In Spain, human immunodeficiency virus (HIV) testing is free; however, diagnosis of HIV infection was delayed in 45.9% of patients diagnosed in 2019.1 A high frequency of missed opportunities for earlier diagnosis of HIV infection has been reported.2 Late diagnosis is associated with such opportunistic infections as progressive multifocal leukoencephalopathy (PML) caused by John Cunningham (JC) virus. PML is characterised by demyelinating brain lesions in MRI studies, with no mass effect or gadolinium uptake, predominantly affecting the occipital and parietal lobes. The most frequent symptoms are loss of strength, ataxia, visual impairment, and cognitive alterations.3 The only effective treatment is antiretroviral therapy (ART), but 15% to 30% of treated patients present immune reconstitution inflammatory syndrome (IRIS), which consists of a paradoxical clinical exacerbation mediated by an exaggerated inflammatory response.4 PML-IRIS is associated with the rapid increase in CD4+ lymphocytes after onset of ART, with high mortality rates and the possibility of incapacitating sequelae.3
We present a case of late diagnosis of HIV infection and PML in a patient who presented severe complications in relation to IRIS.
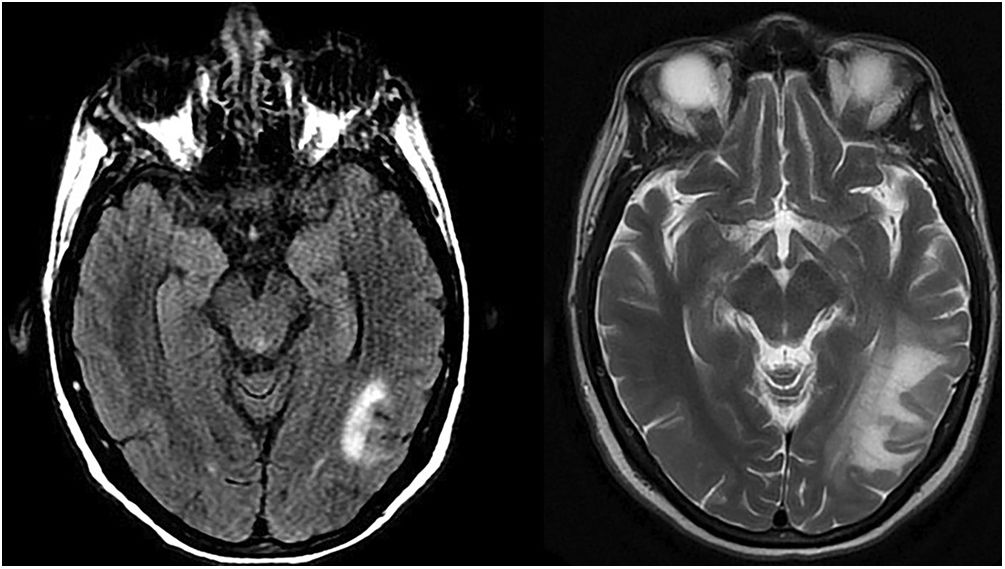
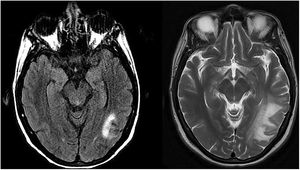
Our patient was a 45-year-old woman with history of depression and multiple visits to the emergency department, who was admitted due to a psychotic break. She presented oppositional behaviour, persecutory delusion, auditory hallucinations, and agitation, showing no improvement with antipsychotics. The neurological examination yielded normal results. Lymphocytopaenia (600 cells/mm3) was detected and an HIV test yielded positive results (viral load above 1 000 000 copies/mL and CD4+ lymphocyte count of 60 cells/mm3). A brain MRI study showed a T1-hypointese and T2-hyperintense lesion in the left temporo-occipital and right parietal white matter, showing no diffusion restriction or mass effect (Fig. 1, left). JC virus DNA was detected in the cerebrospinal fluid (CSF), and other infections were ruled out. We diagnosed PML and started ART (tenofovir-alafenamide, emtricitabine, and bictegravir), which improved the psychiatric symptoms. The patient was asymptomatic at discharge. One month later, CD4+ lymphocyte count was 274 cells/mm3 and the viral load was undetectable. Two months after starting ART, the patient reported progressive vision loss. An MRI study showed increased size of the lesions (Fig. 1, right); we ruled out eye disease and diagnosed probable IRIS, starting treatment with dexamethasone (4 mg/12 h) for 3 weeks. Treatment was subsequently tapered and withdrawn over 4 weeks. Four months after onset of ART, the patient was admitted due to seizures and disabling vision loss. After imaging studies and a CSF analysis, we ruled out other causes and suspected a diagnosis of IRIS; therefore, we restarted treatment with dexamethasone (4 mg/8 h). Seizures were controlled, but visual impairment persisted (right eye: –10.5; left eye: –9.5). The patient was admitted to a social healthcare centre.
Although cognitive alterations are frequent, psychosis is an infrequent manifestation of PML, with few reported cases.3,5
Glucocorticoids are the treatment of choice for PML-IRIS. They are indicated from onset as an adjuvant treatment in patients with HIV infection and tuberculous meningitis, with an estimated risk of IRIS of 18% and mortality of 2%.6 Given the central role of the host response in the pathogenesis of infectious diseases (damage-response framework described by Pirovski and Casadevall7), and the analogy with tuberculous meningitis and Pneumocystis jirovecii pneumonia, there is a need for new therapeutic strategies for PML-IRIS that may include the preventive use of glucocorticoids from the time of ART onset. In patients with haematologic malignancies, glucocorticoids may be an effective treatment for PML.8 One argument against the preventive use of glucocorticoids is that they attenuate the CD8 + T cell response to the JC virus9; however, early and prolonged administration may be associated with better prognosis.10
Our case illustrates the difficulty of diagnosing HIV infection in patients with psychiatric symptoms and the usefulness of systematically requesting HIV testing. Furthermore, after starting ART for HIV-PML, the patient should be carefully monitored, and early and prolonged administration of glucocorticoids should be considered in the event of IRIS, bearing in mind the potentially irreversible sequelae.
Please cite this article as: González-Granados A, Vera-Tomé A, Calvo-Cano A, Rodríguez-Vidigal FF, De la psicosis a la ceguera: ¿glucocorticoides precozmente en la leucoencefalopatía multifocal progresiva? Neurología. 2022;37:612–613.