IgG replacement therapy (IgG-RT) has radically changed the clinical evolution of primary immunodeficiencies, yet the information regarding secondary hypogammaglobulinemia (SHG) is insufficient or conflicting. We aim to describe clinical features, evolution and treatment of SHG patients in our center.
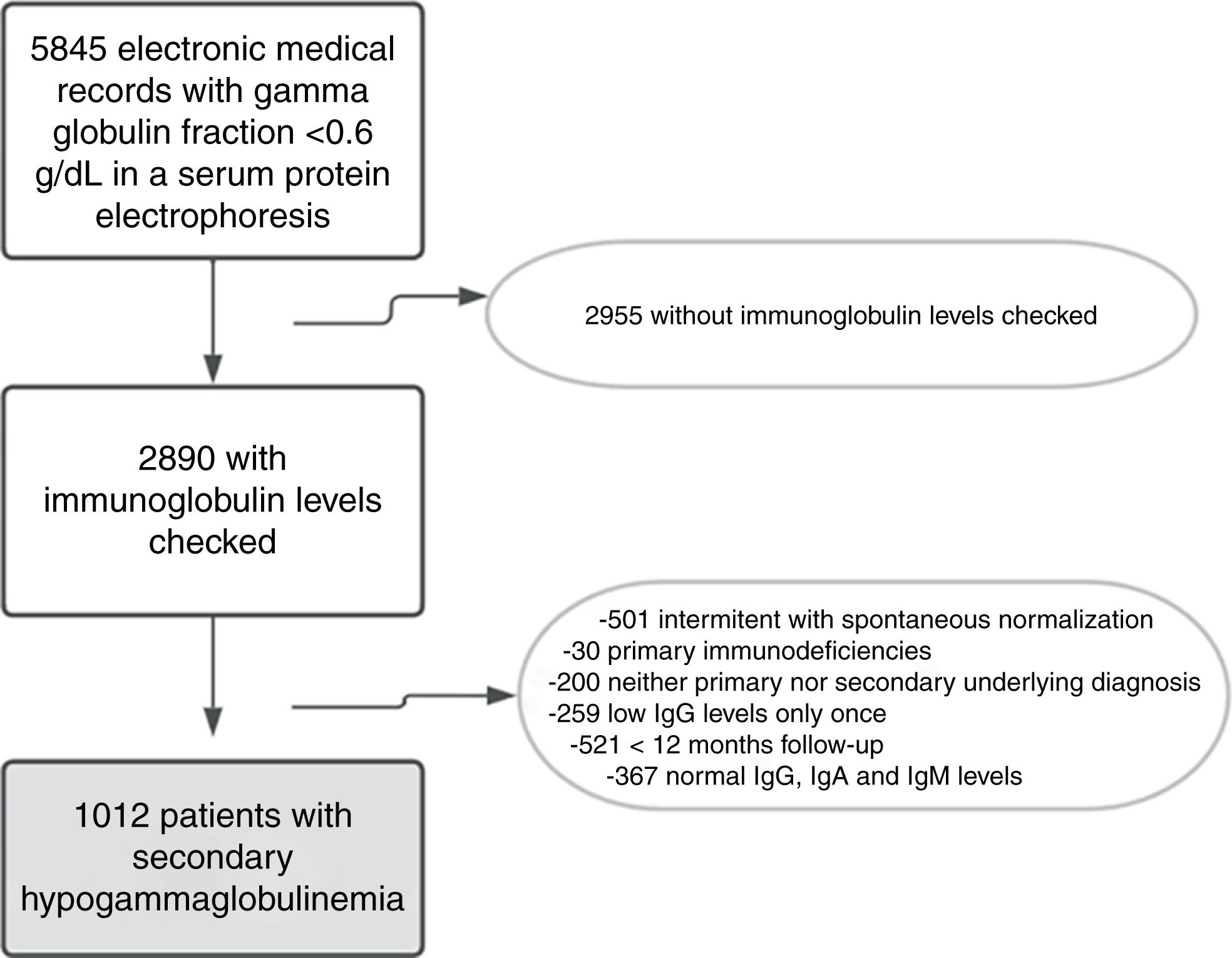
MethodsDynamic retrospective cohort between January 2001 and July 2021 of adults with gamma globulin fraction <0.6g/dL in a serum protein electrophoresis and a coincident decrease of IgG levels – with a disease-related SHG or treatment that reduces serum immunoglobulins.
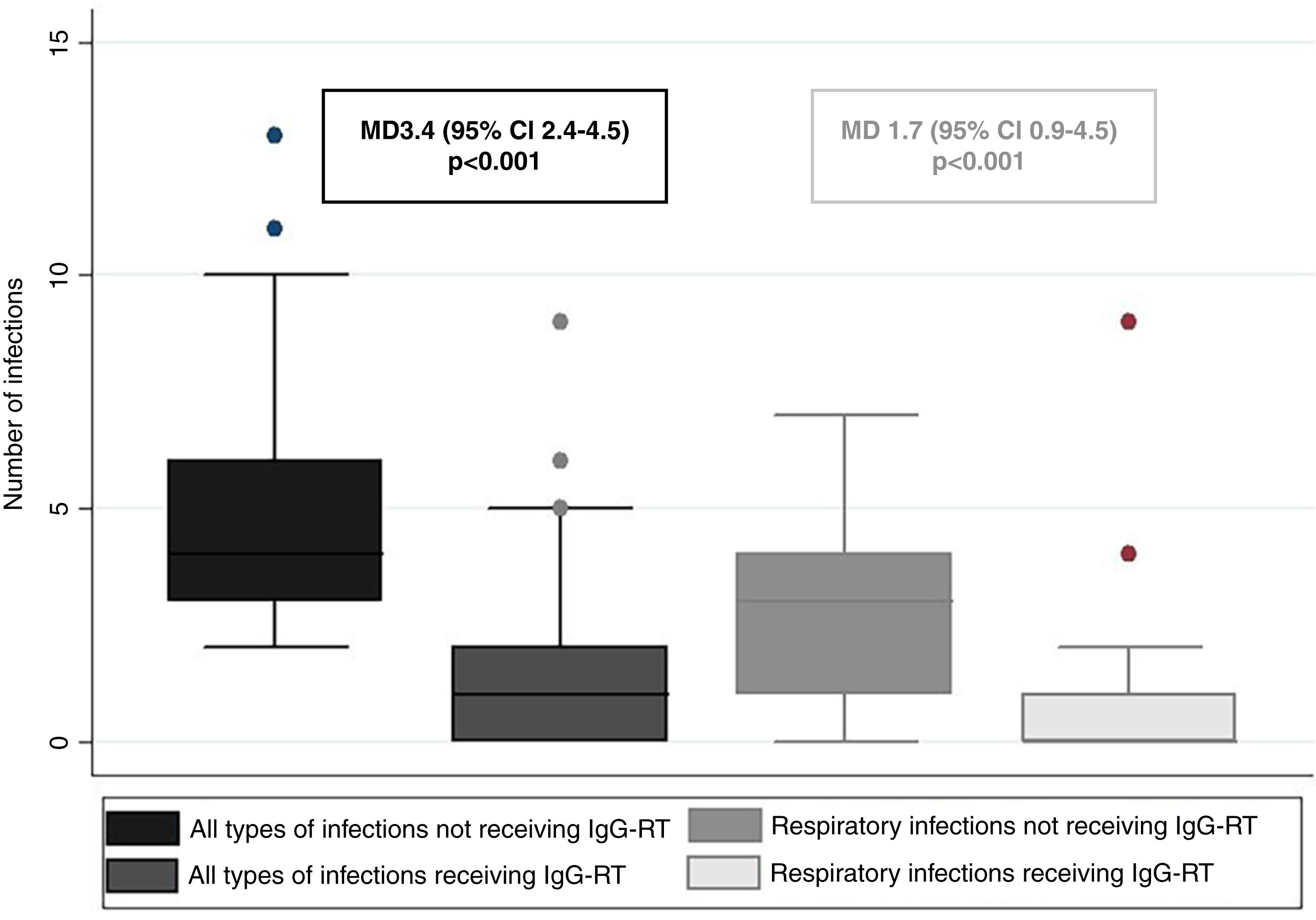
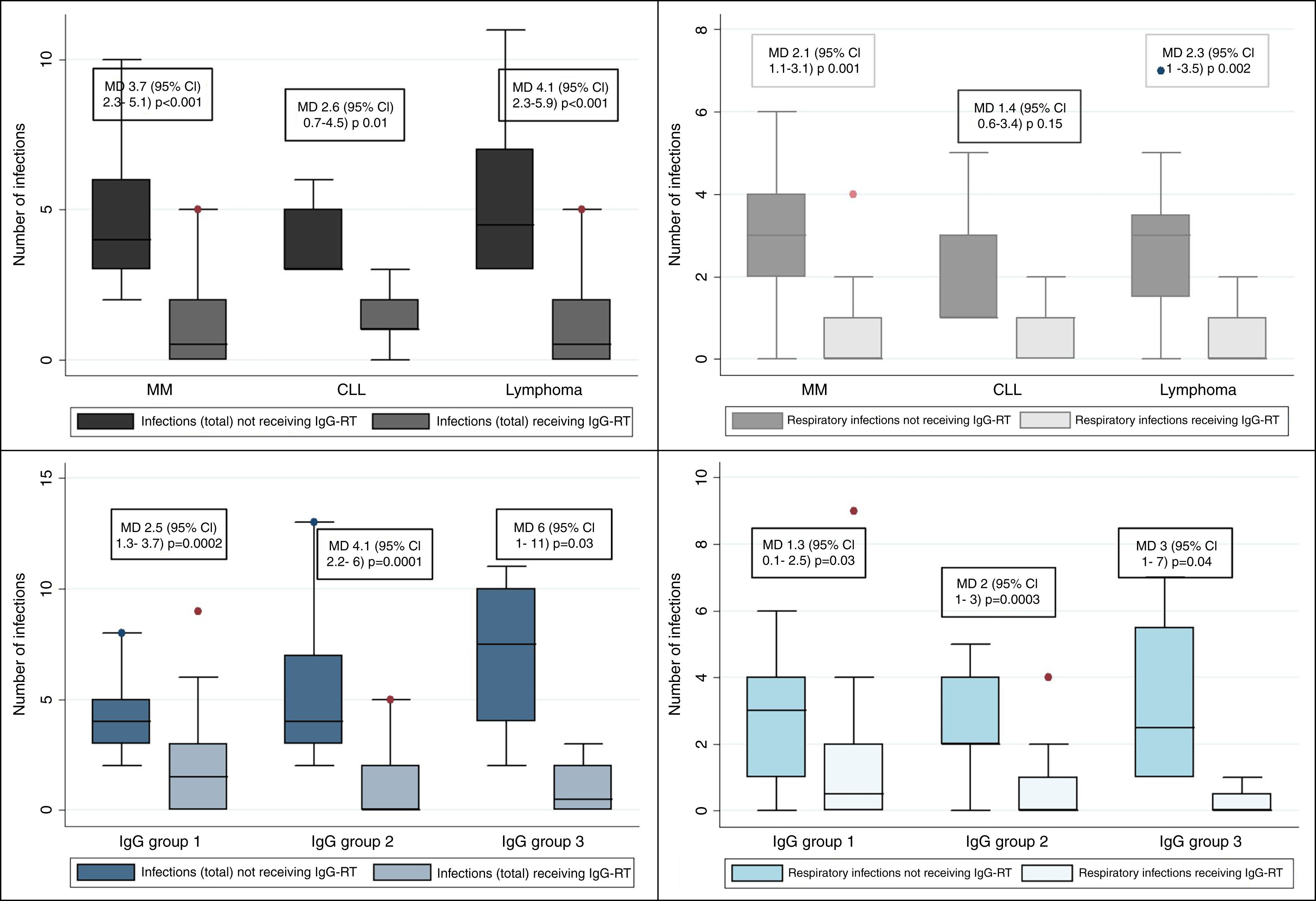
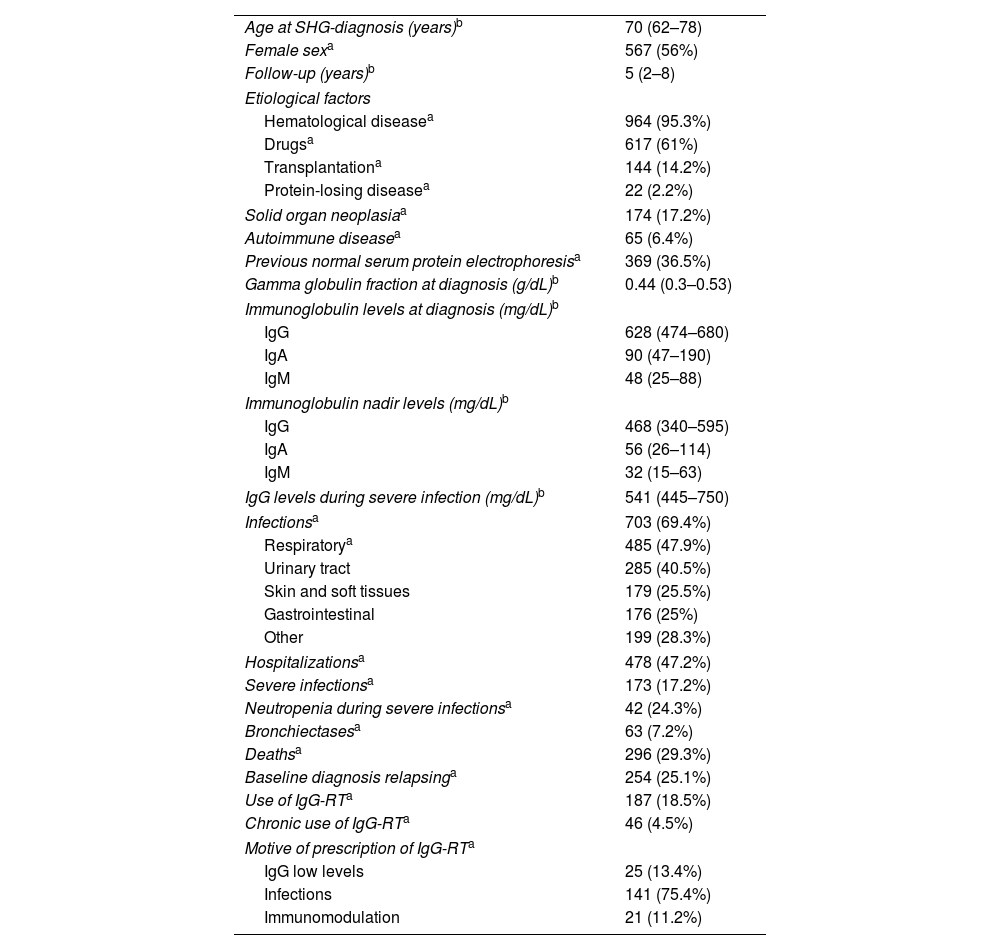
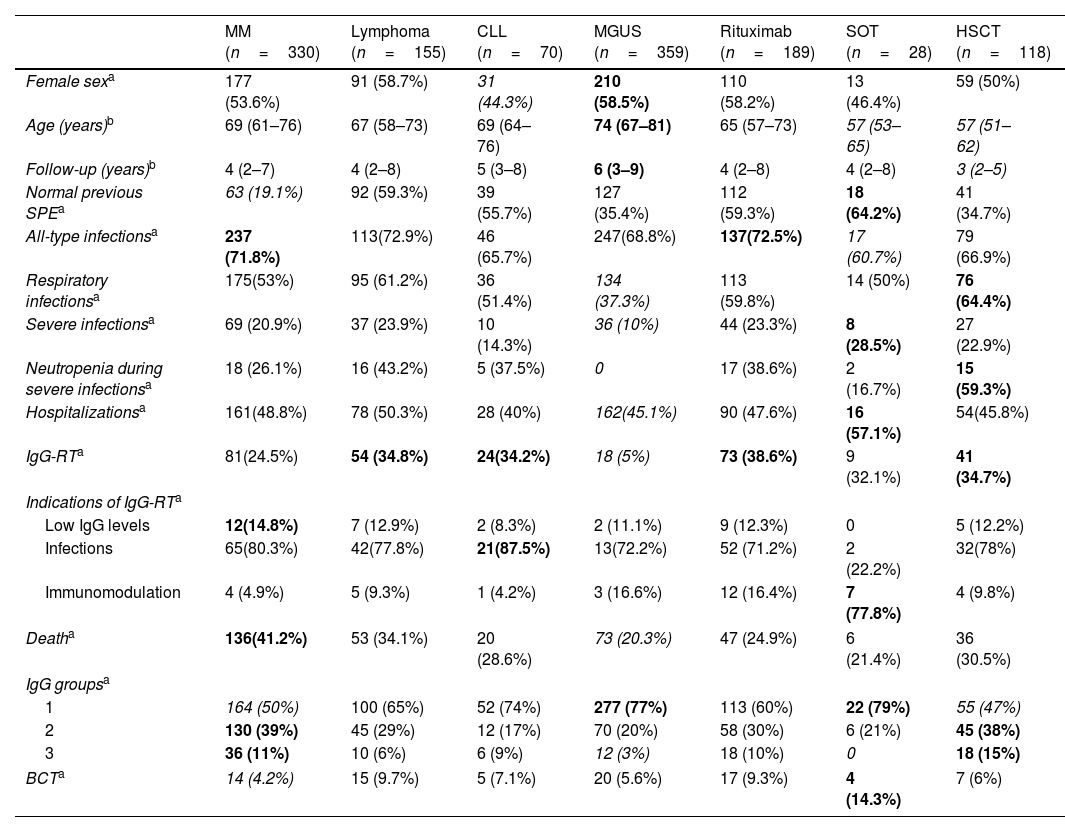
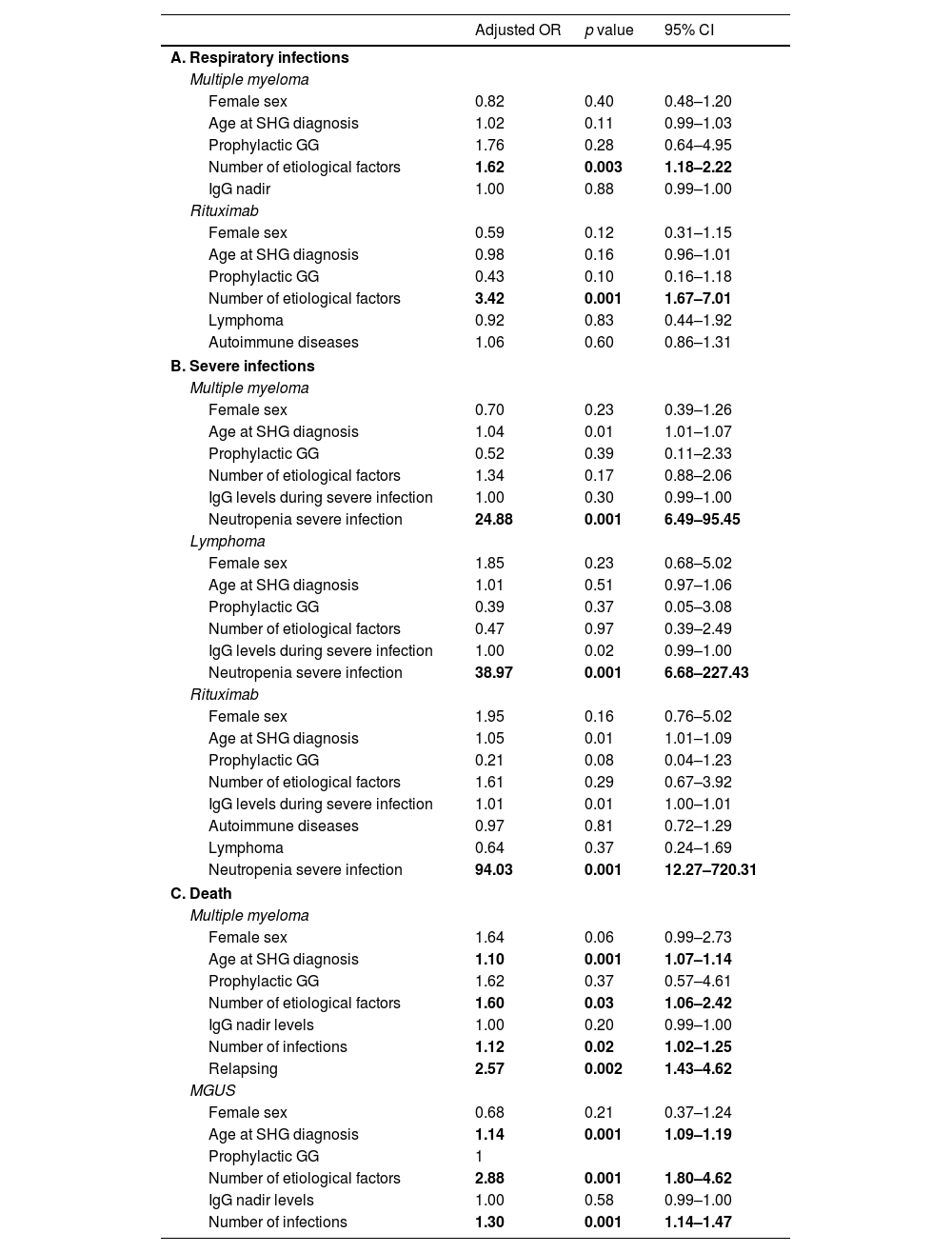
ResultsWe included 1012 patients with SHG with a median follow-up of 5 years (IQR 2–8). Hematological diseases were identified in 95% of the patients and 61% received drugs related to SHG. Sixty five percent had more than one etiological factor associated with SHG. Infectious diseases were present in 69% of the patients, 48% had respiratory infections and 17% had severe infections. There was statistical association between respiratory and severe infections with multiple myeloma (MM), lymphoma and rituximab. MGUS had less infections and death compared with other etiologies. IgG-RT was indicated in 18.7% of the patients and 4.6% received it for more than 6 months with variable intervals. Among the latter group, there was a significant reduction of all-type infections and respiratory infections with IgG-RT (p<0.001), and it was consistent with similar findings in lymphoma, MM and all IgG levels subgroups.
ConclusionSHG was associated with more than one etiological factor and a high frequency of infections. IgG-RT indication was irregular yet still effective. It is relevant to consider IgG levels screening, monitoring and accurate indication of IgG-RT.
La IgG sustitutiva ha cambiado radicalmente la evolución de las inmunodeficiencias primarias, mientras que la información sobre hipogammaglobulinemia secundaria (HGS) es insuficiente y discordante. El objetivo del estudio es describir las características clínicas, evolución y tratamiento de pacientes con HGS.
MétodosCohorte retrospectiva dinámica entre enero de 2001 y julio de 2021 de adultos con proteinograma y fracción de gammaglobulina <0,6g/dL y dosaje disminuido de IgG, con enfermedad o tratamiento que produzcan HGS.
ResultadosSe incluyó a 1.012 pacientes con HGS con una mediana de seguimiento de 5 años (IIC 2-8). El 95% tenía enfermedad hematológica y el 61% recibió fármacos asociados a HGS. El 65% tenía más de un factor etiológico asociado con HGS. El 69% presentó infecciones de cualquier tipo, el 48% infecciones respiratorias y el 17%, infecciones graves. Hubo asociación significativa entre infecciones respiratorias y graves entre los subgrupos de mieloma múltiple, linfoma y rituximab. Los pacientes con MGUS tuvieron menor frecuencia de infecciones y muerte comparados con otros factores etiológicos. El 18,7% de los pacientes recibió IgG sustitutiva y el 4,6% de forma crónica, con intervalos variables. Los últimos tuvieron disminución significativa de infecciones de cualquier tipo e infecciones respiratorias con IgG sustitutiva (p<0,001), que se mantuvo en los subgrupos con mieloma múltiple, linfoma y todos los niveles de IgG.
ConclusiónLa HGS asoció más de un factor etiológico y alta frecuencia de infecciones. La indicación de IgG sustitutiva fue irregular, pero, aún así, efectiva. Se plantea considerar el dosaje de inmunoglobulinas, monitoreo y la adecuada indicación de IgG sustitutiva.