Sarcoidosis and primary Sjögren's syndrome are multi-organ autoimmune diseases with similar clinical manifestations. Sjögren's syndrome, a chronic disease, mainly affects the salivary and lacrimal glands and can damage other organs.1 Sarcoidosis is distinguished by the presence of non-caseating granulomatous inflammation and the lung as well as the lymphatic system are the most commonly involved organs.1,2 This case highlights the initial complexity of trying to distinguish COVID-19 lung pathology from sarcoidosis. However, the resolution revealed an even more intricate reality by identifying an overlap with Sjögren's syndrome, thus underlining the need for a comprehensive study in the management of systemic diseases. Consequently, we believe that the presentation of this case is essential to provide a valuable clinical perspective for the management of similar situations.
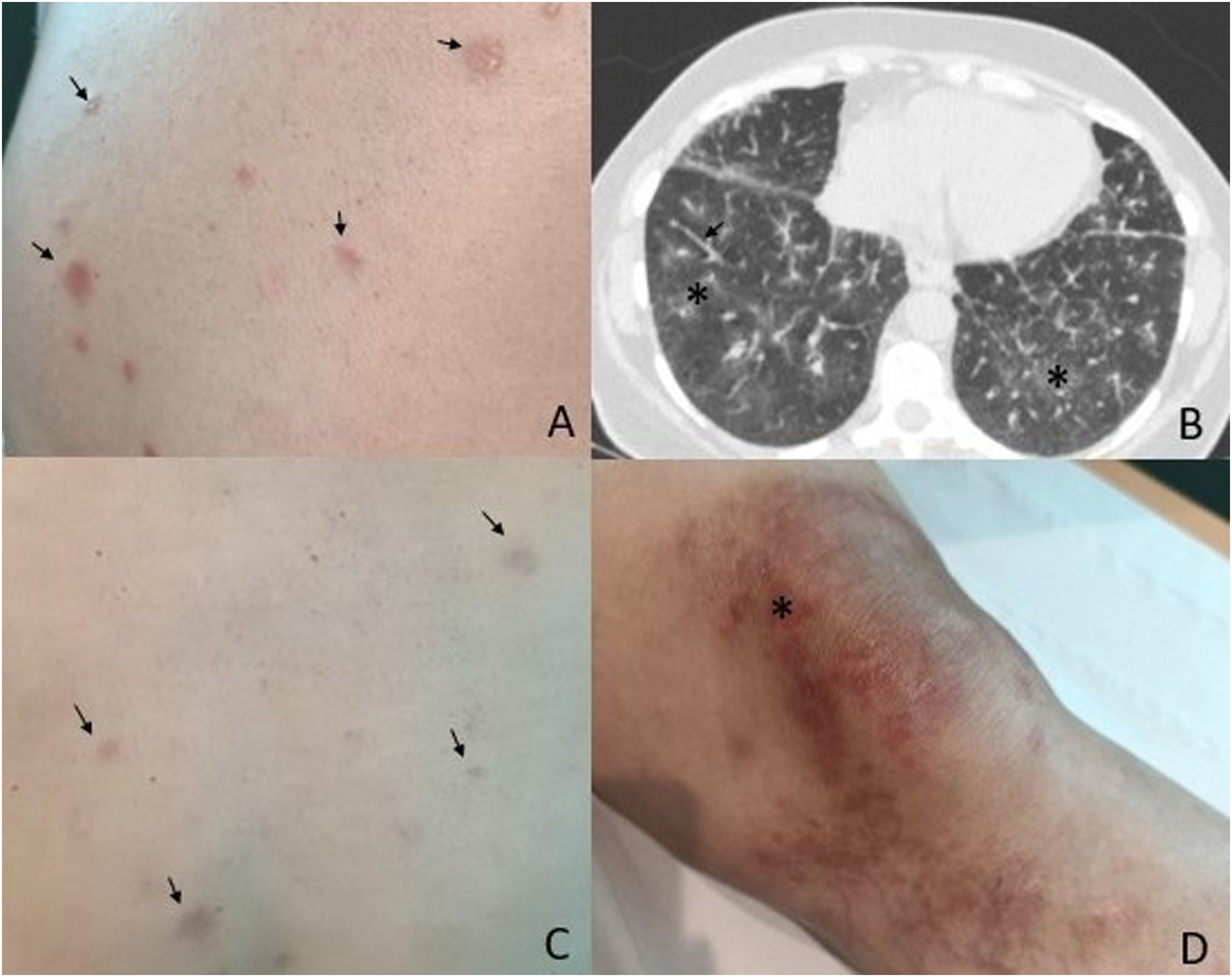
This paper reports the case of a 54-year-old woman of Bulgarian descent who presented with clinical symptoms following an episode of COVID-19 infection in 2021 and who sought medical advice 18 months after infection. She reported progressive dyspnoea on exertion, dry cough and arthralgia with the appearance of skin lesions in the last two months. On examination she had bibasilar crackles and swelling on both knees with erythematous brownish papular lesions with a tendency to coalesce, granulomas on the back and facial telangiectasias (Fig. 1). She reported no ocular, cardiac or gastrointestinal lesions. She reported dry mouth but no dry eyes. There was no constitutional syndrome or fever.
A) Granulomas on the back at the time of diagnosis (arrow). B) HRCT of the chest showing bilateral interstitial involvement (asterisk) and reticular thickening (arrow). C) Improvement of granulomas after two months of treatment (arrow). D) Papules of the knee where the biopsy specimen was taken (asterisk).
HR-CT: high resolution computed axial tomography.
Tests revealed significant findings, with interstitial involvement and reticular thickening, as well as mediastinal lymphadenopathy on high-resolution computed tomography (CT) that was compatible with both COVID and sarcoidosis (Fig. 1). Respiratory function tests showed a moderate decrease in carbon monoxide diffusing capacity (DLCO) and restrictive ventilatory impairment. Laboratory tests showed calcium levels of 10.69mg/dL (normal range: 8.5–10.2mg/dL) with normal parathyroid hormone (PTH), polymerase chain reaction (PCR): 8.68mg/L (normal<6mg/L), erythrocyte sedimentation rate (ESR): 59mm (normal<20mm), normal angiotensin converting enzyme (ACE), rheumatoid factor: 104U/mL (positive if>20U/mL), negative anti-citrullinated antibodies (Ac), antinuclear antibodies (ANA)+1/1.280 with positive anti-Ro-52, anti-Ro-60 and anti-SSB antibodies (anti-SSB); negative anti-dsDNA, negative scleroderma and myositis profile; immunoglobulin G (IgG): 2.360mg/dL (normal range: 768−1632mg/dL) and IgA: 672mg/dL (normal range: 68–378mg/dL). Serologies for hepatitis, human immunodeficiency virus (HIV) and syphilis were negative, as was the Mantoux test. A bronchoalveolar lavage was performed with a CD4/CD8 ratio (bronchoalveolar lavage) of 6.75, and cytology results were negative for malignancy. Additional tests, including Gram staining and aerobic, mycobacterial and fungal cultures, were also negative. In the skin biopsy of the knee, histopathology revealed a non-necrotising granulomatous dermatitis compatible with sarcoidosis. Salivary gland scintigraphy was compatible with Sjögren syndrome.
Skin biopsy of the knee confirmed the presence of non-necrotising granulomatous dermatitis, thus supporting the diagnosis of sarcoidosis. This diagnosis was established through histological confirmation and the exclusion of other diseases that may have manifested in a similar manner.3 It is important to note that there are no specific diagnostic or classification criteria for sarcoidosis other than histological assessment, clinical evaluation and compatible imaging tests.3 Salivary gland scintigraphy was compatible with glandular hypofunction, and a diagnosis of sarcoidosis with overlapping Sjögren's syndrome was established, the latter confirmed by immunological criteria (anti-Ro and anti-SSB antibodies), clinical criteria (dry mouth) and scintigraphy with glandular hypofunction as described in the classification criteria American College of Rheumatology/European League Against Rheumatism (2002).4
Treatment was started with prednisone 30mg/day on a tapering regimen, and improvement was observed after two months, both on pulmonary auscultation, with a decrease in crackles, and on the skin and blood tests, with a decrease in acute phase reactants. Hydroxychloroquine 200mg/day was subsequently added as a glucocorticoid-sparing agent.
A review of the literature reveals limited research reporting on the coexistence of sarcoidosis and Sjögren's syndrome although, where described, there is a higher prevalence of joint involvement, ocular involvement and positive ANA, rheumatoid factor and anti-Ro/SSA results.2 However, a 2017 report from Taiwan, which looked at a study of autoimmune diseases involving 1237 patients diagnosed with sarcoidosis, found a significant association between sarcoidosis and Sjögren's syndrome (adjusted odds ratio 11.6; 95% confidence interval [CI]: 4.36–31).5
Ethical considerationsOral and written consent was obtained from the patient for publication of the photographs and article.
FundingThis research has not received specific support from public, private or non-profit entities.
Conflict of interestThe authors declare that they have no conflict of interest.