Diaphragmatic flutter is a rare condition characterised by rhythmic involuntary contractions of the diaphragm and other respiratory muscles innervated by cervical nerve roots. It has been described in people of all ages and both sexes. Its clinical presentation varies greatly and clinical symptoms are quite unusual, which may result in late diagnoses and ineffective treatments. Symptoms include thoracic or abdominal pain and dyskinetic movements in the thorax and abdominal wall. Idiopathic diaphragmatic flutter is the most common presentation, although it has also been described in association with other clinical and surgical entities. Diagnosis is based on strong clinical suspicion in addition to fluoroscopy or electrophysiological studies showing diaphragm movement. No clinical studies have addressed treatment options for this disorder. Current treatment relies on expert opinion and case reports and may be pharmacological or non-pharmacological.
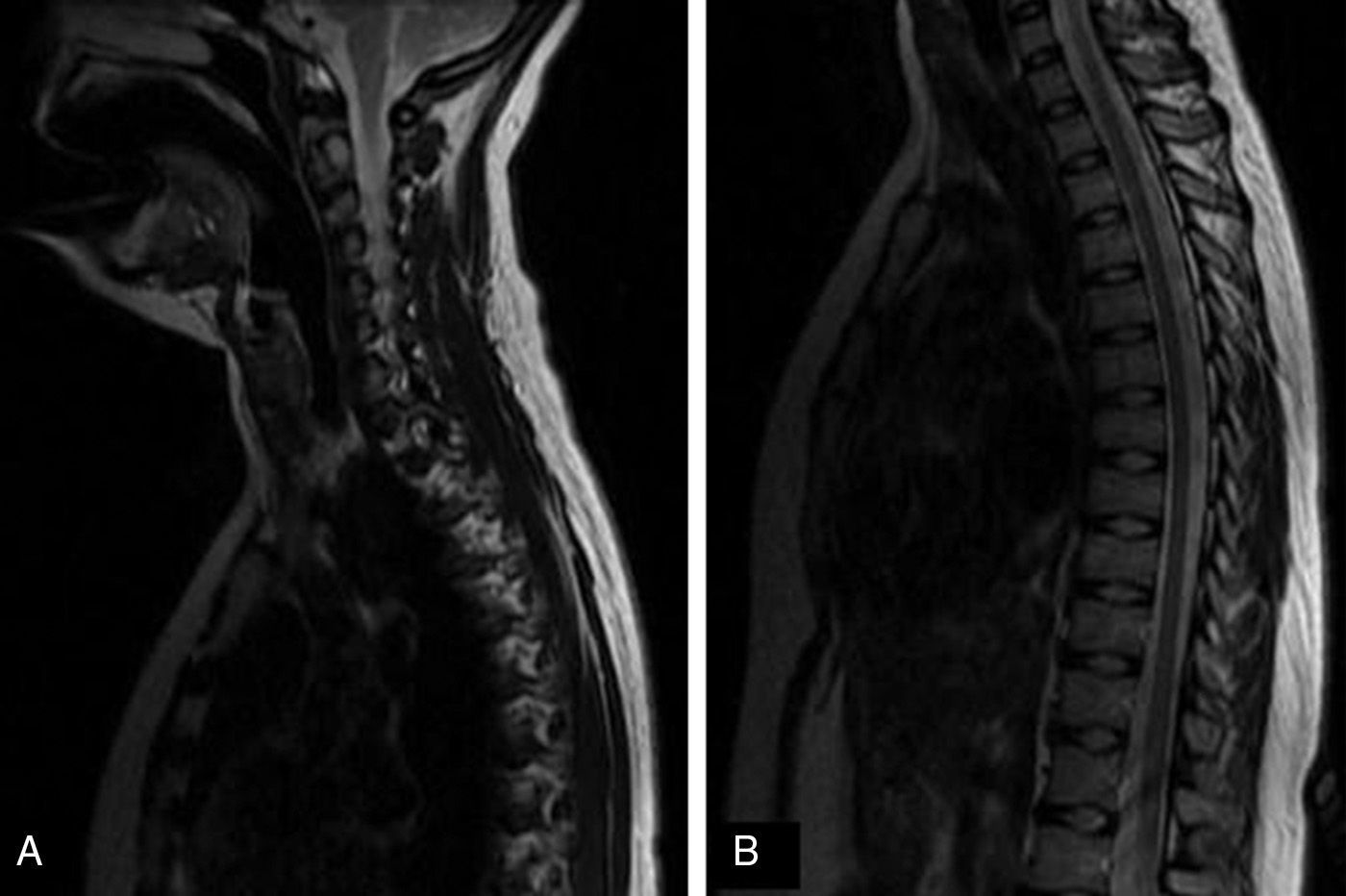
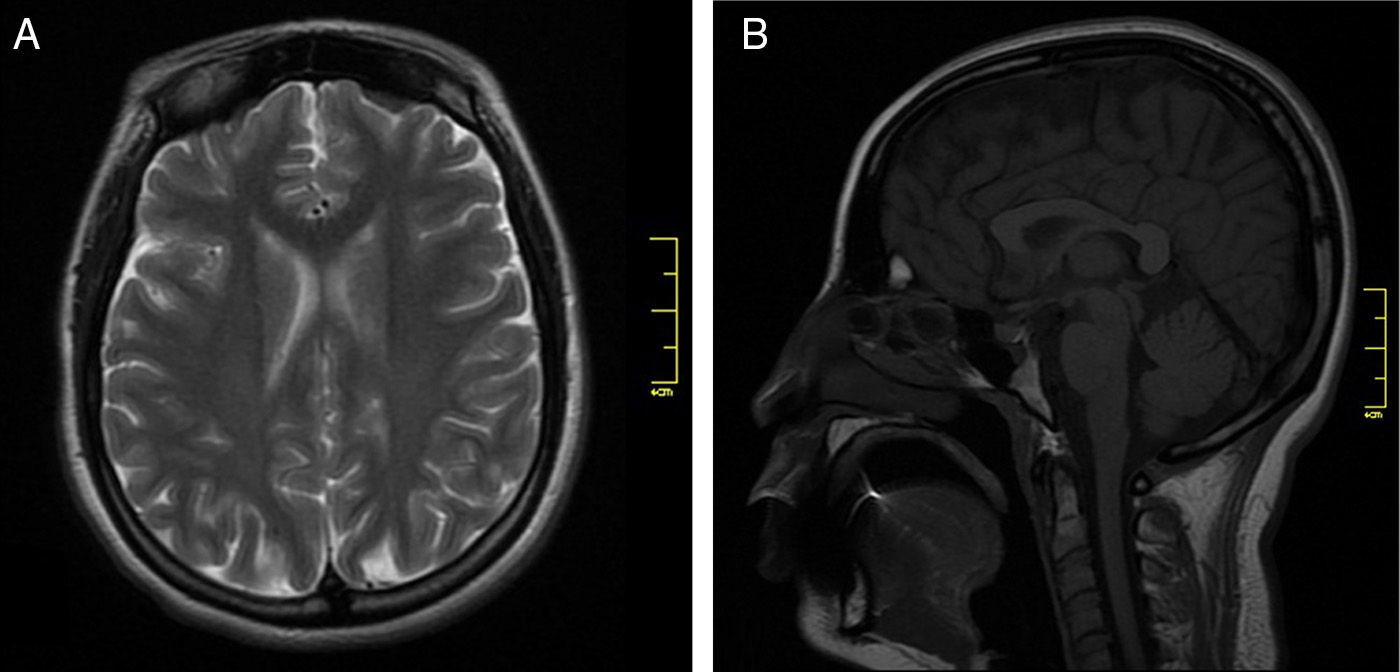
We present the case of a 17-year-old adolescent who experienced sudden onset of pain in the right lumbar region and right iliac fossa which radiated to the back and lasted 45 days. Pain was associated with involuntary movements of the trunk. She was referred to the emergency department by the neurology department due to exacerbation of pain, presence of predominantly right-sided rhythmic involuntary movements of the trunk, nausea, vomiting, and a burning feeling in the right facial and brachial regions and right hemithorax. Our patient had previously been evaluated by several departments at an outpatient clinic, including the neurology, internal medicine, psychiatry, psychology, and rehabilitation and physical medicine departments. She had also undergone neural therapy and physiotherapy, but symptoms did not improve. Findings from contrast and non-contrast MRI studies of the cervical and thoracic spine were normal (Fig. 1). She was treated with fluoxetine 20mg/day and with clonazepam drops; the latter improved her symptoms slightly. Our patient had a history of recurrent urinary infections and mixed anxiety-depressive disorder. She was admitted to the emergency department. Mucosa was hydrated and pink, and vital signs were as follows: blood pressure, 110/60mmHg; heart rate, 78bpm; respiratory rate, 17breaths/min; oxygen saturation, 96%; and no fever. Neurological examination showed that the patient was alert and her higher mental functions were intact. Cranial nerves II to XII were unaffected. She presented deep tendon reflexes graded 2+/4+, preserved muscle strength, no Babinski sign, and a burning feeling on the right facial and brachial regions and right hemithorax. Involuntary rhythmic movements of the abdominal muscles were not exacerbated by touch. All other results from the physical examination were normal. According to the mental examination, the patient showed anxiety; modulated, coherent, and resonant emotions; and logical thoughts, including concerns about her state of health, with no other relevant findings. She was admitted to hospital for additional tests including electromyography and nerve conduction studies of abdominal, paraspinal, thoracic, and cervical muscles. Results showed a myoclonic pattern of involuntary contractions in thoracic dermatomes (T4 to T12). The patient was sedated before undergoing a gadolinium contrast MRI scan of the cervical and thoracic spine, which yielded normal results (Fig. 2). We also performed a complete blood count, HIV and syphilis serology (VDRL), a partial urine test, a lumbar puncture, and tests for creatinine, vitamin B12 and folic acid, erythrocyte sedimentation rate, C-reactive protein, serum electrolytes (potassium, sodium, magnesium, chloride), thyroid stimulating hormone, free T4, antinuclear antibodies, anti-dsDNA antibodies, extractable nuclear antigens, C3 and C4 complements, blood levels of lead and arsenic, and arterial gas. All tests yielded normal results. Since we suspected diaphragmatic flutter, we evaluated diaphragm movement with fluoroscopy. The study showed repetitive movements of the diaphragm (120movements per minute) and normal diaphragm mobility with inspiration and expiration; these findings are consistent with diaphragmatic flutter. The patient was treated with phenytoin and gabapentin, which provided partial pain relief but failed to improve dyskinetic movements. This slight drug-related improvement led us to perform an ultrasound- and fluoroscopy-guided right phrenic nerve block with bupivacaine. During the procedure, diaphragmatic flutter decreased until disappearing on the right side. Although symptoms improved significantly, they reappeared about 6hours later. Since clinical symptoms persisted, we decided to treat the patient by crushing and clipping the right phrenic nerve using video-assisted thoracoscopic surgery. This procedure achieved substantial and lasting improvement of symptoms, resulting in the patient being discharged.
Diaphragmatic flutter is an infrequent disorder characterised by high-frequency rhythmic involuntary contractions of the diaphragm and other respiratory muscles innervated by cervical nerve roots.1 Antonie van Leeuwenhoek is thought to have provided the first description in 1723 after experiencing the disorder himself. In one of his studies, De structura diaphragmatis: epistola domini Antonii van Leeuwenhoek, R. S. S. ad Societatem Regiam, the author explains that he had palpitations in the thorax. Although his doctor suggested that they were of cardiac origin, van Leeuwenhoek realised that his heart rate did not change when symptoms appeared, and thus concluded that it was the diaphragm and not the heart that caused the palpitations.2,3
The descriptions in the literature are based on case reports, and the largest series are those published by Rigatto and DeMedeiros, and Graber and Sinclair-Smith.3
Diaphragmatic flutter has also been called Leeuwenhoek disease, diaphragmatic myoclonus, respiratory myoclonus, belly dancer's syndrome, and belly dancer's dyskinesia.1,4
It has been described in both children and adults.5 Clinical symptoms are highly variable and the syndrome is very rare, which results in late diagnosis. According to the literature, it can take up to 18 years to diagnose this disorder. It may present with pain, but pain cannot be used to locate damage since it is perceived in the thorax, epigastrium, and lumbar region. In fact, this entity may even be confused with ischaemic heart disease due to the pain location, especially when pain affects the left hemidiaphragm: in these cases, pain radiates to the left arm and patients experience dyspnoea. Abdominal movements are also frequent, which has given rise to the term belly dancer's syndrome. These movements may appear at any location, especially in the upper quadrants, and they fluctuate throughout the day. No precipitating factors are known and contractions may persist during sleep according to some studies. Other reported symptoms are inspiratory stridor, epigastric pulsations, palpitations, dyspnoea, nausea, and vomiting. Pain has sometimes led patients to undergo surgery (appendectomy, cholecystectomy, among others) since they attributed the pain to surgical conditions.1–4,6
A number of causes may explain onset of diaphragmatic flutter. It has been described in conjunction with central and peripheral nervous system disorders, such as encephalitis and phrenic nerve irritation, pleural disorders (pleurisy), mediastinal disorders (adenopathies), intra-abdominal disorders (peritonitis), heart diseases (rheumatic fever), cardiac and thoracic surgeries (myocardial revascularisation), idiopathic cervical spine trauma, and lung diseases (including the case of a paediatric patient presenting diaphragmatic flutter after an upper respiratory tract infection). Other studies have described cases of diaphragmatic flutter following osmotic demyelination syndrome and secondary to galantamine and clebopride use.6–8
Diagnosis can be based on fluoroscopy since this technique shows real-time diaphragm movement and allows doctors to evaluate its amplitude and rate.3 Electrophysiological studies can also be used for this purpose. Needle electromyography is particularly useful: needle electrodes should be inserted into the diaphragm. Surface electrophysiological studies are less accurate since thoracic wall movements may interfere. Electrophysiological studies have shown that diaphragmatic flutter can maintain adequate ventilation despite suppressing normal breathing.9
Patients are usually diagnosed with some type of psychiatric disorder before a correct diagnosis is made and will therefore have been treated with multiple drugs, such as valproic acid, haloperidol, pimozide, and clonidine.6 Our patient had been treated with clonazepam and fluoxetine. Treatment is based on the descriptions given in different case series. Some articles recommend pharmacological treatment with phenytoin3 and carbamazepine,1 while others support such invasive procedures as phrenic nerve block at the C4 level with bupivacaine or methylprednisolone infiltrations. The latter procedure is performed when the disorder is believed to have an inflammatory origin, and it will temporarily resolve diaphragmatic contractions.6 In our patient, symptoms improved for 6hours after phrenic nerve infiltration with bupivacaine. Some authors suggest a surgical procedure to crush the phrenic nerve, after which symptom improvement has been reported as lasting up to 6 months, or the time it takes the nerve to regenerate. Several studies report positive outcomes of phrenic nerve crush at the C4 level.3,6
Please cite this article as: Ramírez JD, Gonzales M, Hoyos JA, Grisales L. Aleteo diafragmático. Descripción de caso y revisión de la literatura. Neurología. 2015;30:249–251.