The emerging infectious disease caused by severe acute respiratory syndrome coronavirus 2 (COVID-19), has generated a pandemic situation that has caused the collapse of health systems around the world. In this context, a decrease has been observed in the care activities of other diseases, including patients with acute coronary syndrome.1,2 The backlog in medical assessments, transfer and care difficulties in collapsed hospitals, and the decrease in consultations in the emergency departments due to fear of the health situation, have somehow been able to condition the profile of the patient who consulted for coronary events,3,4 their evolution and their prognosis.
A prospective, single-centre, observational cohort study was conducted in a tertiary hospital. Two groups of patients were included: those who were admitted for a coronary event during the COVID-19 pandemic, without suffering from the infection (February-April 2020), and those hospitalised for a coronary event during the same time interval the previous year (February–April 2019).
Epidemiological, clinical, analytical and prognostic variables considered clinically relevant were collected during hospitalisation. A total of 161 patients were screened: 87 in the pre-COVID-19 interval and 74 in the COVID-19 interval. The study objective was the comparison of these variables between both groups, as well as the analysis of prognostic differences in terms of mortality and cardiovascular events (stroke, reinfarction and new revascularisation).
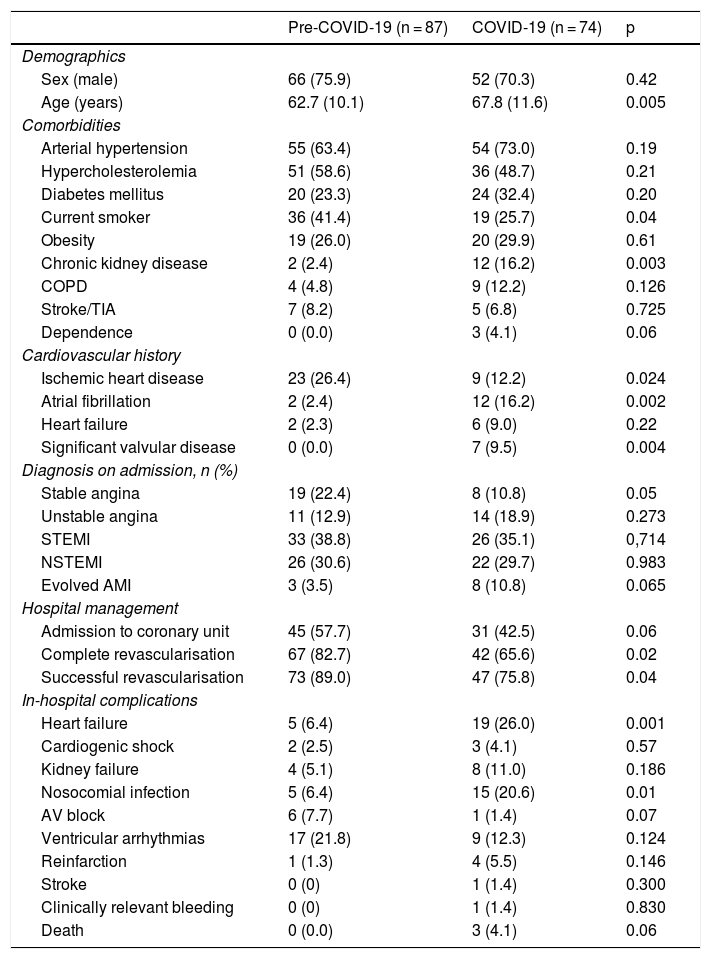
Table 1 shows the baseline characteristics of the population, as well as the differences in the defined prognostic variables. It can be seen that the mean age of the patients was higher in those admitted during the pandemic, and also hospitalisation was more frequent in patients with a history of coronary disease (14.3% vs. 20.3%; p = 0.02), atrial fibrillation (2.4% vs. 16.2%; p = 0.002), significant valvular heart disease (0.0% vs. 9.5%; p = 0.004) and chronic kidney disease (2.4% vs. 16.2%; p = 0.003).
Characteristics of patients hospitalised for coronary events in the pre-COVID-19 period vs. during the COVID-19 pandemic.
| Pre-COVID-19 (n = 87) | COVID-19 (n = 74) | p | |
|---|---|---|---|
| Demographics | |||
| Sex (male) | 66 (75.9) | 52 (70.3) | 0.42 |
| Age (years) | 62.7 (10.1) | 67.8 (11.6) | 0.005 |
| Comorbidities | |||
| Arterial hypertension | 55 (63.4) | 54 (73.0) | 0.19 |
| Hypercholesterolemia | 51 (58.6) | 36 (48.7) | 0.21 |
| Diabetes mellitus | 20 (23.3) | 24 (32.4) | 0.20 |
| Current smoker | 36 (41.4) | 19 (25.7) | 0.04 |
| Obesity | 19 (26.0) | 20 (29.9) | 0.61 |
| Chronic kidney disease | 2 (2.4) | 12 (16.2) | 0.003 |
| COPD | 4 (4.8) | 9 (12.2) | 0.126 |
| Stroke/TIA | 7 (8.2) | 5 (6.8) | 0.725 |
| Dependence | 0 (0.0) | 3 (4.1) | 0.06 |
| Cardiovascular history | |||
| Ischemic heart disease | 23 (26.4) | 9 (12.2) | 0.024 |
| Atrial fibrillation | 2 (2.4) | 12 (16.2) | 0.002 |
| Heart failure | 2 (2.3) | 6 (9.0) | 0.22 |
| Significant valvular disease | 0 (0.0) | 7 (9.5) | 0.004 |
| Diagnosis on admission, n (%) | |||
| Stable angina | 19 (22.4) | 8 (10.8) | 0.05 |
| Unstable angina | 11 (12.9) | 14 (18.9) | 0.273 |
| STEMI | 33 (38.8) | 26 (35.1) | 0,714 |
| NSTEMI | 26 (30.6) | 22 (29.7) | 0.983 |
| Evolved AMI | 3 (3.5) | 8 (10.8) | 0.065 |
| Hospital management | |||
| Admission to coronary unit | 45 (57.7) | 31 (42.5) | 0.06 |
| Complete revascularisation | 67 (82.7) | 42 (65.6) | 0.02 |
| Successful revascularisation | 73 (89.0) | 47 (75.8) | 0.04 |
| In-hospital complications | |||
| Heart failure | 5 (6.4) | 19 (26.0) | 0.001 |
| Cardiogenic shock | 2 (2.5) | 3 (4.1) | 0.57 |
| Kidney failure | 4 (5.1) | 8 (11.0) | 0.186 |
| Nosocomial infection | 5 (6.4) | 15 (20.6) | 0.01 |
| AV block | 6 (7.7) | 1 (1.4) | 0.07 |
| Ventricular arrhythmias | 17 (21.8) | 9 (12.3) | 0.124 |
| Reinfarction | 1 (1.3) | 4 (5.5) | 0.146 |
| Stroke | 0 (0) | 1 (1.4) | 0.300 |
| Clinically relevant bleeding | 0 (0) | 1 (1.4) | 0.830 |
| Death | 0 (0.0) | 3 (4.1) | 0.06 |
Data are presented as number and percentage and as mean and standard deviation.
TIA: transient ischemic attack; ARA II: angiotensin II receptor antagonist; AV: atrioventricular; COPD: chronic obstructive pulmonary disease; AMI: acute myocardial infarction; STEMI: ST-segment elevation myocardial infarction; NSTEMI: Non-ST-segment elevation myocardial infarction; ACEI: angiotensin converting enzyme inhibitor.
During the pre-COVID-19 time period, a higher incidence of stable angina was highlighted (19 [22.4%] vs. 8 [10.8%], p = 0.05), compared to the pandemic period where there was a higher incidence of admissions due to advanced heart attack (3 [3.5%] vs. 8 [10.8%], p = 0.065).
In-hospital management, a lower percentage of complete revascularisations (82.7% vs. 65.6%; p = 0.02) and successful revascularisations (89.0% vs. 75.8%; p = 0.04) were detected during the health emergency.
Regarding the evolution during hospitalisation, the development of heart failure (6.4% vs. 26.0%; p = 0.001) and nosocomial infection (6.4% vs. 20.6%, p = 0.01) was more frequent in the group that was admitted during the pandemic. In this group, a higher incidence close to significance was observed in in-hospital mortality (0.0% vs. 4.1%; p = 0.06). The presence of complications (cardiovascular mortality during hospitalisation, cardiogenic shock, reinfarction, heart failure, ventricular arrhythmias and acute renal failure) was more frequent (26.9% vs. 42.5%; p = 0.045) in admissions during the health emergency.
In the multivariate logistic regression analysis, it was observed that the combined event of in-hospital complications occurred in 51 patients (34.4%). The variables that were independently associated with this event were: admission during the pandemic (odds ratio [OR] = 2.19 [95% confidence interval —95% CI—: 0.98–4.87], p = 0.049); acute ST-segment elevation myocardial infarction [OR = 2.37 (95% CI 1.10–5.11), p = 0.028]; critical unit hospitalisation (OR = 5.02 [95% CI: 2.13–11.82]; p < 0.001) and chronic kidney disease (OR = 5.67 [95% CI: 1.50–21.36]; p = 0.010). A ROC analysis of the binary model sensitivity and specificity for the classification of in-hospital complications was performed, resulting in the area under the ROC curve of 0.756 (95% CI: 0.673–0.838).
The results of this study showed a reduction in admissions due to coronary events during the health emergency time period, in line with other published studies.2 Likewise, it was identified that the profile of the patient who visited a doctor for ischemic heart disease during the pandemic was more fragile and multi-pathological: patients with a higher mean age, more comorbidities, and a higher degree of dependence.
This different profile may explain, in part, the higher number of cardiovascular complications that were recorded during the pandemic. Another reason that may justify this circumstance could be the increase in the rates of unsuccessful and incomplete revascularisation, and the higher incidence of advanced heart attacks.5
The study limitations include the sample size, retrospective design, and possible selection bias, by including only patients admitted to the cardiology department.
Please cite this article as: Carrión-Sánchez I, Gutiérrez-Ortiz E, Gómez-Polo JC. Hospitalizaciones por eventos coronarios durante la pandemia por SARS-CoV2. Med Clin (Barc). 2021;156:191–192.