In the current SARS-CoV-2 pandemic, the use of drugs such as hydroxychloroquine (HQ), azithromycin (AZ), lopinavir/ritonavir (LR) and combinations of these have been shown to have an increased risk of QT interval prolongation1 and caution should be exercised in older patients with polypharmacy and especially with psychotropic drug use.2
Acquired long QT syndrome (ALQTS) is an alteration of ventricular repolarization characterized by a prolonged QT interval heart rate-corrected on the electrocardiogram (ECG), that is, ≥470 milliseconds (ms) in females and ≥450 more in males.3 Drug-induced ALQTS has been a longstanding indicator of increased risk of ventricular arrhythmias, such as polymorphic ventricular tachycardia (Torsade de Pointes) and has been associated with increased mortality. Among the most frequent pharmacological causes to be highlighted in the elderly population are the following drugs: neuroleptics or antipsychotics, antiarrhythmic drugs and antibiotics.2
This letter aims to describe a geriatric population sample with QT prolongation after treatment for SARS-CoV-2 infection based on a comprehensive geriatric assessment and its association with mortality. Patients over 75 years of age admitted to a COVID-19 Geriatric Unit (CGU) from 20 March to 31 May 2020 with a diagnosis of SARS-CoV-2 infection by PCR confirmation or with high clinical-radiological suspicion were included. All patients with ECG recording were analysed considering the measurement of the QT interval at 48h after initiating any type of medical treatment for SARS-CoV-2. The corrected QT was calculated using the Bazett formula, considering a prolonged corrected QT≥470ms for women and ≥450 more for men. Variables such as physical and mental function, comorbidity (Charlson index: high comorbidity, ≥3), polypharmacy (in number [≥5 and extreme ≥10] and drug typology), mortality and the risk of mortality associated with sepsis (QSOFA≥2) were analysed.
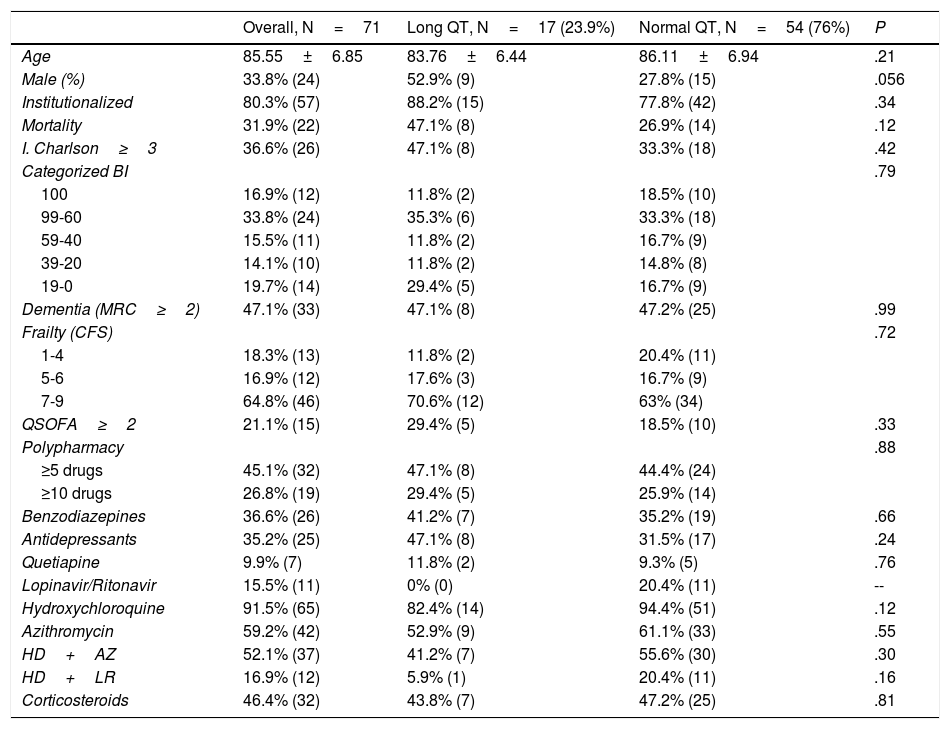
The results (Table 1) evaluated a total of 71 individuals with ECG recording. The mean age was 85.55±6.85 years; 66.2% women. 23.9% had QT prolongation (8 women and 9 men). The mean QT was 428.57±47.46ms (228−565ms) at 48h after initiation of any therapy for SARS-CoV-2 infection regarding the heart rhythm of the sample, 85.9% were in sinus rhythm, 11.3% in atrial fibrillation and 2.8% in pacemaker rhythm.
Baseline Characteristics of Patients with ECG Recording Based on Normal and Long QT.
| Overall, N=71 | Long QT, N=17 (23.9%) | Normal QT, N=54 (76%) | P | |
|---|---|---|---|---|
| Age | 85.55±6.85 | 83.76±6.44 | 86.11±6.94 | .21 |
| Male (%) | 33.8% (24) | 52.9% (9) | 27.8% (15) | .056 |
| Institutionalized | 80.3% (57) | 88.2% (15) | 77.8% (42) | .34 |
| Mortality | 31.9% (22) | 47.1% (8) | 26.9% (14) | .12 |
| I. Charlson≥3 | 36.6% (26) | 47.1% (8) | 33.3% (18) | .42 |
| Categorized BI | .79 | |||
| 100 | 16.9% (12) | 11.8% (2) | 18.5% (10) | |
| 99-60 | 33.8% (24) | 35.3% (6) | 33.3% (18) | |
| 59-40 | 15.5% (11) | 11.8% (2) | 16.7% (9) | |
| 39-20 | 14.1% (10) | 11.8% (2) | 14.8% (8) | |
| 19-0 | 19.7% (14) | 29.4% (5) | 16.7% (9) | |
| Dementia (MRC≥2) | 47.1% (33) | 47.1% (8) | 47.2% (25) | .99 |
| Frailty (CFS) | .72 | |||
| 1-4 | 18.3% (13) | 11.8% (2) | 20.4% (11) | |
| 5-6 | 16.9% (12) | 17.6% (3) | 16.7% (9) | |
| 7-9 | 64.8% (46) | 70.6% (12) | 63% (34) | |
| QSOFA≥2 | 21.1% (15) | 29.4% (5) | 18.5% (10) | .33 |
| Polypharmacy | .88 | |||
| ≥5 drugs | 45.1% (32) | 47.1% (8) | 44.4% (24) | |
| ≥10 drugs | 26.8% (19) | 29.4% (5) | 25.9% (14) | |
| Benzodiazepines | 36.6% (26) | 41.2% (7) | 35.2% (19) | .66 |
| Antidepressants | 35.2% (25) | 47.1% (8) | 31.5% (17) | .24 |
| Quetiapine | 9.9% (7) | 11.8% (2) | 9.3% (5) | .76 |
| Lopinavir/Ritonavir | 15.5% (11) | 0% (0) | 20.4% (11) | -- |
| Hydroxychloroquine | 91.5% (65) | 82.4% (14) | 94.4% (51) | .12 |
| Azithromycin | 59.2% (42) | 52.9% (9) | 61.1% (33) | .55 |
| HD+AZ | 52.1% (37) | 41.2% (7) | 55.6% (30) | .30 |
| HD+LR | 16.9% (12) | 5.9% (1) | 20.4% (11) | .16 |
| Corticosteroids | 46.4% (32) | 43.8% (7) | 47.2% (25) | .81 |
AZ: azithromycin; CFS: Clinical Frailty Scale; MRC: Mental health Red Cross; ECG: electrocardiogram; HD: hydroxychloroquine; BI: Barthel index; LR: lopinavir/ritonavir; QSOFA: Quick Sequential Organ Failure Assessment.
Most of the patients came from nursing homes (80.3%). 64.8% met severe frailty criteria and 71.9% polypharmacy, highlighting benzodiazepines (36.6%), quetiapine (9.9%) and antidepressants (35.2%). Regarding the treatment of SARS-CoV-2: 91.5% received HQ, 59.2% AZ and 15.5% LR. The most common combination was HQ with AZ (52.1%), followed by HQ with LR (16.9%). The triple therapy of HQ+AZ+LR was only prescribed in 4.2% (3 patients). 46.4% received corticosteroid therapy and 21.1% had a QSOFA≥2. In-hospital mortality was 31.9%.
In the univariate analysis (Table 1) only the male gender was associated with a tendency to have a prolonged QT; the rest of the variables, including mortality, did not have a statistically significant association in the analysis, unlike other studies in which advanced age, different comorbidities and polypharmacy were related to potential interactions, particularly with LR.4 Despite the limitations of our study, with a small and non-multicentre sample size, we would like to highlight the fact that in our setting, in a typical geriatric population (high frailty, polypharmacy, comorbidity), the usual treatments for SARS-CoV-2 were not associated with a significant prolongation of the QT interval or an increase in mortality that would invalidate their use. Therefore, they can continue to be considered, on an individualised basis and with caution, as a therapeutic tool for these patients.
FundingThis research has not received specific grants from public or private agencies or from non-profit entities.
Conflict of interestsThere are no conflicts of interest on the part of any of the authors.
We wish to thank the entire Cardiology and Geriatrics team of the Central Red Cross Hospital.
Please cite this article as: Garmendia-Prieto B, Carrillo-García P, Gómez-Pavón J. Prolongación del intervalo QT en pacientes geriátricos bajo tratamiento por la infección por SARS-COV-2: estudio OCTA-COVID. Med Clin (Barc). 2021;157:e302–e303.
All authors were involved in the conception and design of the manuscript, data collection, analysis and interpretation of the data, and the writing, review and approval of the submitted manuscript.