Dizziness is one of the most common reasons for requesting a neurological consultation, but its underlying pathology cannot be detected in as many as 80% of all cases.1,2 Its estimated prevalence is higher than 20% and increases with age. Dizziness most commonly presents in women.1 In addition, dizziness is reported by 4% of all patients who visit emergency departments. Comparison of aetiologies reveals that up to 30% of these cases are secondary to a serious health problem.3
Dysarthria is also a very common motive for requesting a neurological consultation. However, it is considered a non-specific condition due to its multiple aetiologies. It is a common symptom in cerebrovascular disease, although it may also be indicative of certain neurodegenerative diseases, neuromuscular disorders, or an underlying medical process such as encephalopathy or intoxication.4,5
However, the presence of any of these symptoms, especially if onset is acute, requires careful neurological examination, and in some cases, a neuroimaging study. These symptoms may be indicative of serious clinical processes which are nevertheless potentially treatable.
We present the case of a male smoker aged 53 years who had recently been diagnosed with arterial hypertension and was being treated with beta blockers. He had also been diagnosed with type 2 diabetes mellitus for which he was being treated with metformin; compliance was poor. He sought medical attention due to sudden-onset dizziness, instability with illusion of movement in the visual field (oscillopsia), and speech difficulties occurring in the previous 5 days. Neurological examination revealed moderate dysarthria and inability to walk correctly in tandem gait. The patient was admitted to hospital for a neurological assessment due to the symptoms and ictal episode. Complementary studies (brain CT, echo Doppler study of the supra-aortic trunks (SAT), and brain MRI) showed no signs of acute ischaemia. Doctors were unable to perform a transcranial echo Doppler (TCD) since the ultrasound scanner was not available at that time. Instead, they completed MR angiography of the circle of Willis which revealed a lesion in the distal end of the basilar artery without significant stenosis (<50%). The patient was discharged from hospital after doctors adjusted antihypertensive drugs and added antiplatelet drugs and high doses of statins (80mg of atorvastatin).
Four days later, the patient returned to the emergency department due to exacerbation of the initial symptoms (gait instability with tendency to drift to the right and sudden-onset hearing loss in the right ear). These symptoms were confirmed by the neurological examination, which highlighted the patient's tendency to drift to the right while walking, right-sided hearing loss, mild right-sided dysmetria shown by finger-to-nose test, and persistent dysarthria.
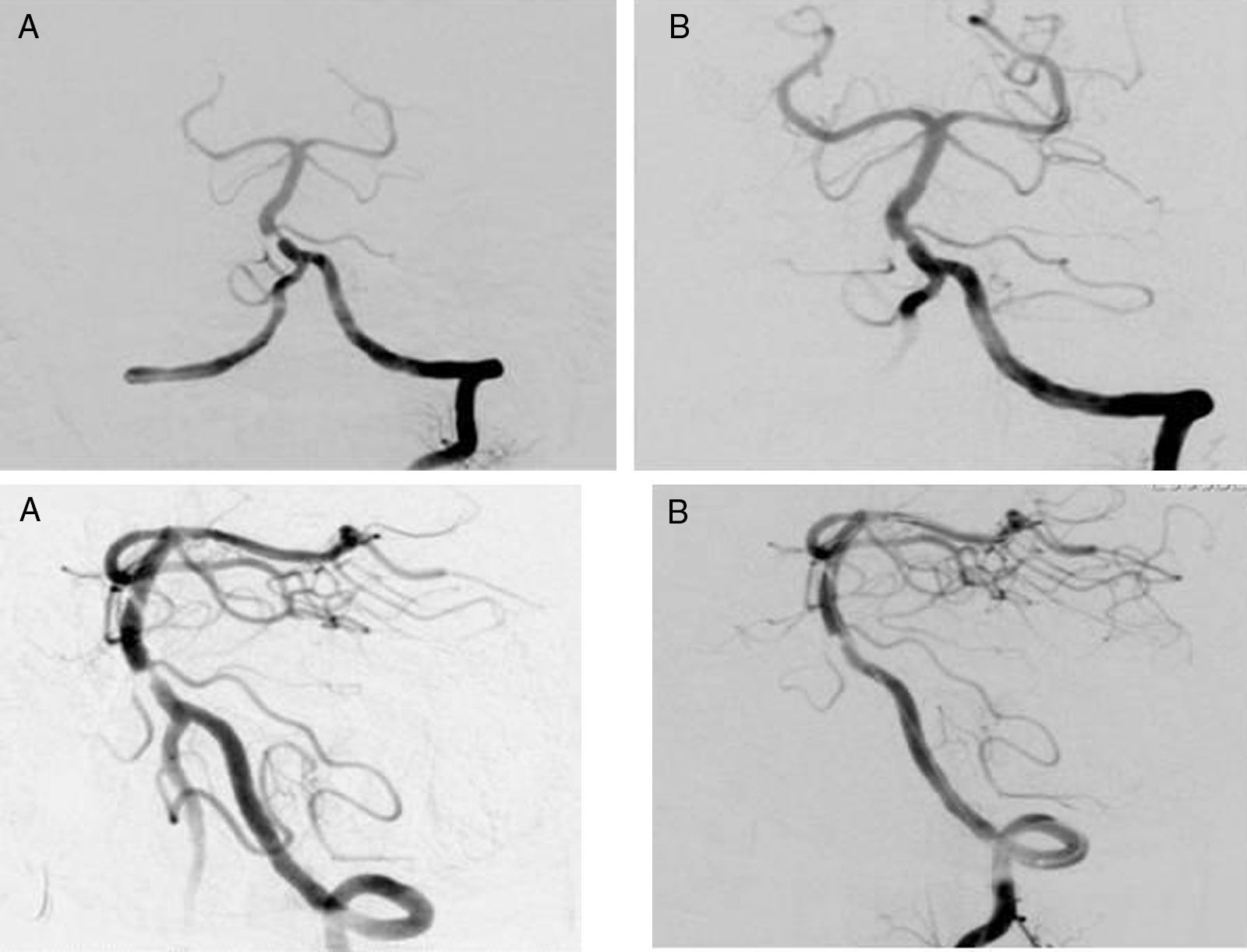
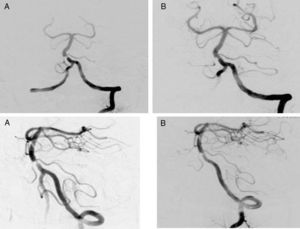
The TCD performed in the emergency department did not record the lower and middle third of the basilar artery. Doctors therefore completed the study with CT angiography of the SAT and circle of Willis, which showed stenosis greater than 80% in lower third of the basilar artery (BA) (Fig. 1). A new brain MRI displayed an acute ischaemic lesion in the territory of the right inferior cerebellar artery. Since the patient's symptoms continued to progress despite proper medical treatment, doctors opted to perform arteriography with angioplasty and have a stent placed in the BA (Fig. 2) in the referral hospital. In order for this to take place, the patient began receiving dual antiplatelet therapy 3 days before surgery and continued with the same treatment for 6 months. The patient's condition improved after placement of the stent. A routine TCD showed sufficient blood flow velocity in the BA, which was confirmed 6 months later by means of arteriography. Clopidogrel was subsequently discontinued.
Cerebral ischaemia related to vertebrobasilar circulation accounts for 20% of all ischaemic strokes.6,7 It usually presents with obvious neurological symptoms, although it may also go undetected, especially in cases of basilar artery stenosis.8 Assessing the vertebrobasilar system (VBS) requires neuroimaging tests. However, examining the VBS and interpreting test results may be more complex than performing a carotid evaluation. Doctors now have ultrasound (US) techniques which have been shown to be useful for assessing posterior circulation. Their other advantages are that they are fast, adaptable, minimally invasive, and require no cooperation from the patient. These features make them ideal for detecting VBS disease.9–11 However, doctors should confirm their findings using more sensitive and specific imaging techniques.12 The time-of-flight MRI is not the best technique for assessing VBS since it may overestimate the degree of arterial stenosis.13 There are currently no studies that directly compare the sensitivity and specificity of contrast-enhanced brain MR angiography with computed tomography angiography (CTA). Doctors use both techniques interchangeably.7 Cerebral arteriography is still considered the gold standard.8–13
An interesting point in our case is the underestimation of the real degree of stenosis in the initial TOF MRI. However, when doctors from the neuroradiology department at the referral hospital analysed the study a second time, they considered the degree of stenosis to be relevant and comparable to CTA results. The initial underestimation is believed to be caused by human error. In addition, when the patient was first admitted to hospital, doctors were unable to assess transcranial VBS using ultrasound, since the TCD scanner was not available. If this procedure had been carried out, results would probably have pointed to a more significant degree of BA stenosis, especially if doctors had used echo enhancers for an optimal view of the BA. We would like to point out the importance of ultrasound techniques since they can be used bedside by neurologists and they permit direct and dynamic assessment of arterial circulation. We would also like to highlight that apparently banal symptoms (dizziness) or non-specific symptoms (dysarthria) should not be underestimated, especially when they are persistent or progressive. Likewise, doctors should perform multiple imaging tests in cases of suspected ischaemia in the territory of the VBS before determining the optimal treatment (medical or surgical) for each patient.
Please cite this article as:: Fernández Domínguez J, et al. Disartria y mareo persistente con estudio neurológico previo: hasta dónde seguir investigando. Neurología. 2013;28:250–2.