Falls are a major health problem in elderly institutionalised patients, due to the associated high morbidity and mortality rates and the impact on future quality of life.
ObjectiveTo analyse the incidence and patient profile for falls, and to identify potential causes and effects. We also assess the efficacy of intervention in selected patients in preventing further falls.
MethodsWe performed a prospective study at a long-term care centre for 12 months. Data were collected via fall reports. The falls committee drafted a monthly data collection form.
ResultsA total of 155 falls were recorded in 80 patients, with 40% presenting more than one fall. Patients aged over 70 years accounted for 84.5% of falls; 42.7% of patients are able to walk independently; 55.5% of falls occurred in the bedroom; 74.8% of patients had been prescribed sedatives or psychoactive, or antihypertensive drugs; 27.7% of falls were due to loss of balance and 22.5% were due to patients performing an activity for which they did not have the capacity. Fractures occurred in 1.9% of patients.
ConclusionsPatients aged over 70 years, walking independently, receiving sedatives or psychoactive or antihypertensive drugs, and with history of falls were at greatest risk. The majority of falls occurred in the bedroom. Physiotherapy interventions were highly effective in cases selected by the falls committee.
Las caídas son un problema de salud importante en ancianos institucionalizados debido a su alta morbi-mortalidad y su relación con la calidad de vida futura.
ObjetivoAnalizar la incidencia de caídas, el perfil de los pacientes que las sufren e identificar las posibles causas y efectos. Valorar la eficacia de la intervención en pacientes seleccionados para evitar más caídas.
MetodologíaEstudio prospectivo en un centro de media y larga estancia durante 12 meses. La obtención de datos se hizo a través del parte de caídas. La comisión de caídas elaboró una hoja de recogida de datos mensuales.
ResultadosHubo 155 caídas de 80 pacientes, presentando el 40% más de una caída. El 84,5% en pacientes con más de 70 años. El 42,7% de los pacientes deambulan de manera independiente. Un 55,5% se producen en el dormitorio. El 74,8% de los casos tenían prescrito sedantes centrales, fármacos psicoactivos y antihipertensivos. El 27,7% de los casos sufrieron caídas por pérdida de equilibrio, y el 22,5% por realizar una actividad sin tener la capacidad necesaria. El porcentaje de fracturas está en 1.9%.
ConclusionesLos mayores de 70 años con pérdida de capacidad física y/o cognitiva, que presentan una marcha independiente, que tienen prescritos fármacos sedantes centrales, fármacos psicoactivos o antihipertensivos y que ya han tenido una primera caída, son aquellos que están en mayor riesgo de caídas. La habitación es el lugar donde más se caen. La intervención del fisioterapeuta en los casos seleccionados por la comisión de caídas fue altamente eficaz.
Falls, defined by the World Health Organization as an event that results in a person coming to rest inadvertently on the ground or floor or other lower level, constitute a major health problem in institutionalised elderly individuals due to the associated morbidity and mortality and their impact on the patient’s subsequent quality of life.1 Ageing leads to progressive loss of strength and function and an increase in the incidence of disorders that cause cognitive impairment. This results in loss of independence and increases the risk of falls.
Any strategy aimed at preventing falls is therefore extremely useful. All centres providing care to elderly individuals should implement fall prevention strategies, follow up all cases of falls, and evaluate the causes and trigger factors with a view to designing specific protocols to reduce the impact of falls and the associated sequelae in this population group.
In 2015, Hospital ICOT Ciudad de Telde, in the Canary Islands, created a falls committee to monitor these events and study the circumstances surrounding each case. In the first year (2016-2017), we implemented a plan to reduce the incidence of falls.
The programme had the following objectives:
- -
To analyse cases of recurrent falls.
- -
To improve communication between departments in recognising patients at risk (multidisciplinary assessment of fall risk).
- -
To offer a personalised intervention: technical support, follow-up of each individual case, and creation of personalised training programmes.
We also designed a more comprehensive falls report with additional sections, with a view to improving follow-up and preventing the most frequent risk factors for falls. The most important additional sections gathered data on age, level of independence, and medication.
Material and methodsStudy designThe falls committee conducted a prospective study of the incidence of falls at the hospital, a medium- and long-stay centre, between July 2016 and June 2017. The falls committee is formed by the technical coordinator, the neurologist, the physiatrist, the nursing coordinator (who coordinates the nursing staff of all units), and the physical therapy department. The committee holds monthly sessions to analyse the circumstances surrounding each fall and to describe the interventions of the physical therapy department in selected cases. The data gathered during the study period were compared against data from the previous year.
PopulationA total of 315 patients were admitted to the hospital during the study period.
Study variablesWe analysed the following variables:
- 1
Age
- 2
Sex
- 3
Factors potentially involved in the fall (setting, medication)
- 4
Use of physical restraints
- 5
Incidence of falls per unit, time and setting of the fall
- 6
Reason
- 7
Level of independence
- 8
Consequences
- 9
Referrals
Each time a fall occurs, the chief nurse of the unit completes a falls report and sends one copy to the nursing coordinator and another to the falls committee. At the end of the month, data are gathered from all falls reports completed during that period. We also analyse each case individually, evaluate whether an intervention by the falls committee is required, and follow up each case. Most cases require no intervention.
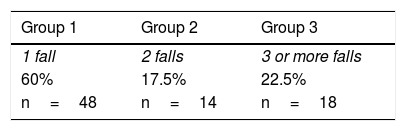
Data analysisWe analysed the data from the 12 monthly falls reports using tables and plots. We subsequently performed a descriptive analysis of the highest percentages for each variable. We calculated the total number of falls per patient and classified patients into 3 groups (patients presenting one fall, 2 falls, or 3 or more falls).
The incidence of falls was calculated using the total number of admissions.
We described the interventions implemented to prevent further falls, and drafted reports with data from each case, factors that may have had an influence on the event, the type of intervention implemented, and the outcomes.
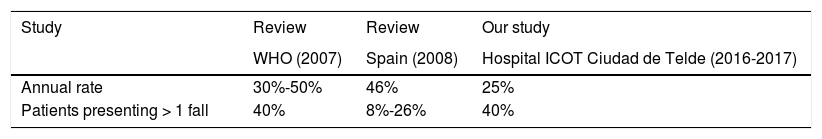
ResultsIncidence of fallsDuring the study period, we recorded a total of 155 falls in 80 patients. Most patients (60%) experienced only one fall, with 17.5% experiencing 2 falls and the remaining patients presenting at least 3 falls. The incidence of falls was estimated at 0.25, meaning that 25 patients out of every 100 new admissions are likely to present at least one fall (Table 1).
Patient profileFalls occurred in patients aged 70 years or older in 84.5% of cases, with 5.8% presenting in patients aged 60 to 69 years, 8.4% in patients aged 50 to 59 years, and 1.3% in patients younger than 50.
By sex, male patients accounted for 56% of falls.
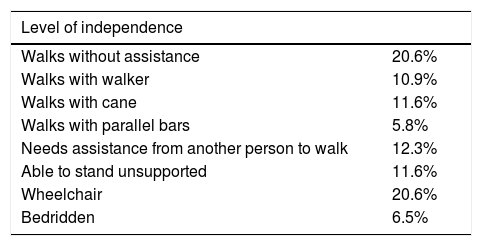
Regarding independence, 42.7% of patients walked independently, with or without walkers or canes.
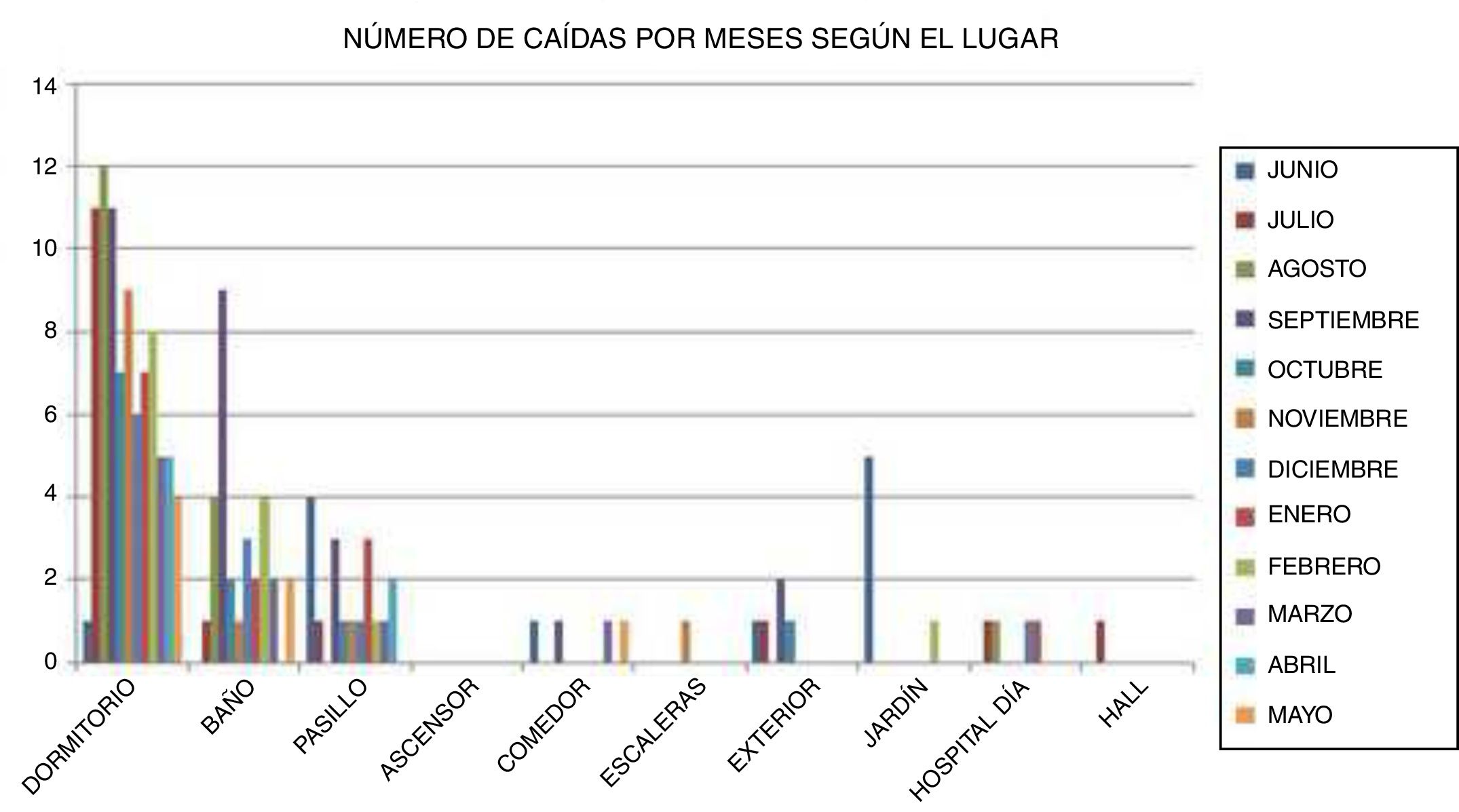
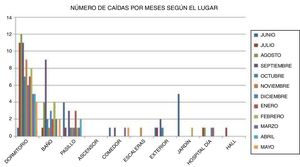
Circumstances surrounding the fallWe gathered data on the setting where the fall occurred, the time, and whether physical restraints were being used. Falls most frequently occurred in the bedroom (55.5%) and bathroom (19.4%) (Fig. 1).
By time of day, 40.6% of falls occurred in the morning, 41.3% in the evening, and the remaining 8.1% at night.
A total of 85.8% of the patients presenting falls were not restrained at the time the fall occurred; this was to be expected given the high proportion of patients who walked independently.
Possible causesThe possible causes of falls were analysed from 2 different perspectives.
Factors potentially influencing the risk of falls- -
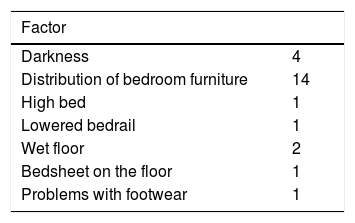
Setting. The setting may have played a role in the fall in 24 cases.
- -
Medication.
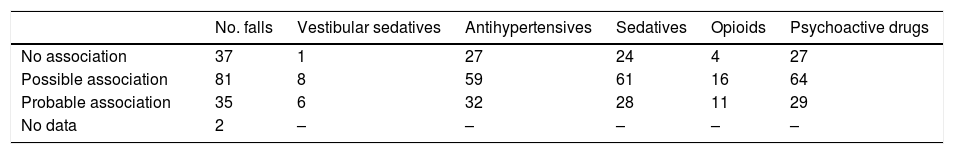
We analysed each fall individually to establish the likelihood (no association, possible association, or probable association) that the medication may have played a role in the fall.
In 74.83% of the cases where medication was judged to be a possible or probable cause of the fall, patients were receiving sedatives, psychoactive drugs, or antihypertensives. In 62.9% of cases, the patients were receiving more than 5 drugs.
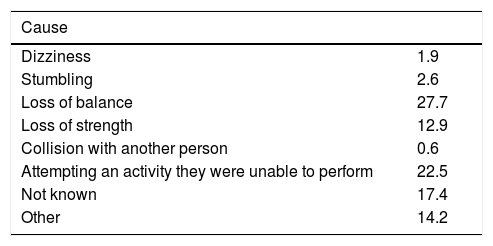
Reason for the fall recorded in the falls reportLoss of balance was the cause of the fall in 27.74% of cases; in 22.58%, falls occurred after the patient attempted an activity that they were unable to perform.
ConsequencesA total of 45.2% of falls had consequences, which mere mild in most cases; only 6 patients had to be referred for medical care, and 3 patients presented fractures.
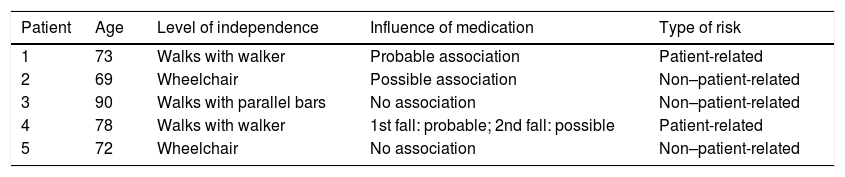
InterventionsThe physical therapy department had to attend 5 different patients, all of whom had presented more than one fall; none of them presented fractures. After their fall, these patients were assessed by the physiatrist, who prescribed physical therapy (daily sessions in one patient and 3 sessions per week in the rest). Physical therapy focused on improving balance, increasing muscle strength, and gait retraining, with technical support if required. None of the patients receiving physical therapy presented further falls after the intervention (Tables 2–6).
Level of independence in the patients presenting falls.
| Level of independence | |
|---|---|
| Walks without assistance | 20.6% |
| Walks with walker | 10.9% |
| Walks with cane | 11.6% |
| Walks with parallel bars | 5.8% |
| Needs assistance from another person to walk | 12.3% |
| Able to stand unsupported | 11.6% |
| Wheelchair | 20.6% |
| Bedridden | 6.5% |
Number of falls and causal relationship between falls and pharmacological treatments.
| No. falls | Vestibular sedatives | Antihypertensives | Sedatives | Opioids | Psychoactive drugs | |
|---|---|---|---|---|---|---|
| No association | 37 | 1 | 27 | 24 | 4 | 27 |
| Possible association | 81 | 8 | 59 | 61 | 16 | 64 |
| Probable association | 35 | 6 | 32 | 28 | 11 | 29 |
| No data | 2 | – | – | – | – | – |
The physical therapy department performed 2 types of interventions, depending on the cause of the fall:
- -
Risk intrinsic to the patient. The rehabilitation department designs an intervention (action protocol, number of sessions, treatment, discharge).
- -
Risk extrinsic to the patient. The intervention focuses on training nursing assistants and patients themselves in how to correctly perform patient transfers and mobilisations.
Table 7 presents the 5 patients undergoing interventions; data are provided on the level of independence, the impact of medication, and the type of risk.
Characteristics of the patients undergoing interventions.
| Patient | Age | Level of independence | Influence of medication | Type of risk |
|---|---|---|---|---|
| 1 | 73 | Walks with walker | Probable association | Patient-related |
| 2 | 69 | Wheelchair | Possible association | Non–patient-related |
| 3 | 90 | Walks with parallel bars | No association | Non–patient-related |
| 4 | 78 | Walks with walker | 1st fall: probable; 2nd fall: possible | Patient-related |
| 5 | 72 | Wheelchair | No association | Non–patient-related |
We present detailed information on the 5 interventions performed.
Patient 1. Patient who had presented 16 falls in a month, with no relevant consequences. The patient started a daily training programme to improve balance and gait. In this case, the intervention was performed before the monthly meeting due to the high frequency of falls.
Patient 2. This patient had poor trunk control, but was usually left unattended in the toilet before showering. We discussed the associated risks with the nursing assistants of the corresponding unit.
Patient 3. During a transfer from the shower wheelchair to the bed, a bedsheet was placed on the wet floor. Same intervention as in patient 2.
Patient 4. The patient presented physical deterioration and fell on 2 occasions. We started a training programme similar to that provided for patient 1, with sessions 3 times per week.
Patient 5. Transfer from wheelchair to bed was performed by a single nursing assistant in a patient for whom the manoeuvre required 2 nursing assistants. We spoke with the nursing assistants about the importance of waiting for a colleague before transferring the patient, to avoid unnecessary risks.
DiscussionAccording to a literature review on the topic published by the World Health Organization,2 28%-35% of adults over 64 years of age fall each year; this percentage increases with age (32%-42% of individuals over the age of 70) and frailty level (30%-50% of people living in long-term care institutions). Furthermore, 40% of elderly individuals present recurrent falls. The risk of falls must therefore be taken into account in hospitalised elderly patients.
According to a review by Da Silva et al.,3 the cumulative incidence of falls in Spain ranges from 14% in the community setting to 46% among institutionalised elderly individuals.
According to our data, the incidence of falls in our hospital is lower than the average rate in Spain. The high percentage of individuals presenting recurrent falls is noteworthy, and indicates that extra precautions should be taken in patients presenting a first fall.
According to Rubenstein,4 the incidence of falls in institutionalised elderly individuals is similar in men and women, or even slightly higher in men. In our study, 56% of falls were observed in men, which probably reflects greater impulsiveness in this subgroup.
According to Urruela et al.5 and Díaz et al.,6 most falls occur at night; in our hospital, however, 81.9% of falls occurred during the day, probably due to the fact that a high proportion of our patients walked independently and required no physical restraints.
Our data are consistent with the results of previous studies, in that physical deterioration7,8 and cognitive impairment7–10 show a direct correlation with the incidence of falls. In our study, 40.6% of falls resulted from loss of strength or balance, and 40% may have been due to cognitive impairment.
Da Silva et al.3 describe a linear relationship between medication and falls in elderly individuals. In our study, most patients who fell were taking sedatives, such as benzodiazepines, followed by psychoactive drugs and antihypertensives.
The consequences of falls are mild in most cases, with the incidence of fractures ranging from 1.2%11 to 16.5%.8 The incidence of fractures in our sample was low, at 1.9%.
According to the review by Torres Egea and Sánchez Castillo,12 nearly all the scientific evidence on fall prevention in institutionalised elderly individuals underscores the multifactorial nature of the problem and the need for an individualised, multidisciplinary approach. Fall prevention interventions in nursing homes and long-stay centres were found to be effective, reducing the overall risk of falls by 59%. In our hospital, prevention strategies were effective in preventing recurrent falls, which shows that detecting patients at risk of fall recurrence (6.25% in our sample) constitutes a useful prevention strategy. However, we lack a scale for predicting the risk of falls.
ConclusionsEstablishing falls committees in nursing homes and long-stay centres is essential. The body must include professionals from different specialties, and should both gather data on falls and design interventions aimed at reducing their number and severity.
According to the data gathered by our committee, the risk of falls is higher in patients older than 70 years and presenting physical deterioration or cognitive impairment; walking independently (with or without assistance); taking sedatives, psychoactive drugs, or antihypertensives; or who have already presented a fall.
Most falls occurred in the bedroom, which underscores the need to adapt these spaces.
Physical therapy interventions were found to be highly effective, despite the small number of cases requiring intervention.
Future studies should aim to develop a tool for predicting the risk of falls in this population subgroup with a view to the early implementation of physical therapy interventions in the individuals presenting the greatest risk.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Cáceres Santana E, Bermúdez Moreno C, Ramírez Suarez J, Bahamonde Román C, Murie-Fernández M. Incidencia de caídas en el hospital de larga-media estancia. Factores de riesgo y estrategias para la prevención. Neurología. 2022;37:165–170.