Limb-shaking transient ischaemic attack (LS-TIA) is defined as the shaking of one or more limbs due to a contralateral hemispheric transient ischaemic attack caused by haemodynamic mechanisms, usually carotidal stenosis.1–3 Some authors have postulated an epileptogenic mechanism induced by ischaemia,4,5 although this has not yet been proven. In fact, to date, there have been attempts to find epileptiform discharges on EEG, but so far they have been unsuccessful. We describe a case of LS-TIA with epileptiform discharges on EEG.
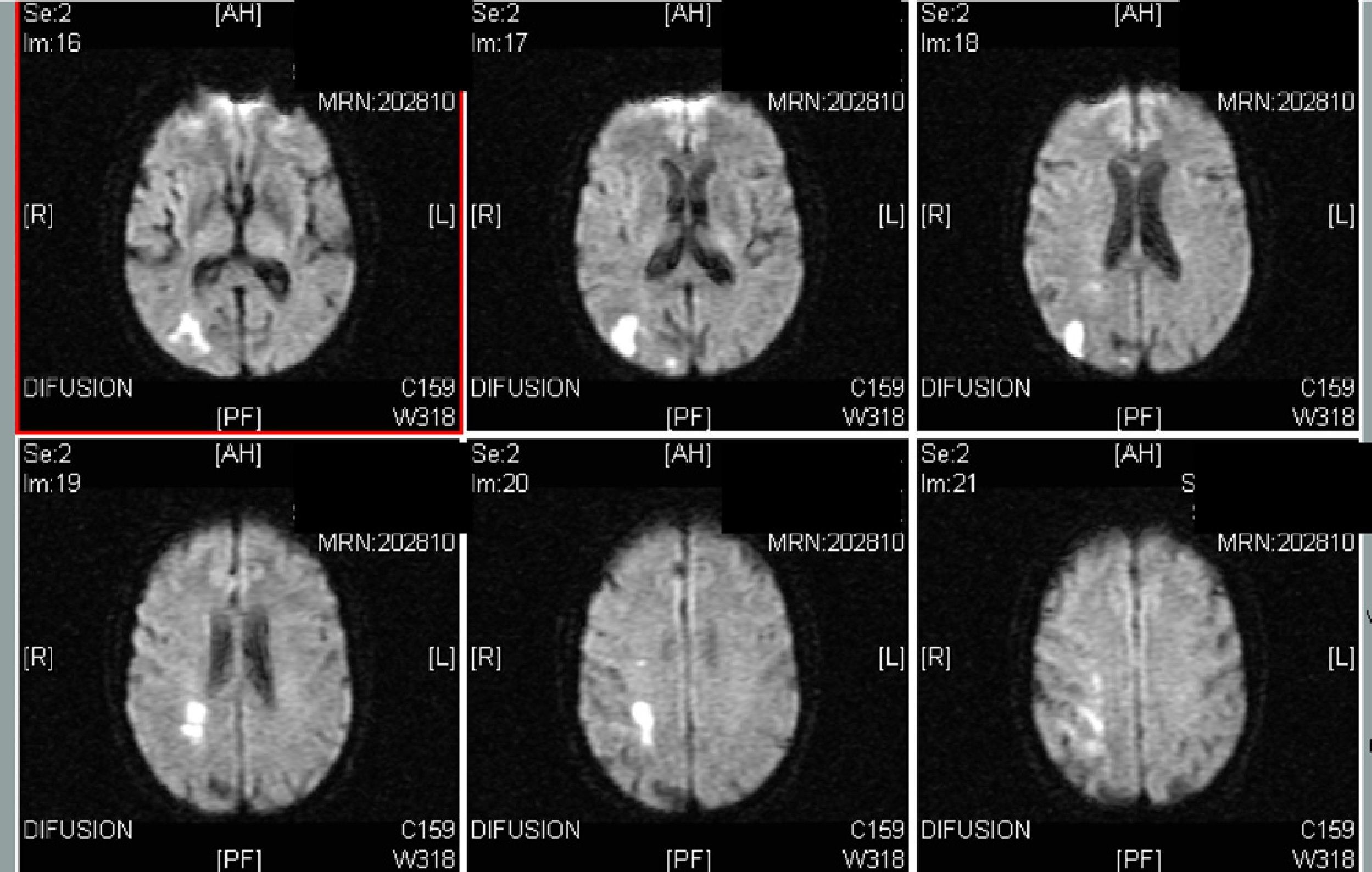
The patient was a 75-year-old male, current smoker, who was admitted after suffering 5 episodes in 1 month of shaking of the left arm whilst standing, along with speech difficulty, lasting for 3–4min. Physical examination detected left, central, facial palsy and live osteotendinous reflexes in the left arm. Duplex examination of the supra-aortic trunks also found 60%–70% stenosis in the right internal carotid (Fig. 1), whilst the EEG presented sharp wave, paroxysmal discharges at 6Hz in the right hemisphere, coinciding with left arm clonisms (Fig. 2). The cranial MRI detected a subacute ischaemic lesion in the terminal territory of the posterior, right, middle, cerebral division (Fig. 3).
These episodes disappeared with rest in supine position, strict control of blood pressure, antiplatelet therapy and statins. Subsequently, the patient underwent carotid endarterectomy, whilst antiplatelet therapy and control of vascular risk factors were maintained. The patient remained asymptomatic.
The first description of LS-TIA symptoms was given by Fisher in 1962.6 According to Yanagihara et al.,1 it would correspond to a case of “stereotyped and self-limiting involuntary movements of one or both limbs on the same side of the body, usually consisting of continuous and asynchronous shocks associated with preocclusive stenosis or occlusion of the contralateral internal carotid”.1,7 Other clinical features would include a latency of seconds after a hemispheric, flow restrictor, triggering event (standing, neck movements, Valsalva manoeuvres), duration of seconds or minutes and possible speech or language alterations, but never loss of consciousness, with a frequent association with contralateral carotid bruit.1–4,7,8 From an epidemiological standpoint, it is a rare occurrence: there were only 45 cases published in 20049 and 12 cases in records dating back 13 years at a cerebrovascular referral centre in the U.S.A.1 Its main differential diagnosis would be with motor simple partial seizures, from which it can be distinguished by the absence of Jacksonian gait and its association with states of reduced hemispheric flow: standing, cervical extension, Valsalva manoeuvres and even postprandial period.1,10 The findings described in laboratory tests include: EEG does not detect epileptiform activity, only contralateral hemispheric slowing in some cases1,11; CT or MRI scans do not detect current lesions, only sequelae of previous lesions in some cases; vascular imaging often reveals severe stenosis or occlusion of the common carotid or the contralateral extracranial internal carotid. Regarding its therapeutic management, antiepileptic drugs appear to be ineffective. The most effective strategy seems to be restoration of the hemispheric flow through postural measures, antiplatelet therapy or anticoagulation therapy and surgical management by endarterectomy.1–3,7,8,12 Regarding its aetiopathogenesis, it seems clear that the cause would be hemispheric flow decrease due to stenosis or carotid occlusion.2,11 This in turn would cause the phenomenon, either by an extrapyramidal mechanism or by a cortical epileptogenic mechanism. The extrapyramidal theory would be supported by the absence of epileptiform activity on the EEG in published cases and the lack of symptomatic response to antiepileptic therapy.1,2,11,12 However, proponents of the epileptogenic theory argue that the absence of epileptiform findings in EEG does not imply their inexistence: they simply would not be detected, either by insufficient sensitivity of the technique or by lack of “timing” during monitoring.4,5
The case described would qualify as a case of LS-TIA, but unlike other reported cases it showed clear contralateral epileptiform discharges on EEG, as well as a contralateral, parietal, and structural acute ischaemic lesion. In this case, the detection of contralateral hemispheric paroxysmal discharges coinciding with flow decrease in that hemisphere and with the clinical presence of clonisms would support the epileptogenic theory of LS-TIA, at least in some cases. We speculate that the acute cortical lesion detected on the MRI scan (not detected in other reported cases of LS-TIA) would justify the EEG findings.
Please cite this article as: Dobato J L, et al. Limb shaking: descripción de descargas epileptiformes en un caso clínico. Neurología. 2012;27:185–8.