The COVID-19 pandemic has resulted in complete saturation of healthcare capacities, making it necessary to reorganise healthcare systems. In this context, we must guarantee the provision of acute stroke care and optimise code stroke protocols to reduce the risk of SARS-CoV-2 infection and rationalise the use of hospital resources. The Madrid Stroke multidisciplinary group presents a series of recommendations to achieve these goals.
MethodsWe conducted a non-systematic literature search using the keywords “stroke” and “COVID-19” or “coronavirus” or “SARS-CoV-2.” Our literature review also included other relevant studies known to the authors. Based on this literature review, a series of consensus recommendations were established by the Madrid Stroke multidisciplinary group and its neurology committee.
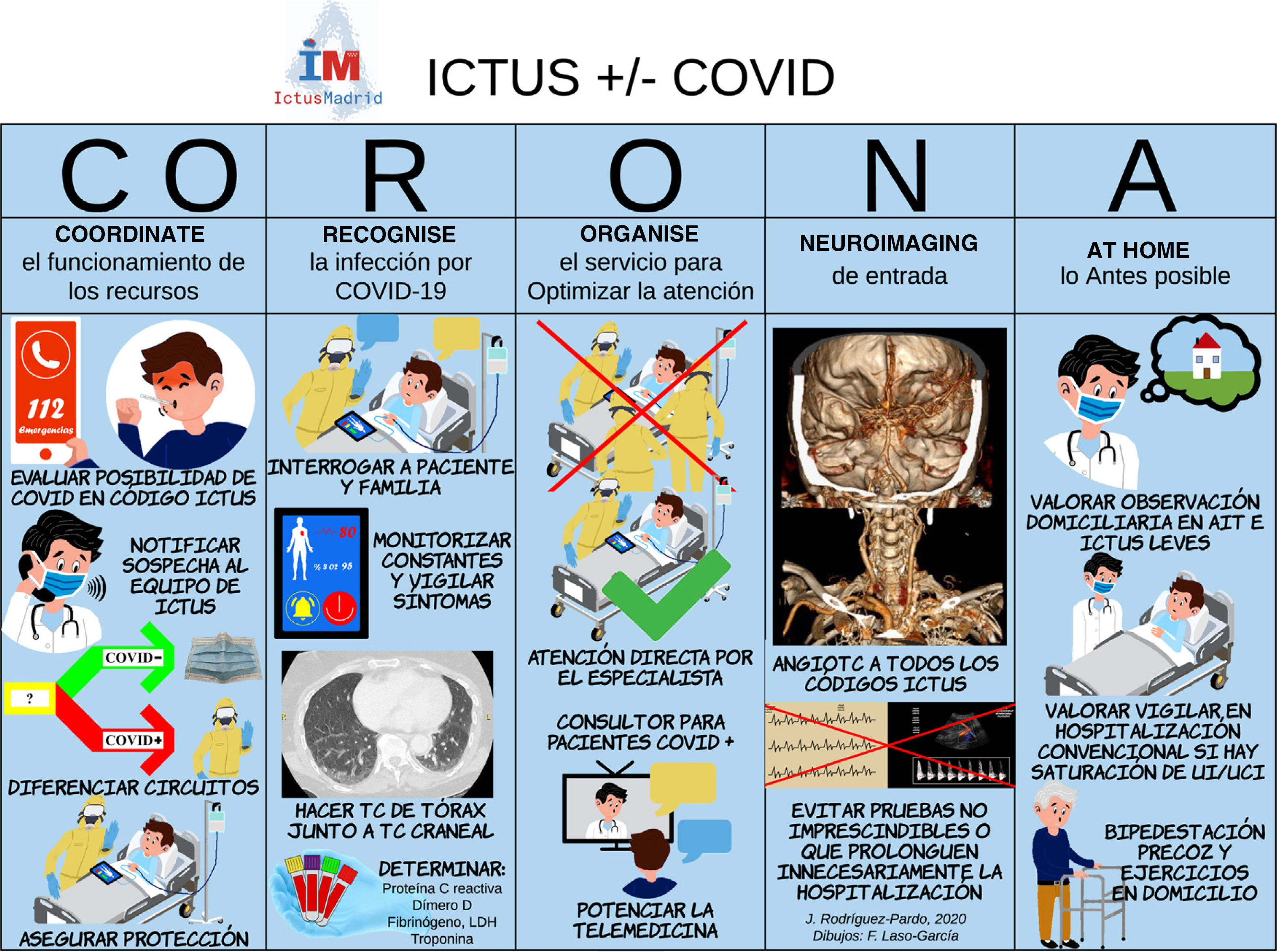
ResultsThese recommendations address 5 main objectives: (1) coordination of action protocols to ensure access to hospital care for stroke patients; (2) recognition of potentially COVID-19-positive stroke patients; (3) organisation of patient management to prevent SARS-CoV-2 infection among healthcare professionals; (4) avoidance of unnecessary neuroimaging studies and other procedures that may increase the risk of infection; and (5) safe, early discharge and follow-up to ensure bed availability. This management protocol has been called CORONA (Coordinate, Recognise, Organise, Neuroimaging, At home).
ConclusionsThe recommendations presented here may assist in the organisation of acute stroke care and the optimisation of healthcare resources, while ensuring the safety of healthcare professionals.
La pandemia por COVID-19 ha obligado a una reorganización de los sistemas sanitarios y ha comportado una saturación excepcional de sus recursos. En este contexto es vital asegurar la atención al ictus agudo y optimizar los procesos asistenciales del código ictus para reducir el riesgo de contagios y racionalizar el uso de recursos hospitalarios. Para ello, desde el Grupo Multidisciplinar Ictus Madrid proponemos una serie de recomendaciones.
MétodosRevisión bibliográfica no sistemática de las publicaciones disponibles con los términos «stroke» y «COVID-19» o «coronavirus» o «SARS-CoV-2», así como otras conocidas por los autores. En base a esta se redacta un documento de recomendaciones que es sometido a consenso por el Grupo Multidisciplinar Ictus Madrid y su Comité de Neurología.
ResultadosLas recomendaciones se estructuran en cinco líneas fundamentales: 1) coordinar la actuación para garantizar el acceso a la asistencia hospitalaria de los pacientes con ictus; 2) reconocer a los pacientes con ictus potencialmente infectados por COVID-19, 3) organización adecuada para garantizar la protección de los profesionales sanitarios frente al riesgo de contagio por COVID-19, 4) en la realización de neuroimagen y otros procedimientos que conlleven contactos de riesgo de infección COVID-19 hay que procurar reducirlos y asegurar la protección, y 5) alta y seguimiento seguros procurando optimizar la ocupación hospitalaria. Resumimos el procedimiento de forma esquemática con el acrónimo CORONA (COordinar, Reconocer, Organizar, Neuroimagen, Alta).
ConclusionesEstas recomendaciones pueden servir de apoyo para la organización del sistema sanitario en la atención al ictus agudo y la optimización de sus recursos, garantizando la protección de sus profesionales.
The COVID-19 pandemic has disrupted the normal functioning of emergency services, primary care centres, and hospitals. In view of the limitations in the availability of resources, emergency departments must improve their triage capacity to ensure that the best possible care is available for patients with the most severe conditions or requiring immediate care. The code stroke protocol provides a good example. In the hospital setting, inpatient wards are saturated and most professionals have been reallocated to care for patients with COVID-19. Hospitals must develop new care pathways to ensure that patients with acute stroke receive the necessary multidisciplinary care.
Since the beginning of the COVID-19 outbreak, several centres have reported a decrease in the number of patients with acute stroke arriving at their emergency departments, as well as delays in stroke care, particularly in more severe cases.1–3 However, this does not imply a decrease in stroke incidence, and identifying these patients continues to be essential. In the areas most affected by the pandemic, such as the region of Madrid, the number of pre-hospital code stroke activations has not decreased significantly.4 Furthermore, the incidence of neurological diseases associated with SARS-CoV-2 infection can be expected to increase during the pandemic.5
Stroke diagnostic pathways must be optimised not only to improve resource management but also to minimise the time spent by the patient at the hospital facilities and the risk of infection in patients and healthcare professionals. The demand for neurological care among patients with conditions requiring less urgent care has decreased dramatically as a consequence of the pandemic. In this context, optimising the allocation of human resources requires the unification of duties, so they can be performed by as few professionals as possible. In view of the current saturation of hospitals, it is also essential to reduce the length of hospital stays in stroke patients in order to ensure the availability of resources for other patients. In a survey of heads of neurology departments, the respondents agreed on the need to increase prevention measures, reduce in-person consultations, and promote the use of telemedicine; however, opinions on other topics, such as indications for complementary testing, were more diverse.6
This study offers a series of recommendations based on the experience of national and international healthcare centres.7–12 Recommendations were reached by consensus of the Madrid Stroke multidisciplinary group and its neurology committee.
MethodsOn 15 April 2020, we conducted a non-systematic literature review on PubMed and Embase using the keywords “stroke” and “COVID-19” or “coronavirus” or “SARS-CoV-2.” We also reviewed communications and reports from scientific societies known to the authors, as well as the references cited in these documents. Based on the information gathered in the literature review, we drafted a series of consensus recommendations agreed by experts from the Madrid Stroke multidisciplinary group and its neurology committee (Appendix B).
ResultsThe expert group analysed and evaluated the information gathered in the literature search and established a series of recommendations addressing 5 main objectives:
- 1.
Coordination of action protocols to ensure access to hospital care for stroke patients
- -
The expert group recommends developing more awareness campaigns about the importance of seeking urgent medical care in the event of stroke symptoms, even during the COVID-19 epidemic.1,8
- -
Code stroke patients must remain a priority for pre-hospital emergency services; these patients should quickly be attended and transferred to a hospital according to the stroke care protocol of the region of Madrid. The protocol includes the use of such pre-hospital stroke scales as the Madrid-DIRECT scale to identify patients eligible for thrombectomy.1,8
- -
We must ensure that emergency departments (which are likely to include temporary or external staff due to the pandemic) are familiar with the code stroke protocol.8,9
- -
We recommend promoting the use of the telestroke system to ensure early diagnosis and treatment (including intravenous thrombolysis) and avoid unnecessary transfers wherever possible.
- -
The on-call neurology service should be authorised to quickly evaluate patients with stroke and indicate the necessary diagnostic procedures and treatments, and to order transfer to another hospital, if this is essential, according to the applicable protocol.8,11
- -
Patients and their families should be involved in the decision-making process at all times, anticipating future situations to avoid the need for visits or consultations.7,11
- -
In hospitals offering mechanical thrombectomy, the endovascular surgery team and the necessary facilities and resources should be available at all times. Protocols should be developed to minimise treatment delays in patients with possible COVID-19 to ensure isolation and to avoid secondary transfers.1,7,9
- -
- 2.
Recognition of potentially COVID-19–positive stroke patients
- a.
Pre-hospital setting
- -
Patients meeting at least one of the following criteria should be considered to have possible SARS-CoV-2 infection8–10:
- a)
Cough, fever or mild fever, chest pain, dyspnoea, myalgia of over 24 hours’ duration in the previous 14 days; patients may also present headache, nausea, or gastrointestinal symptoms in the same timeframe.
- b)
Living with people with confirmed SARS-CoV-2 infection or meeting the previous criterion
- c)
Lack of data due to inability to take the patient's clinical history
- a)
- -
Screening results should immediately be communicated to the on-call neurology service so that the necessary safety measures can be implemented.
- -
- b.
Emergency departments
- -
Different care pathways should be followed for patients with and without suspected COVID-19, including the use of different emergency wards, inpatient wards, and critical care units.2,8–12
- -
Patients with suspected stroke should be screened for COVID-19; screening tools include polymerase chain reaction (PCR) studies and tests for C-reactive protein, d-dimer, fibrinogen, and troponin levels.6,8,10 Antiphospholipid antibody determination may be considered in patients with confirmed COVID-19.13
- -
Chest CT scans should be performed at the same time as emergency head CT/CT angiography in all patients with stroke to detect pulmonary involvement secondary to COVID-19. If radiological findings are compatible with COVID-19, the patient should be considered to have COVID-19.
- -
In patients eligible for thrombectomy, the endovascular neurosurgery team must be informed about whether the patient has tested negative for SARS-CoV-2. If SARS-CoV-2 infection cannot be ruled out, the necessary safety measures must be taken.12
- -
Patients with stroke should be monitored closely for fever, respiratory symptoms, dyspnoea, or oxygen desaturation during hospitalisation. Patients should be tested for SARS-CoV-2 if they present any suggestive symptoms.8,10
- -
Patients with stroke and no suspicion of COVID-19 (negative microbiological and radiological findings) must be attended according to the standard protocol established in the Madrid stroke care plan.
- -
In critical SARS-CoV-2-positive patients, the necessary support measures should be established in consensus with the departments involved (intensive care, anaesthesiology).7,10,11
- -
- a.
- 3.
Organisation of patient management to prevent SARS-CoV-2 infection among healthcare professionals
- -
The number of on-call neurologists (residents, consultants) should be adjusted to meet the centre's needs in the current situation and in accordance with objective 1, presented above.7,8,11
- -
Patients with stroke should be evaluated directly by the on-call neurologist to avoid duplicate testing and delays in decision-making, except in hospitals with specific wards for patients with COVID-19 where physicians have personal protective equipment and may therefore perform clinical examinations under the guidance of a neurologist.8,11
- -
A small group of neurologists should be designated for assessment and follow-up of patients with stroke hospitalised in specific COVID-19 wards; wherever possible, all patients should be evaluated in the same ward round to preserve stocks of protective equipment and to reduce exposure of staff.7
- -
The stroke care team should be well organised to prevent physicians from working several consecutive on-call shifts, which may lead to sleep deprivation.10,11
- -
The management of patients with stroke is often multidisciplinary, with cases discussed in clinical sessions; the use of new technologies for this purpose is highly recommended (apps, video calls, etc.).11
- -
- 4.
Avoidance of unnecessary neuroimaging studies and other procedures that may increase the risk of infection, and ensuring protection of healthcare personnel
- -
All patients with suspected stroke should undergo head CT and CT angiography; other multimodal neuroimaging techniques (perfusion, MRI) may be performed when necessary, if they are available at the centre.2,11
- -
Neurosonology studies should be avoided whenever possible.
- -
Thorough isolation measures should be implemented in patients requiring aerosol-generating procedures or other treatments that may produce respiratory droplets,7,9,12 or other procedures involving direct contact (e.g., placement of nasogastric tubes or urinary catheters).
- -
Tests that either are not essential for aetiological diagnosis or do not significantly influence treatment decisions should be postponed or omitted.7,11
- -
- 5.
Safe, early discharge and follow-up to ensure bed availability
- -
Patients with transient ischaemic attacks should be discharged as soon as possible and followed up in their homes, unless the need for an emergency intervention is foreseen.8,11
- -
Patients with stroke mimics should be discharged immediately, if the underlying condition permits this.
- -
Patients with mild stroke and those not receiving reperfusion therapy may be discharged and followed up in their homes, unless they need close monitoring.8,11
- -
If the patient's clinical situation permits it, conscious sedation should be prioritised over general anaesthesia in patients undergoing mechanical thrombectomy in order to avoid using beds in intensive care and postanaesthesia care units.12
- -
Regardless of whether they have received reperfusion therapy, patients with suspected COVID-19 requiring hospitalisation must be admitted to specific COVID-19 wards (adapted as far as possible for neurological care), unless they require admission to the intensive care unit. These patients should be monitored by the neurology department's stroke care team.2,8
- -
The use of intensive care unit beds should be limited to situations in which it is strictly necessary. If no beds are available at the stroke unit, clinically stable patients with stroke may be transferred to the neurology ward and closely monitored by the neurology department.2,8,10
- -
The aetiological study should only include tests that can be performed in a reasonably short time (<48–72h); under no circumstances should the patient be hospitalised for longer than is strictly necessary.
- -
Early discharge is encouraged for patients who can follow a rehabilitation programme at home, if their clinical situation permits this. The development of tele-rehabilitation programmes should be considered.8,11
- -
Follow-up after discharge should be based on telemedicine to avoid unnecessary visits to hospital. Consultations can be held via telephone, or through a video call system authorised by the centre, if this is necessary to complete the clinical examination.11
- -
The infographic in Fig. 1 summarises the recommendations presented in this article; the management protocol has been named CORONA (Coordinate, Recognise, Organise, Neuroimaging, At home).
Final remarksThe consensus recommendations presented in this article aim to ensure proper functioning of the code stroke protocol while minimising the risk of SARS-CoV-2 infection among patients and healthcare professionals. We hope that they may assist in organising acute stroke care and optimising healthcare resources.
FundingThis study has received no specific funding from any public, private, or non-profit organisation.
We would like to thank Fernando Laso García for his help in designing the infographic.
Exuperio Díez Tejedor (Coordinator), Department of Neurology, Hospital Universitario La Paz; Blanca Fuentes Gimeno, Department of Neurology, Hospital Universitario La Paz; Jorge Campollo, Department of Radiology (Interventional Neuroradiology section), Hospital Universitario 12 de Octubre; Roberto García Leal, Department of Neurosurgery, Hospital Universitario Gregorio Marañón; Blanca Palomino Aguado, Department of Physical Medicine and Rehabilitation, Hospital Universitario Ramón y Cajal; Mª Isabel Egocheaga Cabello, Family Medicine, Centro de Salud Isla de Oza; Jorge Gómez Cerezo, Department of Internal Medicine, Hospital Universitario Infanta Sofía; Alfonso Martín, Emergency Department, Hospital Universitario Severo Ochoa. Nicolás Riera López, SUMMA 112; Rogelio Simón, Department of Neurology (Paediatric Neurology section), Hospital Universitario 12 de Octubre.
María Alonso de Leciñana, Hospital Universitario La Paz; Joaquín Carneado Ruiz, Hospital Universitario Puerta de Hierro; Jaime Díaz Guzmán, Hospital Universitario 12 de Octubre; José Egido Herrero, Hospital Clínico Universitario San Carlos; Carlos Gómez-Escalonilla, Hospital Clínico Universitario San Carlos; Antonio Gil Núñez, Hospital Universitario Gregorio Marañón; Jaime Masjuán, Hospital Universitario Ramón y Cajal; José Vivancos Mora, Hospital Universitario La Princesa.
Both of these authors are the lead authors.
Please cite this article as: Rodríguez-Pardo J, Fuentes B, Alonso de Leciñana M, Campollo J, Calleja Castaño P, Carneado Ruiz J, et al. Atención al ictus agudo durante la pandemia por COVID-19. Recomendaciones Plan Ictus Madrid. Neurología. 2020;35:258–263.