Dystonia is a hyperkinetic disorder characterized by sustained or intermittent muscle contractions, resulting in abnormal repetitive movements and/or postures.1 Oromandibular dystonia (OMD) is a focal type of dystonia that involves masticatory and/or lingual muscles. Lingual dystonia is one of its subtypes. According to some case series, it might take up to the 4% of all the dystonias assessed in a Movement Disorder Department.2 Speech-induced lingual dystonia is rare. Mainly, it can be idiopathic and according to literature can be considered as an occupational dystonia in some patients.3 Despite its low prevalence, it can be very disabling and requires proper identification and management. We report here a case of a young man who presented with an isolated speech-induced lingual dystonia with an excellent response to Botulinum neurotoxin (BoNT).
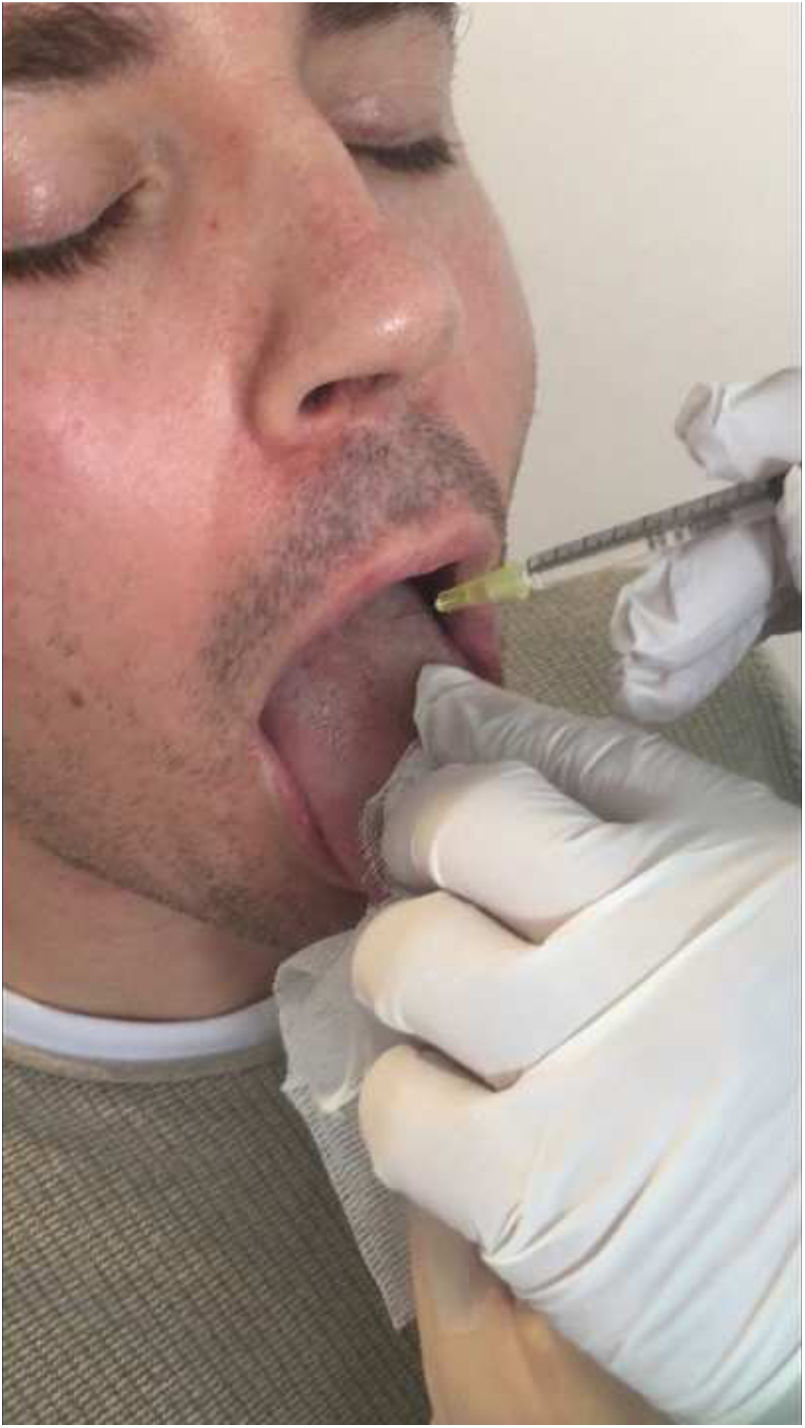
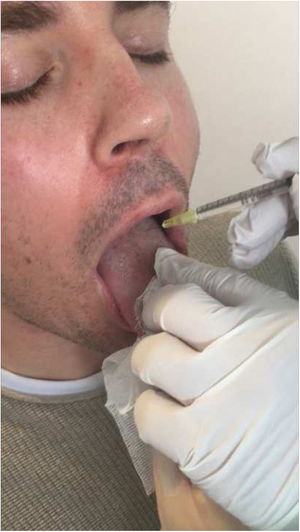
A 34 year-old man was referred to our department of Neurology with a five month history of slurred speech and progressive difficulty to move the tongue. A second-grade relative suffered from epilepsy, but there was no other family history of interest. He worked as telemarketer and spent up to eight hour-a-day speaking. Due to his symptoms, which continued worsening, he had to stop working and felt embarrassed when holding a conversation. No concomitant treatment or any other precipitating factor were found. His neurological exam revealed speech-induced tongue protrusion associated with mild to moderate dysarthria (Video 1). His symptoms improved when chewing gum (Video 2) or bread, as well as when speaking out. Brain MRI (including T2-sequence), electromyography (EMG), and extensive blood tests (including thyroid function, copper metabolism, folate and vitamin B12 levels) were normal. A diagnosis of idiopathic speech-induced focal dystonia (occupational) was performed and trihexyphenidyl (up to 4.5mg) was started, obtaining slight improvement without remarkable secondary effects. Six months later BoNT was started. Specifically, 2.5 units of BoNT (Botox®, Allergan Pharmaceuticals) were injected intraoral bilaterally in only 1 point of each genioglossus muscle (Fig. 1). No secondary effects were observed. One week later he noticed slight clinical improvement, but only maintained for one month. BoNT injection was repeated within 3 and 6 months, increasing dosage up to 5 units at each genioglossus. The second infiltration led to a clinical benefit that remained for only two months. Five days after the third injection a remarkable and sustained response was referred. The neurological exam was normal four months later (Video 3). Trihexyphenidyl was left progressively without impairment. One year later, the patient was looking for a job and reported a great improvement into his social life.
Speech-induced dystonia is a rare, but potentially really disabling condition. Its pathophysiology is not clear yet. Classical models were based into the idea of an abnormal plasticity regulation.4 However, some recent publications question this hypothesis, considering the plasticity response variability inter and intra-subject as well as plasticity is not required to develop secondary dystonia.5,6 Current hypothesis defend that both genetic and environmental factors play an important role in the aetiology of dystonia. Different brain structures (thalamus, cerebellum and sensorimotor cortex) are thought to be involved in its pathophysiology, leading to a network disfunction.6,7 Due to the low prevalence of lingual dystonia, it has previously been reported on in single case reports8,9 or case series.10,11 Recently, Yoshida et al. reported the largest series with 172 patients with lingual dystonia.2 Lingual protrusion, as in our case, was the most frequent but retraction, curling and lateropulsion dystonia have been observed as well. Moreover, it can be considered as an occupational dystonia. Indeed, task-specificity was observed in 90.1% of patients reported by Yoshida et al during speaking, chewing, or swallowing. Our patient had no history of exposure to neuroleptic medications, facial or oromandibular injuries, or recent infection. For this reason, the condition was diagnosed as a lingual dystonia specifically induced by speaking after all laboratory examinations had ruled out secondary causes. Isolated lingual dystonia is extremely rare as most reports have described patients with lingual dystonia who also displayed dystonic movements elsewhere.2 According to this, a case of speech-induced task-specific OMD (involving perioral muscles, the tongue and the jaw) has been reported in a bingo caller8 as well as in a telemarketer.9
A number of treatments are used in oromandibular dystonia such as trihexyphenidyl, baclofen, clonazepam, tiapride, or zolpidem.11 However, BoNT injection has been demonstrated to be the most effective.2,8,11–13 The genioglossus makes up the bulk of the tongue's muscle mass and is responsible for tongue protrusion, making it an ideal candidate for injection. We did not use EMG guide for injections. However, its use is recommended as it may help to identify muscles correctly and to reduce the risk of potential complications such as dysphagia or aspiration. In any event, administration should be always done by an experienced professional. BoNT tongue injections can cause some potential life-threatening secondary effects, as dysphagia or aspiration. Therefore, its administration should be done by an experienced professional. In our case, it is worth noting the absence of side effects and the good response with low doses.
As conclusion, speech-induced lingual dystonia is an uncommon movement disorder that can face as an occupational phenomenon. Neurologists and other physicians need to be aware of this condition, even in the absence of other dystonic phenomena. Although a few cases have been reported to date, BoNT seem to be an effective treatment for this condition. Further studies are needed to clarify underlying mechanism and to evaluate the long-term efficacy of BoNT.
FundingNone declared.
Author's contributionCarlos Cores Bartolomé: conception, organization, and execution of the project writing of the first draft of the manuscript.
José Manuel Paz González: review and critique. Treatment of the patient.
María José García Antelo: review and critique. Diagnosis of the patient.
Diego Santos García: review and critique. Diagnosis and treatment of the patient.
Conflicts of interestNone.
Carlos Cores Bartolomé has received honoraria for educational presentations by Lundbeck, UCB Pharma and Bial.
José Manuel Paz González has received honoraria for educational presentations by UCB Pharma, KRKA, Zambon, Abbvie and Bial.
María José García Antelo: none.
Diego Santos García has received honoraria for educational presentations and advice service by Abbvie, UCB Pharma, Lundbeck, KRKA, Zambon, Bial, Italfarmaco, and Teva.
The following are the supplementary data to this article: