Paraneoplastic neurological syndromes (PNS) are remote effects of cancer which may precede tumour formation. Early diagnosis of PNS is important since the outcome depends fundamentally on the identification and treatment of the primary tumour. Small cell lung carcinoma is the type of tumour most frequently associated with these syndromes, whereas laryngeal cancer is rarely correlated with PNS.1 We describe the case of a patient with a paraneoplastic sensory neuropathy (PSN) associated with laryngeal cancer.
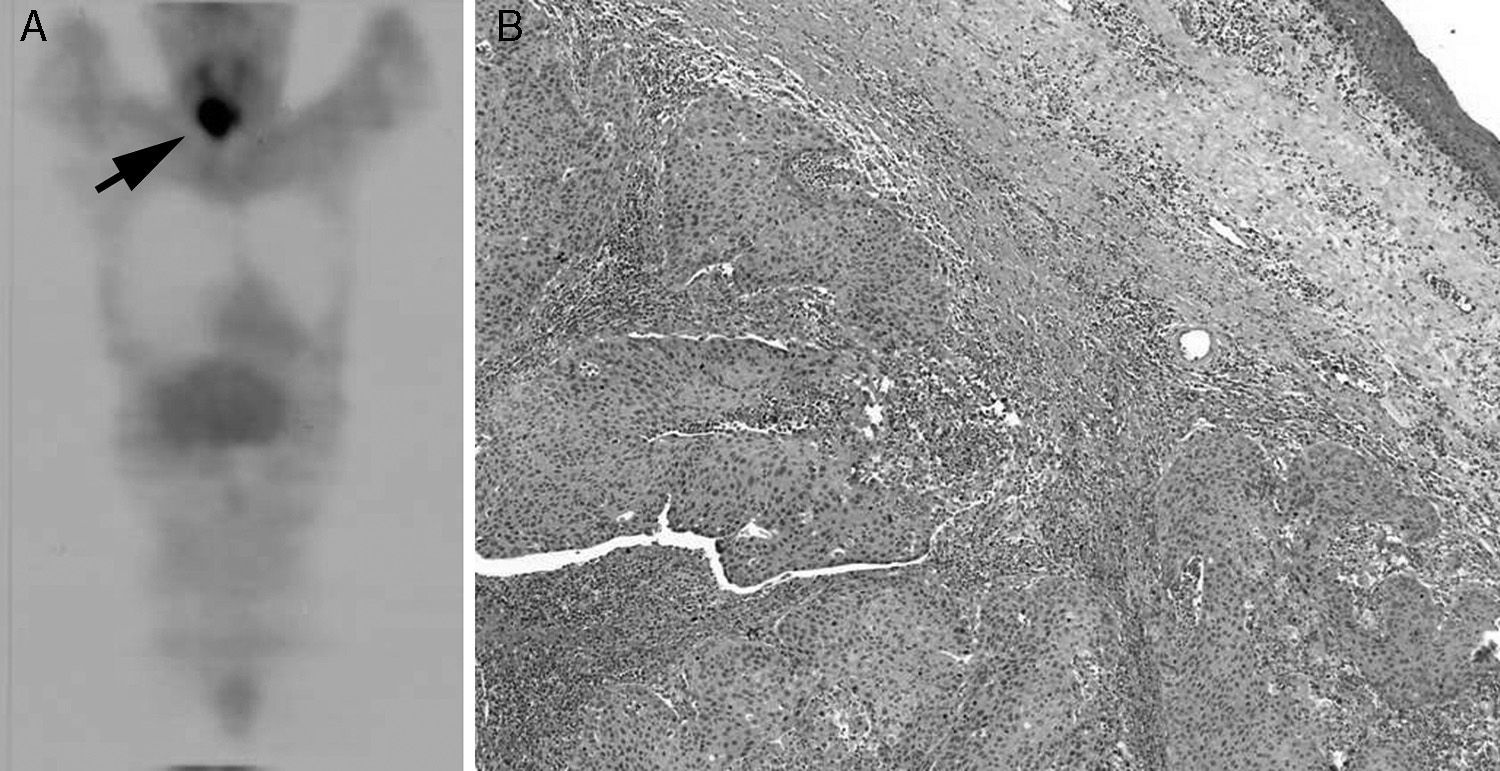
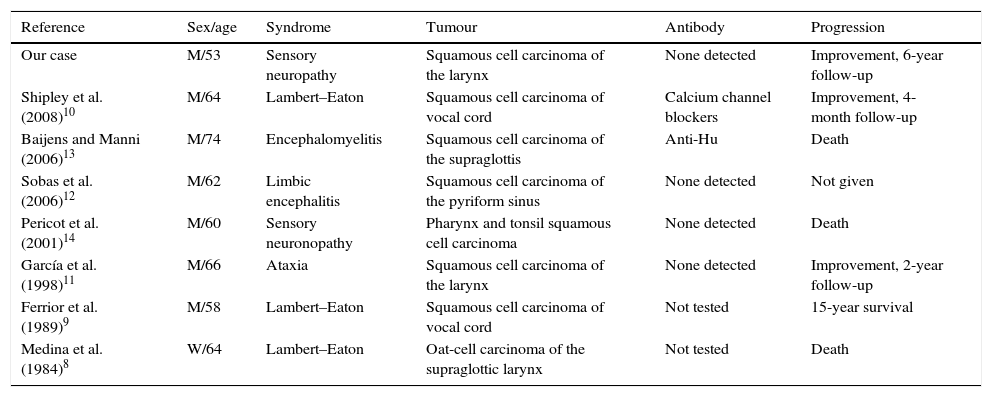
Clinical caseOur patient was a 53-year-old male smoker with a history of hypertension who visited our emergency department in September 2007 because of gait instability and progressive paraesthesia and hypoaesthesia of the hands and feet. Physical examination revealed severe loss of vibration sense and fine touch, and proprioception in hands and feet, as well as universal areflexia. The patient presented pseudoathetosis, bilateral dysmetria in all 4 limbs, and ataxic gait with no motor deficits, atrophy, or fasciculations. The visual field test and cranial nerve examination yielded normal results; language function and the remaining higher brain functions were also normal. He showed no dysphagia or dysphonia. A neurophysiological study revealed absent sensory potentials in the ulnar, median, sural, and superficial peroneal nerves. Motor nerve conduction and F-waves were normal. Cerebrospinal fluid (CSF) analysis showed pleocytosis (15leukocytes/μL, 100% mononuclear), increased protein levels (89mg/dL), and no oligoclonal bands. CSF cytology results revealed the presence of monocytes and the absence of neoplastic cells. We initiated treatment with intravenous immunoglobulins, which resulted in no clinical improvement. Tests were negative for anti-GQ1b, anti-Hu, anti-Yo, anti-Tr, anti-CV2, anti-Ri, and anti-amphiphysin antibodies. Serological tests for syphilis and ANA yielded negative results, and vitamin B12 and folic acid levels were within normal limits. Thoracic-abdominal CT scan and colonoscopy showed no alterations. Fludeoxyglucose positron-emission tomography (FDG-PET) (Fig. 1) revealed increased FDG uptake in the cervical region; no abnormal uptake was found in any other areas. Presence of a laryngeal tumour was confirmed by laryngoscopy. The patient underwent total laryngectomy followed by radiotherapy. Histological examination revealed the tumour to be an adenosquamous carcinoma. Neurological symptoms did not progress once the cancer was treated. However, the patient was left with serious sequelae including severe sensory deficit in hands and feet, and ataxic gait which obligated the use of mobility aids. The last follow-up visit to the oncology department took place in September 2013, 6 years after PSN was diagnosed; no signs of neoplasia were found in other locations.
In this patient, the diagnosis of sensory neuronopathy, or sensory ganglionopathy, was based on clinical manifestations (subacute sensory ataxia and positive sensory symptoms) and neurophysiological findings (absence of sensory potentials).2 No signs of dysautonomia, or clinical or electrical manifestations of motor neuron disease were observed. Likewise, no dysimmune, toxic, or deficiency causes were identified.3 We found a laryngeal tumour using FDG-PET, an imaging technique which is more sensitive in detecting small-sized tumours or adenopathies than conventional studies.4,5 After 6 years of follow-up, our patient has shown no signs of neoplastic disease in any other organ. We therefore established a diagnosis of PSN associated with laryngeal carcinoma according to these criteria published by Graus et al.: classical paraneoplastic neurological syndromes followed by a diagnosis of cancer, even in the absence of onconeural antibodies.6
PSN is the most frequent clinical manifestation of paraneoplastic encephalomyelitis.1 In up to 24% of patients, it may be the only neurological symptom of this syndrome, with no damage to other structures of the nervous system.7 PSN is mainly associated with small cell lung carcinoma. Only a few cases of PSN associated with laryngeal cancer have been described. The PSN more frequently associated with laryngeal cancer is Lambert–Eaton myasthenic syndrome (Table 1).8–10 The literature reports isolated cases of paraneoplastic cerebellar degeneration, encephalomyelitis, and limbic encephalitis.11–13 A very similar case to ours, describing a patient with PSN associated with cancer in the pharynx and tonsil area but no onconeural antibodies, has been published.14
Summary of the cases of paraneoplastic syndromes associated with laryngeal cancer published in the literature.
| Reference | Sex/age | Syndrome | Tumour | Antibody | Progression |
|---|---|---|---|---|---|
| Our case | M/53 | Sensory neuropathy | Squamous cell carcinoma of the larynx | None detected | Improvement, 6-year follow-up |
| Shipley et al. (2008)10 | M/64 | Lambert–Eaton | Squamous cell carcinoma of vocal cord | Calcium channel blockers | Improvement, 4-month follow-up |
| Baijens and Manni (2006)13 | M/74 | Encephalomyelitis | Squamous cell carcinoma of the supraglottis | Anti-Hu | Death |
| Sobas et al. (2006)12 | M/62 | Limbic encephalitis | Squamous cell carcinoma of the pyriform sinus | None detected | Not given |
| Pericot et al. (2001)14 | M/60 | Sensory neuronopathy | Pharynx and tonsil squamous cell carcinoma | None detected | Death |
| García et al. (1998)11 | M/66 | Ataxia | Squamous cell carcinoma of the larynx | None detected | Improvement, 2-year follow-up |
| Ferrior et al. (1989)9 | M/58 | Lambert–Eaton | Squamous cell carcinoma of vocal cord | Not tested | 15-year survival |
| Medina et al. (1984)8 | W/64 | Lambert–Eaton | Oat-cell carcinoma of the supraglottic larynx | Not tested | Death |
In conclusion, it is possible for PSN to be associated with laryngeal cancer. FDG-PET can improve cancer detection in cases of typical PSN when other screening tests yield normal results, since FDG-PET can reveal the presence of tumours in locations infrequently associated with PSN even in the absence of onconeural antibodies.
FundingThis study has received no private or public funding of any kind.
Conflicts of interestThe authors have no conflicts of interest to declare.
Please cite this article as: Erro Aguirre ME, Gila L, Olaziregui O. Neuronopatía sensitiva paraneoplásica asociada a carcinoma escamoso de laringe. Neurología. 2016;31:286–288.