Artículo
Comprando el artículo el PDF del mismo podrá ser descargado
Precio 19,34 €
Comprar ahora
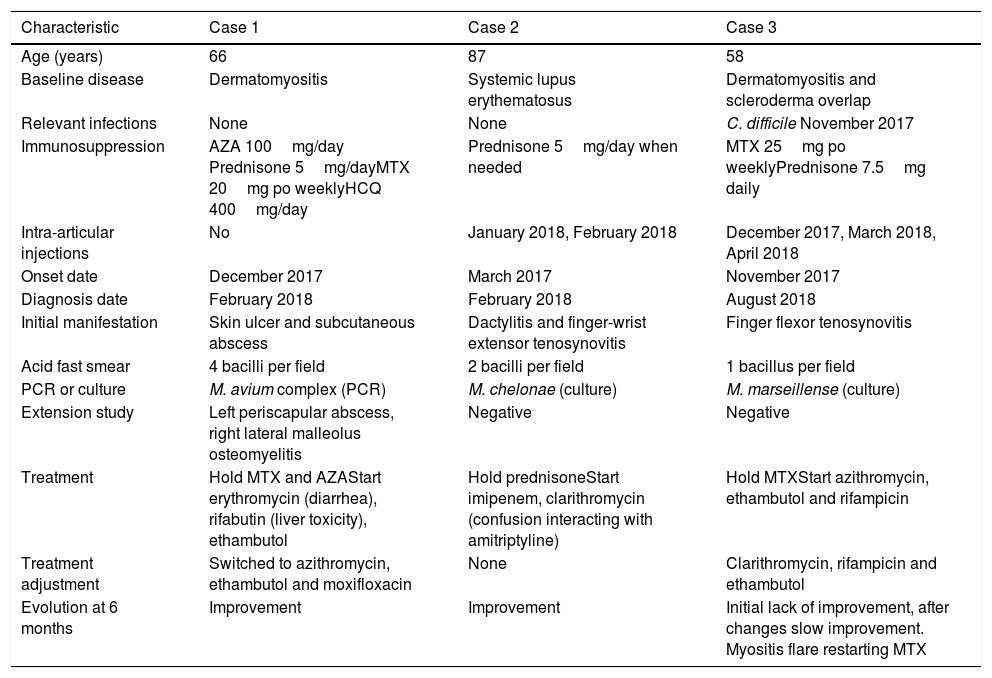
array:24 [ "pii" => "S0025775319303057" "issn" => "00257753" "doi" => "10.1016/j.medcli.2019.04.011" "estado" => "S300" "fechaPublicacion" => "2020-06-12" "aid" => "4862" "copyright" => "Elsevier España, S.L.U.. All rights reserved" "copyrightAnyo" => "2019" "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2020;154:468-9" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "Traduccion" => array:1 [ "en" => array:19 [ "pii" => "S2387020620301789" "issn" => "23870206" "doi" => "10.1016/j.medcle.2019.04.046" "estado" => "S300" "fechaPublicacion" => "2020-06-12" "aid" => "4862" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2020;154:468-9" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:10 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "A cluster of non-tuberculosis mycobacterial infections in patients with connective tissue diseases" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "468" "paginaFinal" => "469" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Clúster de infecciones por micobacterias no tuberculosas en pacientes con enfermedad del tejido conectivo" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Andreu Fernández-Codina, Michael Silverman, Janet E. Pope" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Andreu" "apellidos" => "Fernández-Codina" ] 1 => array:2 [ "nombre" => "Michael" "apellidos" => "Silverman" ] 2 => array:2 [ "nombre" => "Janet E." "apellidos" => "Pope" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "en" => array:9 [ "pii" => "S0025775319303057" "doi" => "10.1016/j.medcli.2019.04.011" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775319303057?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020620301789?idApp=UINPBA00004N" "url" => "/23870206/0000015400000011/v1_202006060744/S2387020620301789/v1_202006060744/en/main.assets" ] ] "itemSiguiente" => array:19 [ "pii" => "S0025775319303045" "issn" => "00257753" "doi" => "10.1016/j.medcli.2019.04.010" "estado" => "S300" "fechaPublicacion" => "2020-06-12" "aid" => "4861" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2020;154:469-70" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "es" => array:10 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Carta al Editor</span>" "titulo" => "Síndrome de dolor regional complejo tras cirugía ginecológica por laparoscopia" "tienePdf" => "es" "tieneTextoCompleto" => "es" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "469" "paginaFinal" => "470" ] ] "titulosAlternativos" => array:1 [ "en" => array:1 [ "titulo" => "Complex regional pain syndrome following laparoscopic gynecological surgery" ] ] "contieneTextoCompleto" => array:1 [ "es" => true ] "contienePdf" => array:1 [ "es" => true ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "Javier Molina-Gil, Ángel Fernández-Díaz, Luis Caminal-Montero" "autores" => array:3 [ 0 => array:2 [ "nombre" => "Javier" "apellidos" => "Molina-Gil" ] 1 => array:2 [ "nombre" => "Ángel" "apellidos" => "Fernández-Díaz" ] 2 => array:2 [ "nombre" => "Luis" "apellidos" => "Caminal-Montero" ] ] ] ] ] "idiomaDefecto" => "es" "Traduccion" => array:1 [ "en" => array:9 [ "pii" => "S2387020620301790" "doi" => "10.1016/j.medcle.2019.04.047" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020620301790?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775319303045?idApp=UINPBA00004N" "url" => "/00257753/0000015400000011/v1_202005280632/S0025775319303045/v1_202005280632/es/main.assets" ] "itemAnterior" => array:19 [ "pii" => "S0025775319303082" "issn" => "00257753" "doi" => "10.1016/j.medcli.2019.04.014" "estado" => "S300" "fechaPublicacion" => "2020-06-12" "aid" => "4865" "copyright" => "Elsevier España, S.L.U." "documento" => "simple-article" "crossmark" => 1 "subdocumento" => "cor" "cita" => "Med Clin. 2020;154:467" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "en" => array:10 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "Melena after endoscopic retrograde cholangiopancreatography: A warning sign of an impending subcapsular hepatic hematoma" "tienePdf" => "en" "tieneTextoCompleto" => "en" "paginas" => array:1 [ 0 => array:1 [ "paginaInicial" => "467" ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Melena posterior a colangiopancreatografía retrógrada endoscópica: un signo de alarma de inminente hematoma hepático subcapsular" ] ] "contieneTextoCompleto" => array:1 [ "en" => true ] "contienePdf" => array:1 [ "en" => true ] "autores" => array:1 [ 0 => array:2 [ "autoresLista" => "José Obeth Montoya Rojo, Marcos Antonio Amezcua Gutiérrez, Jorge Alberto Castañón-González" "autores" => array:3 [ 0 => array:2 [ "nombre" => "José Obeth" "apellidos" => "Montoya Rojo" ] 1 => array:2 [ "nombre" => "Marcos Antonio" "apellidos" => "Amezcua Gutiérrez" ] 2 => array:2 [ "nombre" => "Jorge Alberto" "apellidos" => "Castañón-González" ] ] ] ] ] "idiomaDefecto" => "en" "Traduccion" => array:1 [ "en" => array:9 [ "pii" => "S2387020620301777" "doi" => "10.1016/j.medcle.2019.04.045" "estado" => "S300" "subdocumento" => "" "abierto" => array:3 [ "ES" => false "ES2" => false "LATM" => false ] "gratuito" => false "lecturas" => array:1 [ "total" => 0 ] "idiomaDefecto" => "en" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S2387020620301777?idApp=UINPBA00004N" ] ] "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775319303082?idApp=UINPBA00004N" "url" => "/00257753/0000015400000011/v1_202005280632/S0025775319303082/v1_202005280632/en/main.assets" ] "en" => array:14 [ "idiomaDefecto" => true "cabecera" => "<span class="elsevierStyleTextfn">Letter to the Editor</span>" "titulo" => "A cluster of non-tuberculosis mycobacterial infections in patients with connective tissue diseases" "tieneTextoCompleto" => true "saludo" => "Dear Editor:" "paginas" => array:1 [ 0 => array:2 [ "paginaInicial" => "468" "paginaFinal" => "469" ] ] "autores" => array:1 [ 0 => array:4 [ "autoresLista" => "Andreu Fernández-Codina, Michael Silverman, Janet E. Pope" "autores" => array:3 [ 0 => array:4 [ "nombre" => "Andreu" "apellidos" => "Fernández-Codina" "email" => array:1 [ 0 => "andreu.fernandezcodina@lhsc.on.ca" ] "referencia" => array:3 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">a</span>" "identificador" => "aff0005" ] 1 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">c</span>" "identificador" => "aff0015" ] 2 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">*</span>" "identificador" => "cor0005" ] ] ] 1 => array:3 [ "nombre" => "Michael" "apellidos" => "Silverman" "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">b</span>" "identificador" => "aff0010" ] ] ] 2 => array:3 [ "nombre" => "Janet E." "apellidos" => "Pope" "referencia" => array:1 [ 0 => array:2 [ "etiqueta" => "<span class="elsevierStyleSup">a</span>" "identificador" => "aff0005" ] ] ] ] "afiliaciones" => array:3 [ 0 => array:3 [ "entidad" => "Rheumatology Division, Department of Medicine, University of Western Ontario, London, ON, Canada" "etiqueta" => "a" "identificador" => "aff0005" ] 1 => array:3 [ "entidad" => "Infectious Diseases Division, Department of Medicine, University of Western Ontario, London, ON, Canada" "etiqueta" => "b" "identificador" => "aff0010" ] 2 => array:3 [ "entidad" => "Systemic Autoimmune Diseases Unit, Internal Medicine Department, Hospital Universitari Vall d’Hebron, Universitat Autònoma de Barcelona, Barcelona, Spain" "etiqueta" => "c" "identificador" => "aff0015" ] ] "correspondencia" => array:1 [ 0 => array:3 [ "identificador" => "cor0005" "etiqueta" => "⁎" "correspondencia" => "Corresponding author." ] ] ] ] "titulosAlternativos" => array:1 [ "es" => array:1 [ "titulo" => "Clúster de infecciones por micobacterias no tuberculosas en pacientes con enfermedad del tejido conectivo" ] ] "textoCompleto" => "<span class="elsevierStyleSections"><p id="par0005" class="elsevierStylePara elsevierViewall">Non-tuberculous mycobacteria (NTM) can be found in multiple reservoirs and cause infections in immunocompetent and immunocompromised patients. The isolation of NTM in pulmonary samples increased in Ontario from 1998 to 2010, but the isolation in extrapulmonary samples was stable (4%).<a class="elsevierStyleCrossRef" href="#bib0030"><span class="elsevierStyleSup">1</span></a> Skin/soft tissue NTM infections (representing the second most common extra-pulmonary location) decreased. We report a cluster of NTM soft-tissue and bone infections in patients with connective tissue diseases (CTD) from a single Rheumatology practice in London, Ontario (<a class="elsevierStyleCrossRef" href="#tbl0005">Table 1</a>).</p><elsevierMultimedia ident="tbl0005"></elsevierMultimedia><p id="par0010" class="elsevierStylePara elsevierViewall">Case 1. A 66-year-old woman with longstanding dermatomyositis in remission in February 2018. She reported an ongoing left calf necrotic ulcer (diameter 4<span class="elsevierStyleHsp" style=""></span>cm) since December 2017, a small ulcerative plaque in the proximal third of her left arm and a lump in the proximal third of her left elbow. She also had some mechanical pain in her left scapula. The elbow lump resulted in an abscess, which was drained and sent for culture, resulting positive for <span class="elsevierStyleItalic">Mycobacterium avium complex</span> (MAC). A bone scan showed an abscess posterior to the left scapula and a focus of osteomyelitis in the right ankle.</p><p id="par0015" class="elsevierStylePara elsevierViewall">Case 2. An 87-year-old woman with longstanding systemic lupus erythematosus (SLE) in remission. Since March 2017, she had an ongoing dactylitis in the 2<span class="elsevierStyleSup">nd</span> finger left hand that progressed to a tenosynovitis of the left dorsal wrist in October 2017. Given the functional impairment of the hand, she had the tenosynovitis injected with 40<span class="elsevierStyleHsp" style=""></span>mg of triamcinolone and 0.5<span class="elsevierStyleHsp" style=""></span>mL of a 1% lidocaine solution with a clean technique in early January and February 2018. In the later date, a synovial fluid sample was sent for analysis and culture. Ten days after, the laboratory notified the growth of <span class="elsevierStyleItalic">Mycobacterium chelonae</span>.</p><p id="par0020" class="elsevierStylePara elsevierViewall">Case 3. A 58 year-old woman with a longstanding overlap of dermatomyositis and limited cutaneous systemic sclerosis, with interstitial lung disease, presented with a flexor tenosynovitis of the 3<span class="elsevierStyleSup">rd</span> finger of her left hand in December 2017. One month before she had been admitted due to a <span class="elsevierStyleItalic">Clostridium difficile</span> colitis, after receiving 2 courses of antibiotics for an episode of sinusitis. She had the finger injected with triamcinolone and lidocaine, and prednisone was increased to 10<span class="elsevierStyleHsp" style=""></span>mg/day. In the following months, the tenosynovitis had progressive worsening and she was injected on 2 more occasions. In August 2018, she had erythema, swelling and pain in between the 3<span class="elsevierStyleSup">rd</span> metacarpophalangeal joint and the proximal interphalangeal joint. There was some fluid collection and a sample was obtained, resulting in a positive acid fast staining. The culture was positive for <span class="elsevierStyleItalic">Mycobacterium marseillense</span>.</p><p id="par0025" class="elsevierStylePara elsevierViewall">All patients were evaluated by an Infectious Diseases specialist. No patient had extra-risk factors (trauma, drug abuse, previous injections or surgeries, exposures), testing for human immunodeficiency virus was negative, none had symptoms of pulmonary involvement and all had normal chest X-rays. Lidocaine and triamcinolone vials from the Rheumatology clinic tested negative for any contamination. They all started specific anti-mycobacterial treatment (<a class="elsevierStyleCrossRef" href="#tbl0005">Table 1</a>), for 6 months in patient 2 (elder and localized disease) and 12 months in patients 1 (multiple abscesses) and 2 (slow improvement and resistance to moxifloxacin and linezolid). Corticoid sparing agents were held and glucocorticoids were reduced to the minimum effective dose.</p><p id="par0030" class="elsevierStylePara elsevierViewall">Recent American studies show an increase in the incidence of NTM cutaneous infections, from 0.7/100,000 person-years (period 1980–1999) to 2/100,000 person-years (2000–2009).<a class="elsevierStyleCrossRef" href="#bib0035"><span class="elsevierStyleSup">2</span></a> All series show a predominance of MAC among the overall isolates for NTM, and also for the skin/soft tissue infections.<a class="elsevierStyleCrossRefs" href="#bib0030"><span class="elsevierStyleSup">1,2</span></a> Skin infections caused by rapid growing mycobacteria like <span class="elsevierStyleItalic">M. marinum</span> or <span class="elsevierStyleItalic">M. chelonae</span> have become more frequent recently.<a class="elsevierStyleCrossRef" href="#bib0035"><span class="elsevierStyleSup">2</span></a> Opportunistic infections by tuberculous and NTM were commonly associated with immunosuppression in inflammatory myopathy.<a class="elsevierStyleCrossRef" href="#bib0040"><span class="elsevierStyleSup">3</span></a> A review of SLE patients with NTM skin infection reported cases of infections with or without ongoing immunosupressive treatment.<a class="elsevierStyleCrossRef" href="#bib0045"><span class="elsevierStyleSup">4</span></a> NTM infections are well known to be associated to the use of biologic therapies. No solid association between CTD and NTM infections has been reported.</p><p id="par0035" class="elsevierStylePara elsevierViewall">Diagnosis of NTM skin/soft tissue or bone infections can be challenging. A retrospective study regarding upper extremity NTM infections,<a class="elsevierStyleCrossRef" href="#bib0050"><span class="elsevierStyleSup">5</span></a> showed a median diagnostic delay of 4 months due to the paucity of the symptoms. Hands were the most commonly involved location. Half of the patients presented with erythema, joint pain and swelling. These clinical signs might be mimicked by CTD or inflammatory arthritis. Local steroid injections might contribute to worsen the infection and to mask it. Nevertheless, patients with autoimmune diseases, when treated, are immunosuppressed and injections might inoculate mycobacteria that could already be colonizing patients or the injectate. Reducing immunosupressants to the minimally effective doses seems reasonable at the beginning of the anti-tuberculous treatment, but disease flares may require dose increases.</p><p id="par0040" class="elsevierStylePara elsevierViewall">Physicians should be aware of NTM infections in patients with CTD. Clinical suspicion and sending samples for specific mycobacteria smears and cultures are vital.</p></span>" "pdfFichero" => "main.pdf" "tienePdf" => true "NotaPie" => array:1 [ 0 => array:2 [ "etiqueta" => "☆" "nota" => "<p class="elsevierStyleNotepara" id="npar0005">In accordance with the Western Ethics Review Boards’ procedures, this case report was waived from an assessment.</p>" ] ] "multimedia" => array:1 [ 0 => array:8 [ "identificador" => "tbl0005" "etiqueta" => "Table 1" "tipo" => "MULTIMEDIATABLA" "mostrarFloat" => true "mostrarDisplay" => false "detalles" => array:1 [ 0 => array:3 [ "identificador" => "at1" "detalle" => "Table " "rol" => "short" ] ] "tabla" => array:2 [ "leyenda" => "<p id="spar0010" class="elsevierStyleSimplePara elsevierViewall">PCR: polymerase chain reaction; AZA: azathioprine; HCQ: hydroxychloroquine; MTX: methotrexate; po: per os.</p>" "tablatextoimagen" => array:1 [ 0 => array:2 [ "tabla" => array:1 [ 0 => """ <table border="0" frame="\n \t\t\t\t\tvoid\n \t\t\t\t" class=""><thead title="thead"><tr title="table-row"><th class="td" title="\n \t\t\t\t\ttable-head\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t" scope="col" style="border-bottom: 2px solid black">Characteristic \t\t\t\t\t\t\n \t\t\t\t\t\t</th><th class="td" title="\n \t\t\t\t\ttable-head\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t" scope="col" style="border-bottom: 2px solid black">Case 1 \t\t\t\t\t\t\n \t\t\t\t\t\t</th><th class="td" title="\n \t\t\t\t\ttable-head\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t" scope="col" style="border-bottom: 2px solid black">Case 2 \t\t\t\t\t\t\n \t\t\t\t\t\t</th><th class="td" title="\n \t\t\t\t\ttable-head\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t" scope="col" style="border-bottom: 2px solid black">Case 3 \t\t\t\t\t\t\n \t\t\t\t\t\t</th></tr></thead><tbody title="tbody"><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Age (years) \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">66 \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">87 \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">58 \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Baseline disease \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Dermatomyositis \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Systemic lupus erythematosus \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Dermatomyositis and scleroderma overlap \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Relevant infections \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">None \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">None \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t"><span class="elsevierStyleItalic">C. difficile</span> November 2017 \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Immunosuppression \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">AZA 100<span class="elsevierStyleHsp" style=""></span>mg/day Prednisone 5<span class="elsevierStyleHsp" style=""></span>mg/dayMTX 20<span class="elsevierStyleHsp" style=""></span>mg po weeklyHCQ 400<span class="elsevierStyleHsp" style=""></span>mg/day \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Prednisone 5<span class="elsevierStyleHsp" style=""></span>mg/day when needed \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">MTX 25<span class="elsevierStyleHsp" style=""></span>mg po weeklyPrednisone 7.5<span class="elsevierStyleHsp" style=""></span>mg daily \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Intra-articular injections \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">No \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">January 2018, February 2018 \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">December 2017, March 2018, April 2018 \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Onset date \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">December 2017 \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">March 2017 \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">November 2017 \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Diagnosis date \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">February 2018 \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">February 2018 \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">August 2018 \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Initial manifestation \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Skin ulcer and subcutaneous abscess \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Dactylitis and finger-wrist extensor tenosynovitis \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Finger flexor tenosynovitis \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Acid fast smear \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">4 bacilli per field \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">2 bacilli per field \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">1 bacillus per field \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">PCR or culture \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t"><span class="elsevierStyleItalic">M. avium</span> complex (PCR) \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t"><span class="elsevierStyleItalic">M. chelonae</span> (culture) \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t"><span class="elsevierStyleItalic">M. marseillense</span> (culture) \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Extension study \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Left periscapular abscess, right lateral malleolus osteomyelitis \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Negative \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Negative \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Treatment \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Hold MTX and AZAStart erythromycin (diarrhea), rifabutin (liver toxicity), ethambutol \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Hold prednisoneStart imipenem, clarithromycin (confusion interacting with amitriptyline) \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Hold MTXStart azithromycin, ethambutol and rifampicin \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Treatment adjustment \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Switched to azithromycin, ethambutol and moxifloxacin \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">None \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Clarithromycin, rifampicin and ethambutol \t\t\t\t\t\t\n \t\t\t\t</td></tr><tr title="table-row"><td class="td-with-role" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t ; entry_with_role_rowhead " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Evolution at 6 months \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Improvement \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Improvement \t\t\t\t\t\t\n \t\t\t\t</td><td class="td" title="\n \t\t\t\t\ttable-entry\n \t\t\t\t " align="left" valign="\n \t\t\t\t\ttop\n \t\t\t\t">Initial lack of improvement, after changes slow improvement. Myositis flare restarting MTX \t\t\t\t\t\t\n \t\t\t\t</td></tr></tbody></table> """ ] "imagenFichero" => array:1 [ 0 => "xTab2300052.png" ] ] ] ] "descripcion" => array:1 [ "en" => "<p id="spar0005" class="elsevierStyleSimplePara elsevierViewall">Characteristics of the CTD patients with NTM infections.</p>" ] ] ] "bibliografia" => array:2 [ "titulo" => "References" "seccion" => array:1 [ 0 => array:2 [ "identificador" => "bibs0015" "bibliografiaReferencia" => array:5 [ 0 => array:3 [ "identificador" => "bib0030" "etiqueta" => "1" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Pulmonary versus nonpulmonary nontuberculous mycobacteria, Ontario, Canada" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:4 [ 0 => "S.K. Brode" 1 => "A. Marchand-Austin" 2 => "F.B. Jamieson" 3 => "T.K. Marras" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.3201/eid2311.170959" "Revista" => array:6 [ "tituloSerie" => "Emerg Infect Dis" "fecha" => "2017" "volumen" => "23" "paginaInicial" => "1898" "paginaFinal" => "1901" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/29048292" "web" => "Medline" ] ] ] ] ] ] ] ] 1 => array:3 [ "identificador" => "bib0035" "etiqueta" => "2" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Increased incidence of cutaneous nontuberculous mycobacterial infection, 1980 to 2009: a population-based study" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:5 [ 0 => "A.B. Wentworth" 1 => "L.A. Drage" 2 => "N.L. Wengenack" 3 => "J.W. Wilson" 4 => "C.M. Lohse" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:5 [ "tituloSerie" => "Mayo Clin Proc" "fecha" => "2013" "volumen" => "88" "paginaInicial" => "38" "paginaFinal" => "45" ] ] ] ] ] ] 2 => array:3 [ "identificador" => "bib0040" "etiqueta" => "3" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Opportunistic infections in patients with idiopathic inflammatory myopathies" "autores" => array:1 [ 0 => array:2 [ "etal" => true "autores" => array:6 [ 0 => "A. Redondo-Benito" 1 => "A. Curran" 2 => "A. Villar-Gomez" 3 => "E. Trallero-Araguas" 4 => "A. Fernández-Codina" 5 => "I. Pinal-Fernandez" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1111/1756-185X.13255" "Revista" => array:6 [ "tituloSerie" => "Int J Rheum Dis" "fecha" => "2018" "volumen" => "21" "paginaInicial" => "487" "paginaFinal" => "496" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/29314762" "web" => "Medline" ] ] ] ] ] ] ] ] 3 => array:3 [ "identificador" => "bib0045" "etiqueta" => "4" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Skin nontuberculous mycobacterial infection in systemic lupus erythematosus: an unusual skin infection mimicking lupus vasculitis" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:5 [ 0 => "Z. Touma" 1 => "A. Haddad" 2 => "D.D. Gladman" 3 => "E.M. Uleryk" 4 => "M.B. Urowitz" ] ] ] ] ] "host" => array:1 [ 0 => array:2 [ "doi" => "10.1016/j.semarthrit.2012.08.002" "Revista" => array:6 [ "tituloSerie" => "Semin Arthritis Rheum" "fecha" => "2013" "volumen" => "42" "paginaInicial" => "498" "paginaFinal" => "506" "link" => array:1 [ 0 => array:2 [ "url" => "https://www.ncbi.nlm.nih.gov/pubmed/23332736" "web" => "Medline" ] ] ] ] ] ] ] ] 4 => array:3 [ "identificador" => "bib0050" "etiqueta" => "5" "referencia" => array:1 [ 0 => array:2 [ "contribucion" => array:1 [ 0 => array:2 [ "titulo" => "Nontuberculous mycobacterial infections of the upper extremity: 15-year experience at a tertiary care medical center" "autores" => array:1 [ 0 => array:2 [ "etal" => false "autores" => array:6 [ 0 => "D. Sotello" 1 => "H.W. Garner" 2 => "M.G. Heckman" 3 => "N.N. Diehl" 4 => "P.M. Murray" 5 => "S. Alvarez" ] ] ] ] ] "host" => array:1 [ 0 => array:1 [ "Revista" => array:3 [ "tituloSerie" => "J Hand Surg Am" "fecha" => "2018" "volumen" => "43" ] ] ] ] ] ] ] ] ] ] ] "idiomaDefecto" => "en" "url" => "/00257753/0000015400000011/v1_202005280632/S0025775319303057/v1_202005280632/en/main.assets" "Apartado" => array:4 [ "identificador" => "66430" "tipo" => "SECCION" "es" => array:2 [ "titulo" => "Cartas al Editor" "idiomaDefecto" => true ] "idiomaDefecto" => "es" ] "PDF" => "https://static.elsevier.es/multimedia/00257753/0000015400000011/v1_202005280632/S0025775319303057/v1_202005280632/en/main.pdf?idApp=UINPBA00004N&text.app=https://www.elsevier.es/" "EPUB" => "https://multimedia.elsevier.es/PublicationsMultimediaV1/item/epub/S0025775319303057?idApp=UINPBA00004N" ]
Consulte los artículos y contenidos publicados en este medio, además de los e-sumarios de las revistas científicas en el mismo momento de publicación
Esté informado en todo momento gracias a las alertas y novedades
Acceda a promociones exclusivas en suscripciones, lanzamientos y cursos acreditados
Medicina Clínica, fundada en 1943, es la única publicación semanal de contenido clínico que se edita en España y constituye el máximo exponente de la calidad y pujanza de la medicina española. Son características fundamentales de esta publicación el rigor científico y metodológico de sus artículos, la actualidad de los temas y, sobre todo, su sentido práctico, buscando siempre que la información sea de la mayor utilidad en la práctica clínica. Los contenidos de Medicina Clínica abarcan dos frentes: trabajos de investigación original rigurosamente seleccionados atendiendo a su calidad, originalidad e interés, y trabajos orientados a la formación continuada, encomendados por la revista a autores relevantes (Editoriales, Revisiones, Conferencias clínicas y clínico-patológicas, Diagnóstico y Tratamiento). En estos artículos se ponen al día aspectos de destacado interés clínico o conceptual en la medicina actual. Medicina Clínica es un vehículo de información científica de reconocida calidad, como demuestra su inclusión en los más prestigiosos y selectivos índices bibliográficos del mundo.
Current Contents/Clinical Medicine, Journal Citation Reports, SCI-Expanded, Index Medicus/Medline, Excerpta Medica/EMBASE, IBECS, IME, MEDES, PASCAL, SCOPUS, ScienceDirect
Ver másEl factor de impacto mide la media del número de citaciones recibidas en un año por trabajos publicados en la publicación durante los dos años anteriores.
© Clarivate Analytics, Journal Citation Reports 2022
SJR es una prestigiosa métrica basada en la idea de que todas las citaciones no son iguales. SJR usa un algoritmo similar al page rank de Google; es una medida cuantitativa y cualitativa al impacto de una publicación.
Ver másSNIP permite comparar el impacto de revistas de diferentes campos temáticos, corrigiendo las diferencias en la probabilidad de ser citado que existe entre revistas de distintas materias.
Ver más
Medicina Clínica sigue las recomendaciones para la preparación, presentación y publicación de trabajos académicos en revistas biomédicas
¿Es usted profesional sanitario apto para prescribir o dispensar medicamentos?
Are you a health professional able to prescribe or dispense drugs?
Você é um profissional de saúde habilitado a prescrever ou dispensar medicamentos