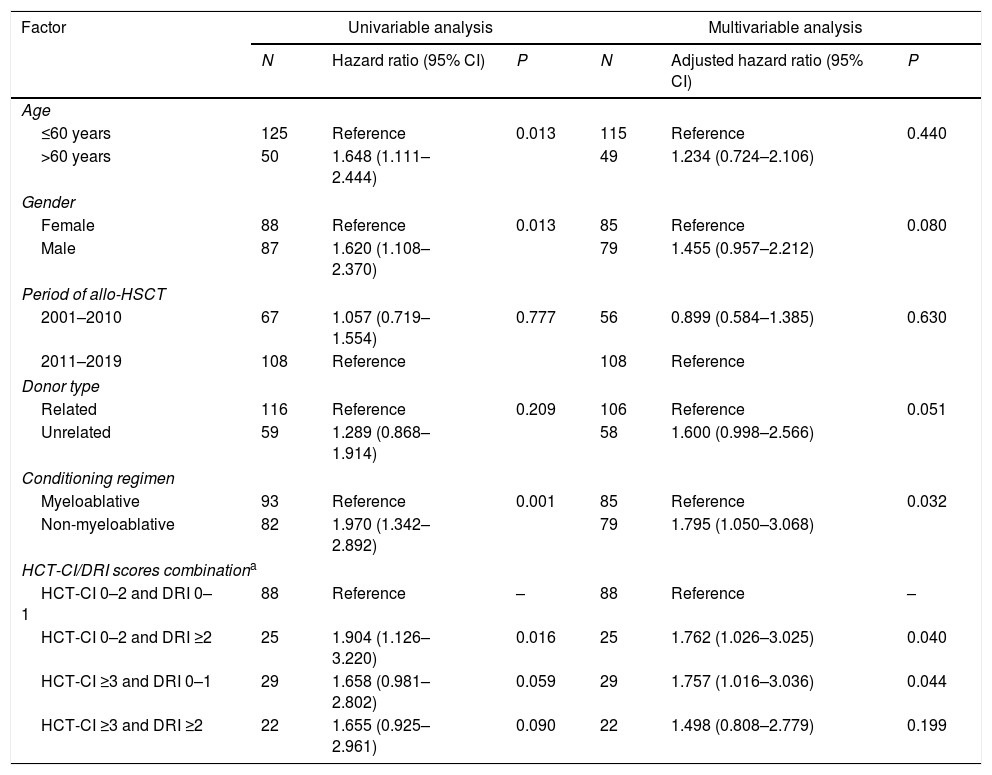
Results175 patients were evaluated. With a median (range) follow-up of 3.96 (0.32–17.22) years, the 5-year probabilities (95% CI) of OS, CIR, NRM, and GRFS were 36% (28%–44%), 28% (21%–35%), 38% (30%–46%) and 24% (17%–31%), respectively. For OS, only the DRI score selected two groups with statistically significant differences (DRI 0–1: 41% vs. DRI ≥2: 24%; p=0.011). The combination of DRI 0–1 and HCT-CI 0–2 showed OS probabilities of 45% vs. 26% for those with DRI 0–1 and HCT-CI ≥3; p=0.041.
ConclusionsIn patients with AML and MDS submitted to allo-transplant, the combination of HCT-CI and DRI scores provided the best stratification for OS.
Las principales causas de fallo del trasplante alogénico de células madre hematopoyéticas (alotrasplante) en pacientes con leucemia mieloide aguda (LMA) y síndromes mielodisplásicos (SMD) son las recaídas y la mortalidad debida al trasplante. Se han diseñado diferentes puntuaciones para predecir el pronóstico de dichos pacientes. El objetivo de este estudio fue evaluar qué puntuación o combinación tiene la mejor capacidad predictiva del resultado.
MétodosAnálisis retrospectivo de pacientes con LMA y SMD que recibieron un primer alotrasplante de sangre periférica en un único centro, entre diciembre de 2001 y octubre de 2019. Se calcularon las puntuaciones del Hematopoietic Cell Transplantation Comorbidity Index (HCT-CI), del European Group for Blood and Marrow Transplantation (EBMT) y del Disease Risk Index (DRI). Para cada puntuación y para las combinaciones HCT-CI/DRI y HCT-CI/EBMT se analizaron la supervivencia global (SG), la incidencia acumulada de recaídas (CIR), la mortalidad no relativa a las recaídas (NRM) y la supervivencia libre de recaídas y libre de enfermedad de injerto versus huésped (GRFS).
ResultadosSe evaluaron 175 pacientes. Con un seguimiento medio (rango) de 3,96 (0,32-17,22) años, las probabilidades a 5años (IC95%) de SG, CIR, NRM y GRFS fueron del 36% (28-44), del 28% (21-35), del 38% (30-46) y del 24% (17-31), respectivamente. Para la SG, solo la puntuación DRI seleccionó dos grupos con diferencias estadísticamente significativas (DRI 0-1: 41% vs. DRI≥2: 24%; p=0,011). La combinación de DRI 0-1 y HCT-CI 0-2 reflejó probabilidades de SG del 45% vs. 26% para los pacientes con DRI 0-1 y HCT-CI≥3 (p=0,041).
ConclusionesEn los pacientes con LMA y SMD sometidos a alotrasplante la combinación de las puntuaciones HCT-CI y DRI proporcionó la mejor estratificación para la SG.