An 80-year-old male, hospitalised due to coronavirus-associated pneumonitis with extensive bilateral affectation, observed in the admission scan. He stated he had dyspnoea at rest, cough and fever after 48 hours taking paracetamol and oral cefuroxime due to suspicion of bacterial pneumonia.
Previously independent, afflicted by prostatism, diabetes, dyslipidaemia and normal pressure hydrocephalus which limited the ability to walk. He received statins, anticholinergic drugs, clopidogrel and alpha-blockers.
He was indicated high flow oxygen therapy (transitory auto-PEEP valve without ventilation), lopinavir/ritonavir and hydroxychloroquine, methylprednisolone every eight hours and antibiotherapy. As a poor candidate for invasive measures, his worsening condition required a bolus dose of methylprednisolone (250 mg × 5) on day 5, immunoglobulin therapy on day 9 (×3) and anakinra from day 13 onwards, with marked improvement.
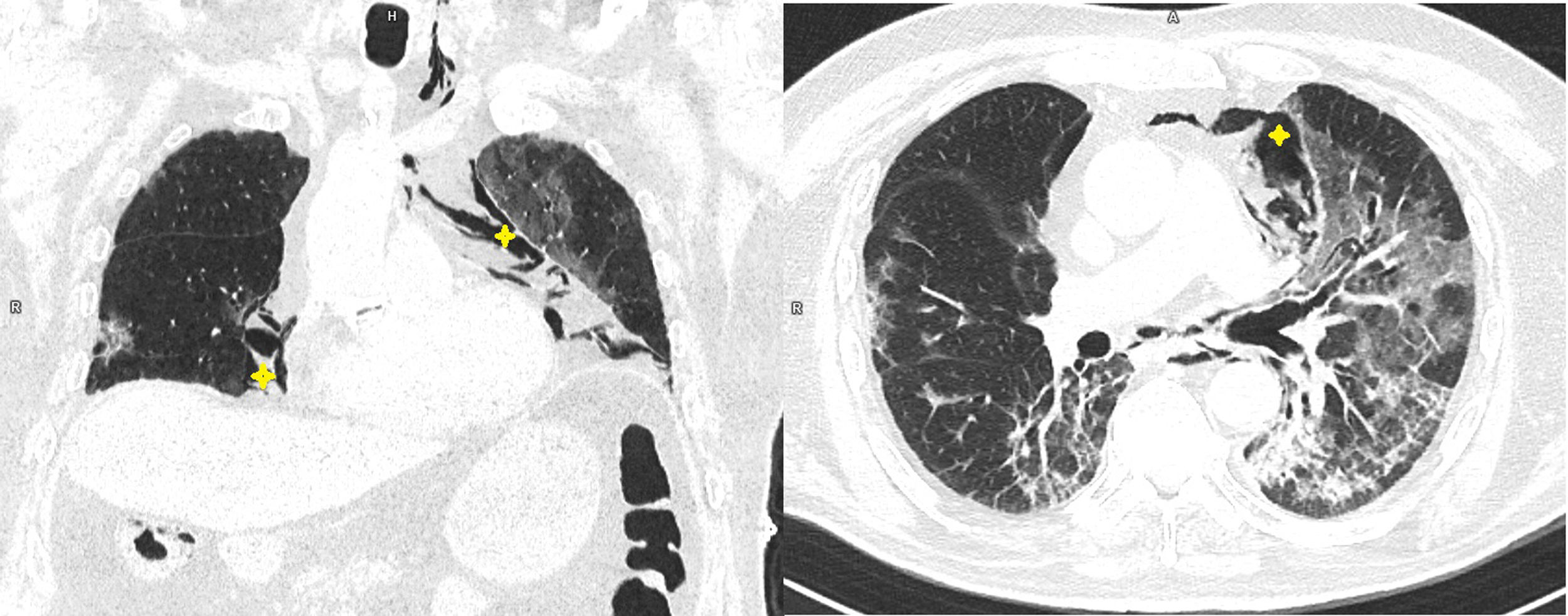
A control computerised tomography scan (CT) performed on day 19 (Fig. 1) showed a tendency towards fibrosis and pneumomediastinum dissecting to the cervical region. The fraction of inspired oxygen was increased with almost complete improvement shown by imaging six days later, and he was discharged after 27 days.
Pneumomediastinum is a rare clinical finding that seems to be occurring or reported more often in both early- and late-stage coronavirus-associated pneumonitis, usually with low flow/high inspired oxygen fractions, related or unrelated to the use of mechanical ventilation. Presumably, it indicates both lung fragility as well as the need to select appropriate imaging techniques for diagnosis and follow-up, to determine progress and inadvertent complications.
FundingThe authors have not received funding for the preparation of this paper.
Please cite this article as: Fernández-Raga S, Fidalgo-Navarro A, Bernardo-Cofiño J. Neumomediastino espontáneo en neumonitis por coronavirus evolucionada. Med Clin (Barc). 2020;155:421.