Acute leukemia (AL) is the most common malignant disease in children, and one of the most important causes of death in pediatric age. For practical purposes, one in three children with cancer has AL, and three to four new cases occur each year per 100,000 children under 15 years of age. In Mexico, there are about 1000 new cases diagnosed per year, so the pediatrician and family physician ideally need tools that allow for early diagnosis.1
There are a series of important prognostic factors, particularly in acute lymphoblastic leukemia (ALL), which is the variety that explains 85–90% of all cases of leukemia in children. This factors allow us to make a distinction between at least three risk groups for relapse of the disease, namely, low risk, standard risk and high risk. Each of these three groups receives different chemotherapy treatment protocols; children at high risk receive the most intense treatment and those at low risk are in turn easier to handle and less likely to generate complications.2
It is clear, that to offer the most appropriate treatment for each of the children, it is essential to carry out this distinction of risk groups and prevent a patient at low risk of relapse from receiving an intense treatment that exposes them to unnecessary toxic effects, and also preventing a high risk patient from receiving an insufficient chemotherapy scheme, which would significantly reduce their chances of being cured. It should be stressed that these prognostic factors are not life-or-death sentences, just elements that allow us to offer the best possible treatment for each patient.
These risk factors can be divided into three groups: those having to do with the characteristics of neoplastic cells, those having to do with treatment response and those having to do with the characteristics of each patient. A very important example regarding neoplastic cells is referred to as the presence of the Philadelphia chromosome (Ph+). If a child with this condition receives a standard treatment, the chances of being cured are almost 0%, while a treatment that includes tyrosine kinase inhibiting drugs, such as imatinib, significantly increase the chances of a cure.
Regarding treatment response, as with virtually any disease, patients who respond well to chemotherapy protocols are more likely to be cured. This response assessment can be carried out in different ways. One of the most commonly used assessments around the world was proposed by a German group almost 20 years ago. In it, children with ALL initially receive 7 days of treatment solely with corticosteroids. If at the end of this week the patient has less than 1000 blast cells per mm3 in their peripheral blood it is considered a favorable response and these children's chances of being cured are set higher. If, on the contrary, the patient's leukemic cells are not reduced below this figure, it will be necessary to administer more intense treatment protocols. Fortunately these cases are less frequent in most populations.
Other institutions perform bone marrow studies, fifteen days after starting treatment. And finally, any location that has one, usually performs a determination of minimal residual disease (MRD) at the end of the first month of treatment, which has been our center's policy for the last eight years. With an MRD, and with the use of monoclonal antibodies, we can quantify the number of neoplastic cells the patient has at the end of the first month of treatment with certainty. In this manner, we can objectively evaluate 500,000 or more cells and determine if the patient has <0.1×104 leukemic cells per mm3, which is to say, less than 1 malignant cell for every 10,000 evaluated. When the MRD is negative, the possibility of being cured increases, otherwise, the patient should be treated with more intense chemotherapy protocols and even consider a hematopoietic progenitor cell transplant. Previously, the patient would be evaluated after one month of treatment to see if he had achieved complete remission (less than 5% blasts in the bone marrow study) by a morphological review conducted by the hematologist after observing between 500 and 1000 cells by microscope. This was an “operator dependent” method and was therefore less accurate.
The pediatrician and primary care physicians do not have any participation in the workup mentioned above, i.e., the cytogenetic characteristics or immunophenotype markers are beyond the reach of many of us, and response to treatment protocol that is used depends mainly on the hematologist. In addition, they cannot influence the prognostic factors that depend on patient characteristics, such as gender (the prognosis is slightly better in women), race (the Anglo-Saxon population shows better results than blacks or Hispanics, which is determined, among other factors, by specific genetic alterations) and age at diagnosis (children between one and nine years old have the best outlook).
The early suspicion of a diagnosis is the only prognostic factor that a pediatrician or primary care physician can influence, and therefore has an influence on the absolute leukocyte number in the initial blood count (BH) being less than 50,000/uL, most medical groups accept that children diagnosed with less than this figure have a better prognosis than those with higher counts, which are associated with an increased risk of relapse and should receive more intense chemotherapy schemes.
What happens when a child is diagnosed with more than 50,000 white blood cells per microliter? Initially, they will be included in the group of patients receiving more intensive treatment, which is usually more toxic and more likely to develop complications, with an increased risk of presenting infiltration to the central nervous system and also in developing serious complications in the early days of treatment, such as tumor lysis syndrome. In effect, the fact of having more than 50,000 white blood cells per microliter at diagnosis is associated with a smaller possibility of a cure.
In children with less than 50,000 leukocytes at diagnosis and without other adverse prognostic factors, a cure rate of up to 80% can be achieved. In a group of patients with more than 50,000 leukocytes at diagnosis, the chances of being cured would be reduced to 50%. It is important to note that many times the course of the disease is so fast that, however early it is suspected and the necessary workup measures carried out, a patient with ALL can present with very high leukocyte counts from the beginning.
Most of the time, the diagnosis of ALL revolves around the complete blood count (CBC), because of the clinical situations which result in requesting them, as well as the significant interpretation data that can be derived from it.3
The following are the instructions for requesting a CBC in children.
Anemic syndromeThe vast majority of patients with anemic syndrome (fatigue, weakness, paleness, hyporexia, headache, etc.) will have a different diagnosis than leukemia. In fact, the diagnosis will be iron deficiency anemia over 90% of the time. However a CBC should still be requested. It is important to mention that to continue considering a diagnosis of iron deficiency anemia, the anemia should be microcytic and hypochromic, with high RDW, and normal to elevated leukocytes, and platelets. In fact, if in addition to the above, the patient shows a low percentage of reticulocytes (which are rarely requested), the diagnosis of iron deficiency anemia has a high degree of certainty without the need for any other test.
Purpuric syndromeA child with mucosal bleeding and manifested petechiae, ecchymosis, or epistaxis, requires a CBC. In these cases, most patients will have an immune thrombocytopenic purpura. It is important to note that these patients are basically “healthy” children who only have purpuric syndrome and a low platelet count in the CBC. Everything else is normal, the child has no fever, no weight loss, and no hyporexia, adenopathy, splenomegaly or bone pain.
Bone painOne in four children with ALL manifest bone pain. It should be mentioned that the most common cause of pain in children are growing pains. An 80% of children with growing pains refer them in the lower limbs, and as being symmetrical, very intense, lasting a short time and, most importantly, recurring weeks or even months later. So with any other type of bone pain in children, ALL should be considered and a CBC should be requested.
SplenomegalyAll children with a palpable spleen should get a CBC, without exception. Among the most common causes for splenomegaly in children are viral infections. Regardless of how it is discovered, once splenomegaly is noted, a CBC should be performed and the diagnosis of ALL should be excluded.
FeverConsidering the large number of children who have a fever, when would the fever call for doing a CBC? If the patient has three or more days of fever without clinical improvement; or has several febrile episodes in a short period of time, or if along with fever, the patient shows any of the aforementioned conditions (anemic or purpuric syndrome, bone pain and splenomegaly), then he should receive a CBC.
It should be made clear that to request a CBC in any of the situations mentioned above does not mean that the child has ALL. Requesting a CBC simply allows us to make a timely diagnosis. Regarding the proper interpretation of the CBC, it should consider a number of very important data. For example, four out of five patients with acute leukemia have anemia, which is normocytic and normochromic, so the diagnosis should not be excluded just because the patient does not have anemia.4 Also, one in five children with ALL has no thrombocytopenia in the same way that occurs with anemia, so having a normal platelet count does not exclude the diagnosis.
Pancytopenia is defined as, upon performing a CBC, having a diminished hemoglobin, platelets and leukocyte count. That is, affecting all three cell lines simultaneously, and this must be considered a medical emergency, which is to say that the patient must be evaluated with the intention of confirming a diagnosis as quickly as possible, as the majority of children with pancytopenia also have ALL.
It is not difficult to diagnose leukemia or suspect it with a CBC reporting more than 50,000 leukocytes. However, it is very important to consider that 50% of children with ALL present with less than 11,000 leukocytes on an initial CBC, so it should be clear that there can be any white blood cell count in the initial CBC; only 20% of patients have more than 100,000 leukocytes at diagnosis and less than 7% have more than 200,000 per microliter.
Another consideration is related to the common fact that the presence of blasts or immature cells in the leukocyte differential is not reported in the initial CBC; for practical purposes, all cases of ALL are present in the peripheral blood at diagnosis. The reasons they are not reported are, among others, a lack of experience on the part of the smear's observer, a lack of certainty in reporting them, and the presence of a reduced number of them, especially in cases with low leukocyte counts. It is also important to note that blasts are very often reported as atypical lymphocytes, and appear to be handled as synonyms despite their different origins. It is also common for reports to include terms such as “immature”, “ugly” or “suspicious”, leading to the aforementioned fact that even though no blasts are reported in the CBC, the diagnosis of ALL should not be discarded.
Most of the time, the diagnosis of ALL is not very complicated for hematologists, because they can count on the use of bone marrow aspirates for suspected cases. The problem is that patients must come to the clinic for that study. Another important factor is the lack of communication between the doctor and the laboratory personnel; the staff is usually more interested in a case in which the doctor tells them about suspected acute leukemia.
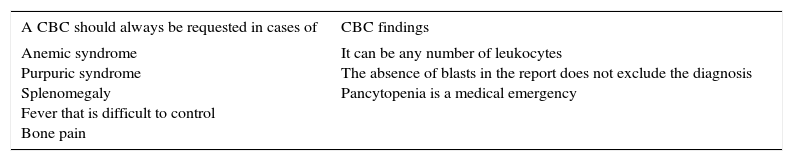
Finally, we must re-emphasize the following data (Table 1):
Leukemia is the most common cancer in children and is among the leading causes of death in Mexico. It is clear that this data is sufficient for the pediatrician to familiarize himself with this disease.
The important role of the pediatrician is in the early diagnosis of ALL.
Request a CBC in all cases of children with anemic syndrome, purpuric syndrome and splenomegaly. CBC should also be considered in children with bone pain that does not appear to be growth-related and in children with a fever that is long-standing and unresponsive to conventional treatments.
Pancytopenia should be considered a medical emergency.
The leukocytes count in ALL can be low, normal or high.
The absence of “blasts” or “immature cells” in the CBC report do not exclude a diagnosis of acute leukemia.
CBC requests and findings.
| A CBC should always be requested in cases of | CBC findings |
|---|---|
| Anemic syndrome Purpuric syndrome Splenomegaly Fever that is difficult to control Bone pain | It can be any number of leukocytes The absence of blasts in the report does not exclude the diagnosis Pancytopenia is a medical emergency |
Carrying out a timely diagnosis for ALL results in a better prognosis, and considering what has been referred in this article, the appropriate involvement of the pediatrician or primary care physician is of great importance for the course and outcome of children with this disease.
Ethical disclosuresProtection of human and animal subjectsThe authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of dataThe authors declare that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that no patient data appear in this article.
FundingNo financial support was provided.
Conflict of interestThe authors have no conflicts of interest to declare.