The discovery and widespread use of different SARS-CoV-2 vaccines has made it possible to combat the COVID-19 disease in an effective and safe way. Among the adverse effects that have been observed during the implementation of the vaccination campaign is the appearance of thrombosis and bleedings associated with a syndrome known as Vaccine-Induced Thrombotic Thrombocytopenia (VITT), related only to viral vector vaccines. VITT is more frequent in young women and appears to be a phenomenon similar to heparin-induced thrombocytopenia and have an autoimmune source.1,2
Pituitary apoplexy, described as an infarction or hemorrhage of the pituitary gland, is a rare entity generally associated with pituitary adenomas and constitutes, in most cases, an endocrine emergency that may require decompressive surgery and specific treatment. Currently, in the context of SARS-CoV-2 infection, rare and specific cases of pituitary apoplexy have been described both associated and not associated with pituitary adenomas. However, to date, there have been no reported cases of vaccine-associated pituitary apoplexy.3
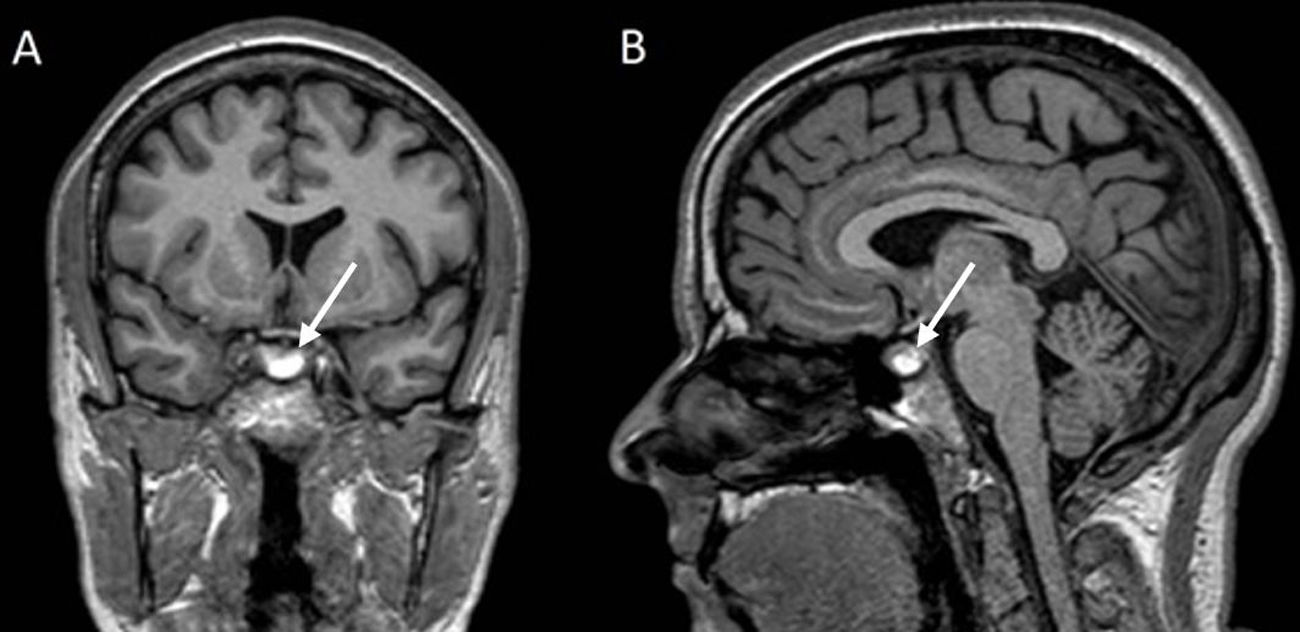
We present the case of a 37-year-old woman who, 5 days after vaccination with ChAdOx1-S, developed a high-intensity frontal headache with partial relief with habitual analgesia. A complete physical examination was performed, which did not demonstrate the presence of neurological focality, cranial nerve involvement, or campimetric involvement. Despite this, due to the intensity of the headache, a brain MRI was performed (Fig. 1). It showed signs concordant with adenohypophysis hemorrhagic bleeding in association with a possible 10mm intraglandular adenoma without chiasmatic involvement. The patient did not present syndromic signs consistent with Cushing's disease or acromegaly, nor did she present symptoms or signs of pituitary hormonal deficits prior to the event. A campimetry and a pituitary hormonal analysis were performed, both yielding normal results. Symptoms were resolved within 2–3 weeks with no complementary treatment and without associated hormonal deficits in that period.
To our knowledge, this is the first case of pituitary hemorrhage described after SARS-CoV-2 vaccination. The possible presence of a previous undiagnosed adenoma could have influenced the appearance of a hemorrhagic phenomenon at this level. Unfortunately, a hemogram was not performed at the time of the event, so we could not confirm the presence of thrombocytopenia that would reinforce the association between pituitary bleeding and vaccination in the context of VITT. At the time of our evaluation, two months later, the patient had a normal blood count without observing this abnormality. In this context, we cannot affirm the correlation between both phenomena, although the temporal evolution of the clinical picture and the radiological findings in which evidence of acute bleeding was denoted does make us consider this case as probably associated with vaccination.4 Generally, the evaluation of headache after SARS-CoV-2 vaccination in the context of screening for cerebral sinus thrombosis is carried out through a cranial CT scan. In this type of examination, the pituitary area is difficult to evaluate, especially when small bleeds occur without hormonal and/or campimetric repercussions, such as in the case presented. Therefore, these types of entities may be underdiagnosed.
In conclusion, we suggest that this case should be taken into account for the evaluation of postvaccinal headache and the possibility of VITT, evaluating campimetric compromise and the possibility of hormonal deficits, both in patients with known pituitary adenomas and in cases without prior diagnosis. Despite not having occurred in our case, the development of an undiagnosed pituitary hormonal deficiency can lead to a torpid evolution.
Patient consentInformed consent has been obtained from the patient for publication of the case report and accompanying images.
Funding resourcesThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Conflict of interestThe authors declare no conflict of interests.