Intracranial lipomas are uncommon and benign congenital malformations that account for only 0.03% to 0.08% of all types of intracranial masses.1 They are usually located in the interhemispheric fissure, especially in the corpus callosum. Lipomas of the corpus callosum are frequently associated with other congenital malformations of that structure, such as agenesis, hypoplasia, or hypertrophy. Since half of all cases are asymptomatic, they are only diagnosed based on incidental findings in neuroimaging studies. In the remainder of the cases, they are associated with neurological symptoms such as psychomotor retardation, headache, epilepsy, and cerebral palsy.
Our patient was a 23-year-old woman with a history of migraine without aura. Her gestation and birth were uneventful and psychomotor development was normal. She did not suffer from any febrile seizures, cranial trauma, or central nervous system infections during childhood. She had no family history of epilepsy or any other neurological disorders.
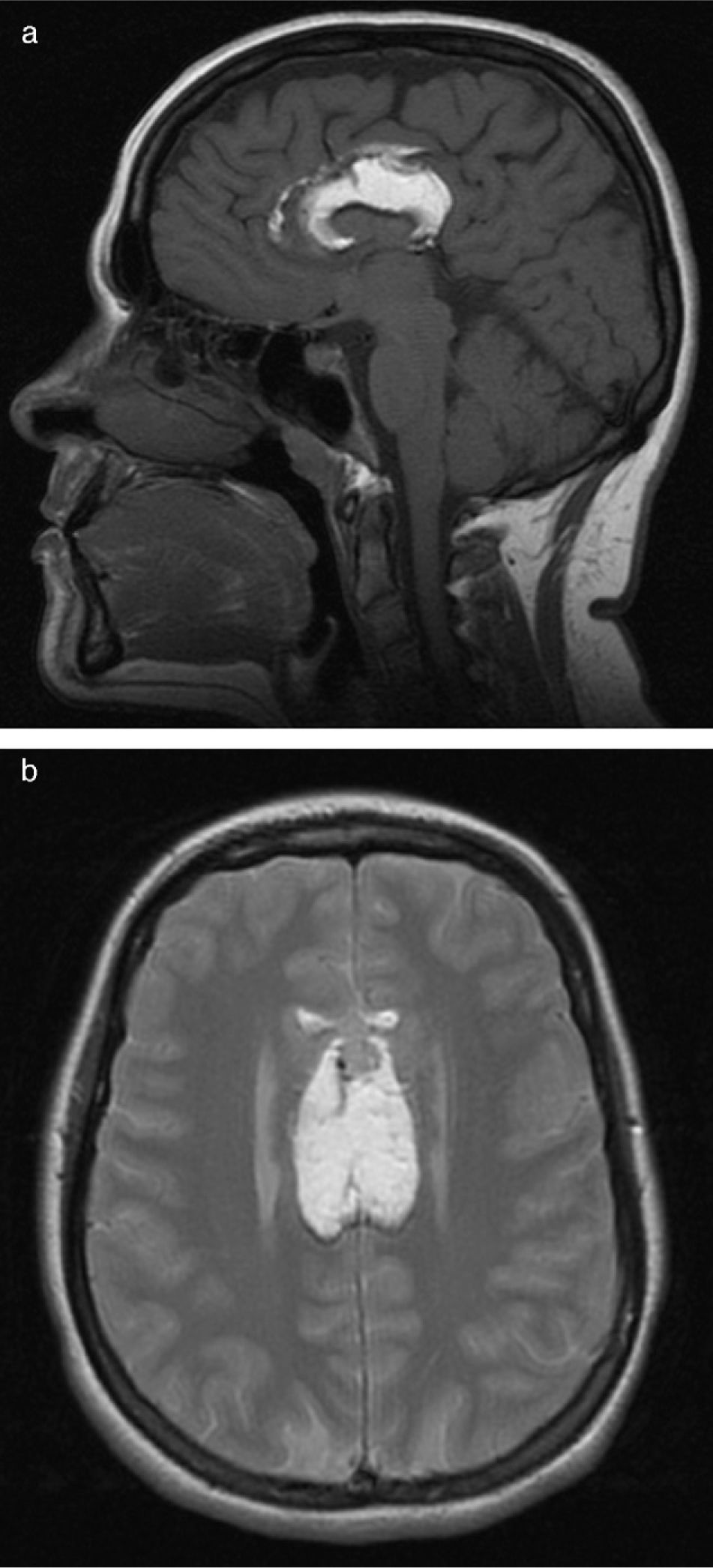
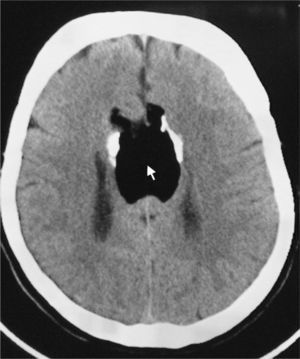
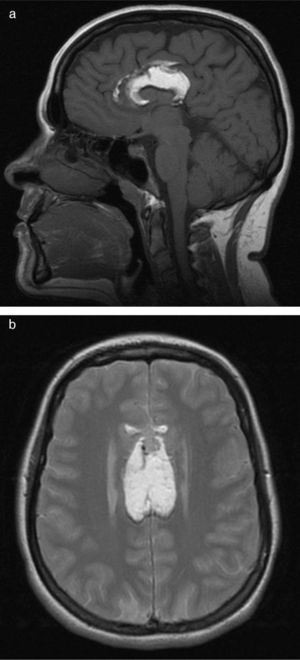
The patient visited the emergency department with symptoms of disorientation and buccofacial movements suggesting complex partial epileptic seizure. Neurological examination was normal. The cranial CT scan carried out in the emergency department (Fig. 1) showed absence of the corpus callosum and a hypodense homogeneous lesion in its location. We observed curvilinear calcifications on both sides of the lesion. Findings suggested agenesis of the corpus callosum with interhemispheric lipoma. Treatment with valproic acid was prescribed. The electroencephalogram showed epileptiform activity in the left temporo-parietal region. Brain MRI (Fig. 2) showed that the entire corpus callosum from the genu to the splenium was occupied by tissue that was hyperintense on all sequences, with the exception of the fat suppression sequence. The sagittal sequence showed bands of tissue that may correspond to remnants of the normal corpus callosum located between the lipomatous areas. We also observed slight dilation of the posterior horns of both lateral ventricles.
The patient received several antiepileptic drugs in different combinations, but seizure control was never achieved. Since that time we have performed several routine brain MRI scans and the lesion has remained unchanged.
Lipoma of the corpus callosum is a congenital disorder which probably arises due to poor differentiation of the meningeal tissue. Agenesis of the corpus callosum is a type of cerebral dysraphism in which the neural tube does not close properly.
This disorder is usually accompanied by epilepsy, which may manifest as either partial simple seizures or complex seizures.2 The origin of seizures is unknown, but they could stem from an epileptogenic focus caused when the cerebral cortex is invaded by the collagenous capsule of the lipoma, or from interhemispheric disconnection.
The appearance of the corpus callosum lipoma on the cranial CT scan is quite typical, with the low attenuation seen only in adipose tissue. In addition, it is surrounded by bilateral, rounded mural calcifications. After administration of contrast, the lesion showed no changes. In the brain MRI the lesion presents characteristics of fatty tissue, with a hyperintense signal in both T1- and T2-weighted studies.3 During complete agenesis of the corpus callosum, the lateral ventricles are far apart and never converge. They often have small frontal horns and disproportionally thick occipital horns (colpocephaly).
Differential diagnosis must be performed with epidermoid cyst, teratoma, craniopharyngioma, and epidermoid tumours.4 The cystic content of the craniopharyngioma may have a fat-like density, but the appearance is complex with atypical calcifications. Teratomas and dermoid cysts are usually heterogeneous because they contain other tissues in addition to fat. Dermoid cysts are generally located in the cerebellopontine angle, parahypophyseal region, or the fourth ventricle. The density of the lesion in the cranial CT scan is similar to that of cerebrospinal fluid.
Some cases of interhemispheric lipomas are associated with agenesis of the corpus callosum resulting from connatal infection with cytomegalovirus or X chromosome deletion, although most are idiopathic.
Surgical treatment is not recommended except in cases of secondary hydrocephalus that require ventriculoperitoneal shunting. Surgery is not advisable in other cases due to their abundant vascularisation, capsule infiltration, and adherence to adjacent tissue, plus the fact that these tumours do not grow and often have few clinical consequences. Even when surgery is performed, epileptic seizures rarely cease. Nevertheless, other authors have had favourable results using microsurgery and a CO2 laser.5
Please cite this article as: Jiménez Caballero PE. Lipoma interhemisférico asociado a agenesia del cuerpo calloso. Neurología. 2012;27:515–7.