Photophobia is a symptom of abnormal light intolerance without pain sensation that requires an anamnesis and an examination to diagnose an underlying etiology.
Basic procedureThis article focuses on 30 clinical cases with isolated intense photophobia and on the review of the literature.
ObjectiveThe purpose of this article is to establish diagnostic criteria for photophobia.
ResultsThe etiology of photophobia appears to be at the level of the intrinsically photosensitive retinal ganglion cells known as melanopsin cells and at a neurochemical level mediated by calcitonin-related peptide and the pituitary activating peptide cyclase.
ConclusionThe treatment of photophobia could consist of monoclonal antibodies against calcitonin-related peptide and/or pituitary activating peptide cyclase.
La fotofobia es un síntoma de intolerancia anómala a la luz sin sensación de dolor que requiere de una anamnesis y una exploración para el diagnóstico de una etiología subyacente.
Procedimiento básicoEl presente artículo se centra en 30 casos clínicos con fotofobia intensa aislada y su revisión de la bibliografía.
ObjetivoEl objetivo consiste en establecer unos criterios diagnósticos de la fotofobia.
ResultadosLa etiología de la fotofobia parece encontrarse a nivel de las células ganglionares de la retina intrínsecamente fotosensibles, conocidas como las células de la melanopsina, y a un nivel neuroquímico mediado por el péptido relacionado con la calcitonina y el péptido pituitario activador de la ciclasa.
ConclusiónEl tratamiento de la fotofobia podría consistir en anticuerpos monoclonales contra los péptidos relacionados con la calcitonina y/o el péptido pituitario activador de la ciclasa.
Photophobia is a painless, anomalous intolerance to light that requires history taking and clinical examination to diagnose the underlying aetiology. Photophobia is usually associated with ophthalmological disease (from anterior segment involvement, such as dry eye syndrome, iritis, and blepharitis, to posterior segment involvement, such as retinal dystrophy and retinitis pigmentosa), neurological disease (from primary headache, with migraine being the most frequent, to traumatic brain injury), psychiatric disorders (depressive disorders and anxiety disorders), or pharmacological treatments (barbiturates, benzodiazepines, or haloperidol).1
This article focuses on photophobia associated with primary headache in the context of migraine. Photophobia presents in up to 80% of patients with migraine, manifesting before or during migraine episodes.1
In this context, photophobia is usually associated with other characteristic symptoms, such as headache, phonophobia, nausea, and vomiting.2
Based on 30 clinical cases and the published literature, we propose a series of diagnostic criteria for intense and isolated photophobia.
Material and methodsWe present 30 cases of patients diagnosed with intense, continuous photophobia at the neuro-ophthalmology unit at Hospital Clínico San Carlos and presenting normal neurological and ophthalmological examination results. Only 3 were men. Mean age was 38 years (range, 27-54) (Table 1).
Characteristics of the 30 cases with intense, disabling photophobia.
| Sex | Age | Migraine | Aura | Treatment |
|---|---|---|---|---|
| Man | 38 | HFEM | No | Triptans |
| Woman | 54 | LFEM | No | Magnesium |
| Woman | 36 | LFEM | No | Triptans |
| Woman | 42 | LFEM | No | Triptans |
| Woman | 27 | LFEM | No | Melatonin |
| Woman | 52 | LFEM | Yes | Melatonin |
| Woman | 45 | LFEM | No | Topiramate |
| Woman | 32 | HFEM | No | Nebivolol |
| Woman | 29 | HFEM | No | Nebivolol |
| Woman | 54 | HFEM | No | Zonisamide |
| Woman | 36 | HFEM | No | Duloxetine, zonisamide, botulinum toxin |
| Woman | 38 | CM | No | Botulinum toxin, venlafaxine, pregabalin |
| Woman | 37 | CM | No | Pregabalin, lisinopril |
| Woman | 28 | HFEM | No | Triptans |
| Woman | 35 | LFEM | No | Zonisamide |
| Woman | 45 | HFEM | Yes | Zonisamide |
| Woman | 42 | HFEM | Yes | Topiramate |
| Woman | 34 | HFEM | Yes | Duloxetine |
| Woman | 43 | HFEM | No | Melatonin, nebivolol |
| Woman | 35 | HFEM | No | Botulinum toxin, duloxetine |
| Woman | 34 | CM | No | Botulinum toxin |
| Woman | 42 | CM | No | Magnesium, nebivolol |
| Woman | 36 | CM | No | Duloxetine, topiramate |
| Man | 35 | CM | No | Botulinum toxin, melatonin, venlafaxine |
| Woman | 48 | CM | No | Zonisamide, botulinum toxin |
| Woman | 42 | HFEM | No | Candesartan |
| Woman | 29 | HFEM | No | Candesartan |
| Woman | 38 | CM | Yes | Botulinum toxin |
| Woman | 37 | CM | No | Duloxetine, melatonin |
| Man | 31 | HFEM | No | Nebivolol |
CM: chronic migraine; HFEM: high-frequency episodic migraine; LFEM: low-frequency episodic migraine.
The ophthalmological examination included a visual acuity test, biomicroscopy of the anterior pole, intraocular pressure determination, assessment of extrinsic and intrinsic ocular motility, and fundoscopy. Visual field campimetry and optical coherence tomography (OCT) yielded normal results in all cases.
Acute episodes of continuous photophobia that manifested in all patients previously diagnosed with migraine headache (chronic migraine, high- and low-frequency episodic migraine) presented without any prodromal symptom of migraine or any other accompanying symptom. Only 5 patients presented migraine aura in addition to photophobia. No patient manifested any trigger factor or subsequent headache (Table 1).
All patients underwent complementary imaging studies, such as CT and brain MRI; structural disease was not detected in any patient.
Patients with migraine received such treatments as antiepileptic drugs (topiramate, zonisamide, and pregabalin), antidepressants (venlafaxine or duloxetine), beta-blockers (nebivolol), and other drugs (candesartan, magnesium, melatonin, and botulinum toxin) (Table 1).
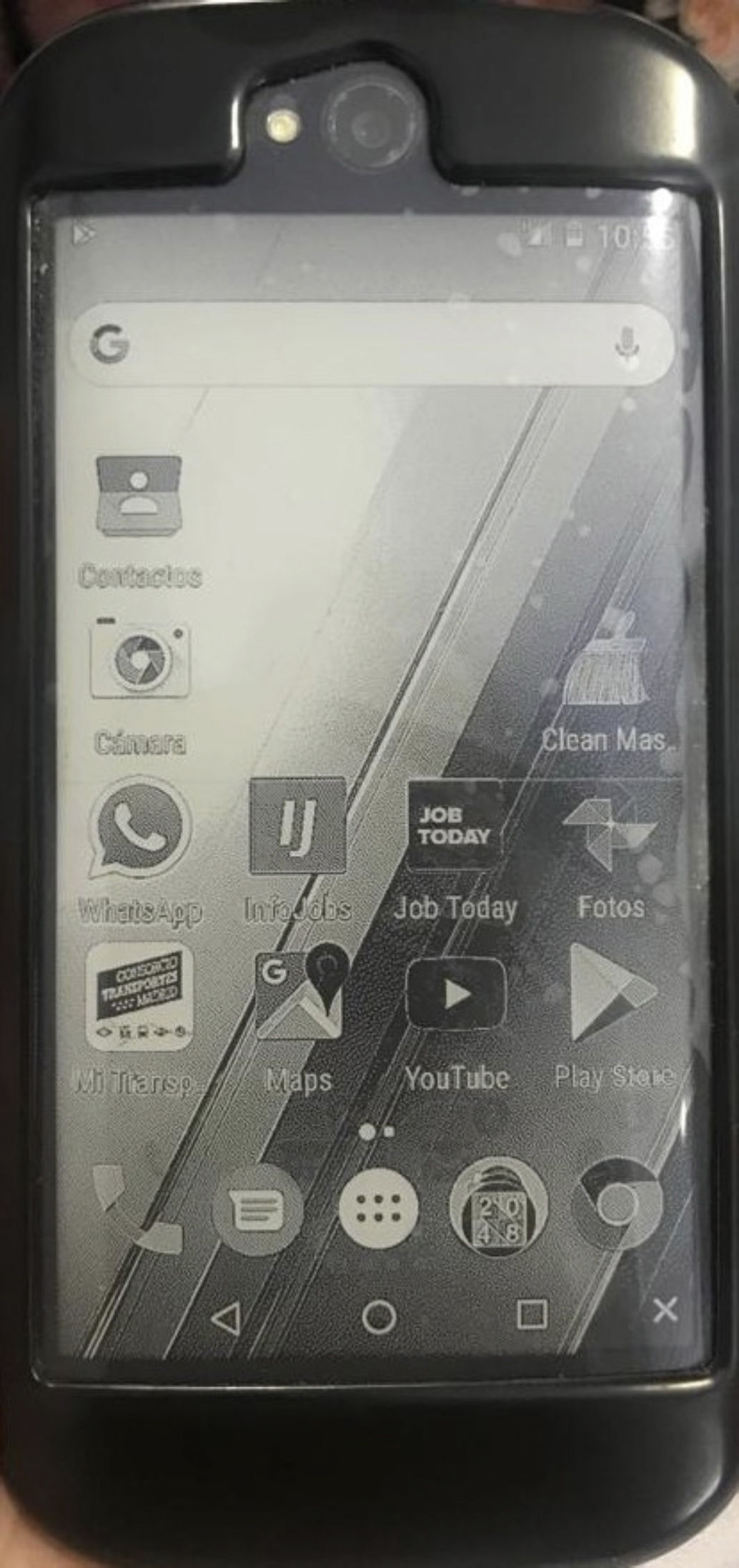
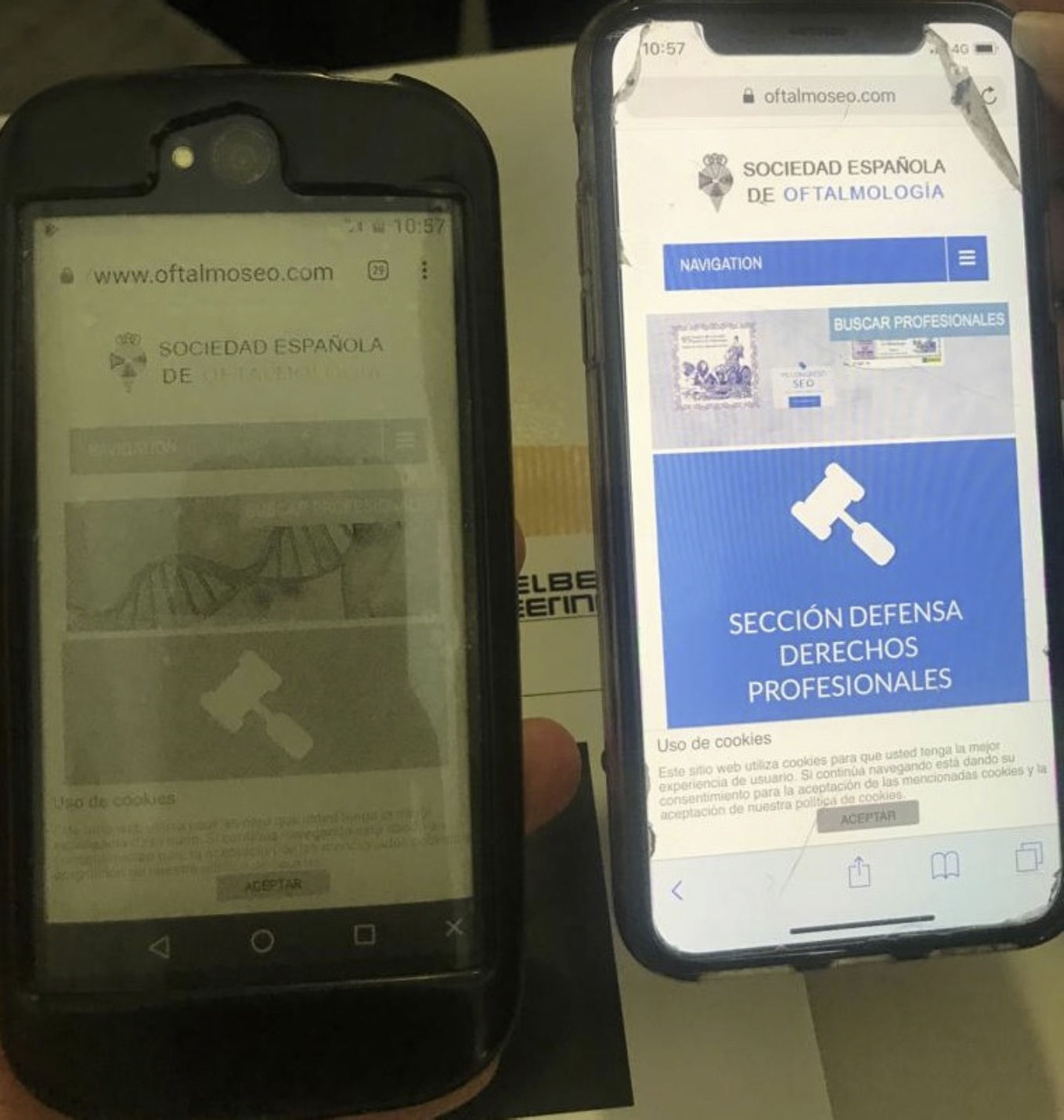
None of these treatments improved the isolated, disabling photophobia present in all the patients in our series. One of patient had modified all of his everyday habits, covering light sources (windows and balconies), limiting trips outside during daytime, and even adapting light-emitting devices, such as his mobile phone (Figs. 1 and 2).
Having ruled out ophthalmological, neurological, and psychiatric diseases, and diseases caused by pharmacological iatrogenesis, patients were diagnosed with intense, persistent photophobia. The aetiology of photophobia in our patients is functional, in the context of migraine with no subsequent headache.
DiscussionLight sensitivity thresholds are highly variable between patients. Patients with migraine or headache have a reduced threshold and therefore present greater sensitivity. Different wavelengths cause some degree of discomfort. Several studies3 report that such short wavelengths as the colour blue and such long wavelengths as that of red light are particularly unpleasant for patients with migraine.
The decreased sensory threshold in the occipital cortex and the resulting increase in susceptibility to photophobia have been studied using such neuroimaging techniques as functional MRI.4
Retinal phototransduction is performed by intrinsically photosensitive retinal ganglion cells (ipRGC), also known as melanopsin-containing retinal ganglion cells.5 Unlike other ganglion cells, which project axons to the lateral geniculate nucleus, these cells project axons to the suprachiasmatic nucleus6 and to the Edinger-Westphal nucleus to control the pupillary light reflex.1 Furthermore, studies with animal models3,7 have reported that ipRGCs project connections to the pain centres in the thalamus. We may hypothesise that this connection exists in patients with photophobia in the context of migraine.
Because they contain the photosensitive pigment melanopsin, ipRGCs are intrinsically photosensitive, meaning that they may be stimulated by light in the absence of traditional photoreceptors such as cones and rods.6
Studies with animal models describe 3 possible pathways by which ipRGCs transform light stimuli into painful sensations. The first pathway involves activation of the trigeminal nerve, which causes ocular vasodilation and pain activation at the trigeminal level.8 The second pathway consists of a direct connection between ipRGCs and pain centres in the thalamus,3,7 where sensory integration and connections towards the somatosensory cortex take place. The third proposed pathway does not include the optic nerve,9 as studies with animal models have shown direct phototransduction to the trigeminal system after section of the optic nerve.
At the trigeminovascular level, 2 neuropeptides modulate pain transmission in patients with migraine: the calcitonin gene–related peptide (CGRP) and the pituitary adenylate cyclase–activating polypeptide (PACAP). Both are vasodilators and pain triggers.10,11 Animals with mutations in the CGRP receptor showed light-aversive behaviour after administration of CGRP, whereas those lacking PACAP developed no light aversion.12 Both neuropeptides may be the cause of the unique characteristics present in migraineurs and absent in controls, which may lead to photophobia.13
Taking into account the pathophysiology of photophobia at the anatomical level, according to functional neuroimaging studies of the occipital cortex, at the neurophysiological level, analysing the melanopsin-containing retinal ganglion cells, and at the neurochemical level, studying the peptides of the trigeminovascular system, we may establish a series of diagnostic criteria for isolated photophobia. Santos-Ly-Porta diagnostic criteria:
- •
Duration of more than 3 months
- •
Continuous photophobia lasting longer than 24 hours
- •
Meets criteria for episodic migraine
- •
Isolated photophobia without aura
- •
Not explained by another medical aetiology (medication, psychiatric disorder, etc).
Finally, it is important to differentiate eye involvement from photophobia as a symptom of the visual aura preceding migraine. Photophobia symptoms involve light-related discomfort with unaltered vision; at the neurochemical level, CGRP and PACAP alterations are observed. On the other hand, visual aura manifests as vision loss that depends on the type of aura, and is associated with glutamate alterations.
In conclusion, photophobia is considered an isolated symptom of migraine of unknown prevalence whose recognition by neurologists and ophthalmologists is essential to the correct diagnosis and management of these patients. In our series, the majority of patients were young women. The possible treatment of intense, isolated photophobia may be based on monoclonal antibodies against the CGRP and PACAP peptides.
Conflicts of interestThe authors have no conflicts of interest to declare.