Floating right heart thrombus preceding a thromboembolic event constitutes a rare and probably underdiagnosed finding that is almost exclusively detected in patients with severe pulmonary embolism, with an estimated incidence of 4%-18% of cases.1–3 Its prevalence in the context of stroke has not been determined. This medical emergency is associated with a mortality rate of up to 44%.1,4,5 In patients with ischaemic stroke of unknown origin, this finding is suggestive of paradoxical embolism as the cause of the stroke. We present the case of a patient with stroke of unknown cause and a floating right heart thrombus.
The patient was a 77-year-old woman with history of hypertension, dyslipidaemia, and obesity, who came to the emergency department due to complete right hemispheric syndrome upon awakening (National Institutes of Health Stroke Scale score of 18 points). A head CT scan showed no signs of early ischaemia; intra- and extracranial CT angiography revealed occlusion of the terminal segment of the right internal carotid artery, and brain perfusion maps confirmed the presence of significant ischaemic penumbra. Mechanical thrombectomy achieved complete recanalisation and immediate resolution of symptoms, except for moderate right facial and brachiocrural hemiparesis (4/5). The patient was admitted to the stroke unit with sinus rhythm.
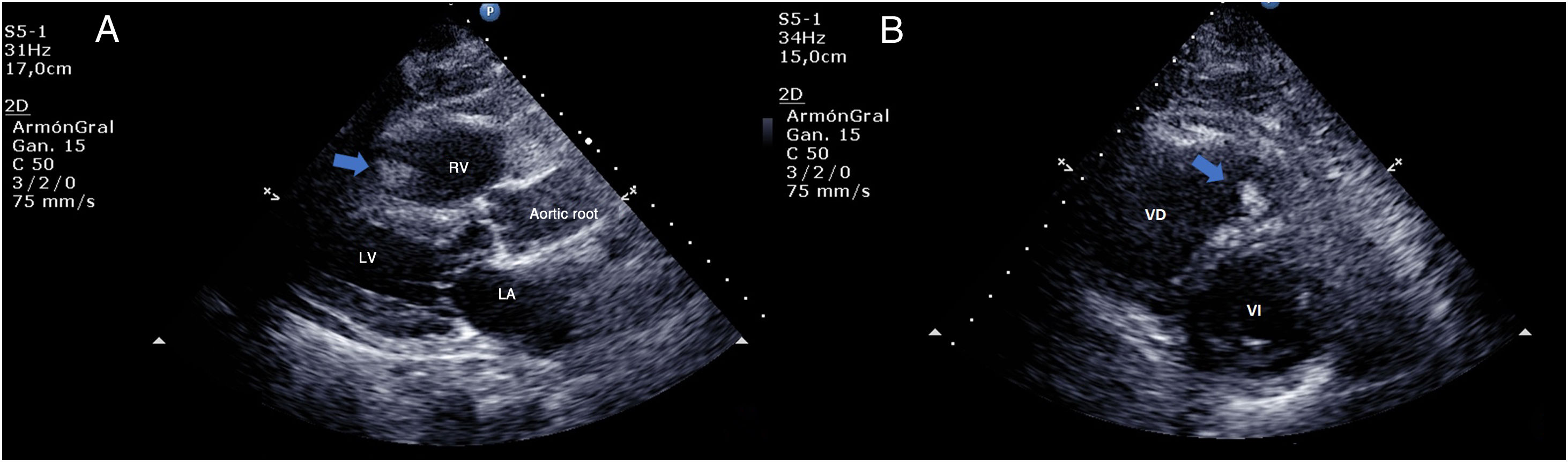
Prolonged cardiac monitoring (3 days) revealed sinus rhythm at all times except for an episode at 18 hours of admission, coinciding with symptoms of sudden dyspnoea and oxygen desaturation (88%), associated with atrial flutter of 2 hours’ duration on the electrocardiography recording. An ultrasound cardioscopy study performed at that time identified an elongated, mobile floating thrombus in the right cardiac chambers (Fig. 1); the patient was started on anticoagulation treatment with sodium heparin. A transthoracic echocardiogram performed 2 days later revealed patent foramen ovale without interatrial septal aneurysm; the floating thrombus had disappeared. A CT pulmonary angiogram confirmed the diagnosis of pulmonary thromboembolism. We hypothesise that deep vein thrombosis led to embolism of the right cardiac chambers and subsequently of the lung, and that the thrombus reached the left circulation through the patent foramen ovale, causing right internal carotid artery stroke. Symptoms subsequently resolved with treatment; at discharge, the patient continued treatment with a direct-acting oral anticoagulant.
Ultrasound cardioscopy. A) Parasternal long-axis view showing the left atrium (LA), left ventricle (LV), aortic root, and the right ventricle (RV), containing a mobile hyperechogenic mass, compatible with a floating intracavitary thrombus. B) Parasternal short-axis view showing both ventricles, the LV at the level of the mitral valve. The RV is slightly dilated and presents a hyperechogenic mass in its interior, compatible with a thrombus.
We should highlight the role of ultrasound cardioscopy in identifying intracavitary thrombi when performed in the acute phase by a vascular neurologist. Intracardiac thrombi may be classified as type A, B, or C. Type A thrombi are elongated and mobile (“floating” or “in transit”), and frequently originate from deep vein thrombosis in the legs (hence their shape). Venous Doppler ultrasound of the legs can identify type A thrombi in 90% of cases.1 Type A thrombi are the most frequent and the most emboligenic, and are associated with poorer prognosis. Type B thrombi are oval-shaped, and adhere to the vessel wall; they frequently originate in the heart, and are rarer and less emboligenic. Prognosis of these thrombi is good when treated with heparin.1,5 Type C thrombi present mixed characteristics. Our patient presented a type A thrombus.
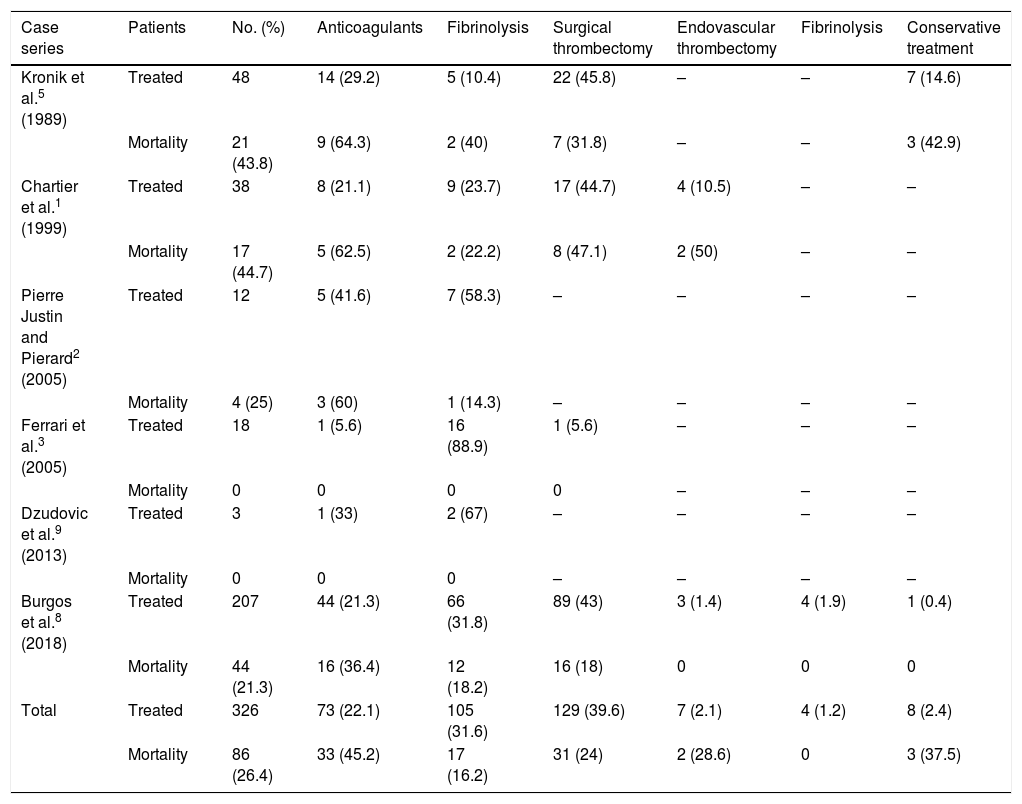
The treatment of floating thrombi is controversial. Our literature search identified 6 case series including a total of 326 cases of floating right heart thrombi in patients with pulmonary thromboembolism (Table 1).1,2,6–9 These patients were treated with heparin, fibrinolysis, surgical thrombectomy, and mechanical thrombectomy or endovascular fibrinolysis in isolated cases. Most studies are retrospective and non-randomised, and present several biases, such as selecting treatment according to severity or the physician’s preferences or using different doses or combinations of multiple treatments; there is also a lack of clinical trials. Overall, the most frequent treatment was surgery (39.6%), followed by fibrinolysis (31.6%) and anticoagulation, mainly with heparin (22.1%). Few patients received conservative treatment; most cases of conservative treatment were from over 20 years ago. Overall mortality was 26.4%, with the highest mortality rates recorded among patients receiving anticoagulants (45.2%), surgery (24%), and fibrinolysis (16.2%). The most effective treatment is still to be determined. However, the literature includes several case series in which heparin in isolation was associated with higher mortality rates than fibrinolysis or surgery for floating right heart thrombi. Other more recent series of patients with thrombi in the right cardiac chambers do not take into account the characteristics of the thrombus.4,6,7,10
Case series of floating right heart thrombi. Treatment is expressed according to intention to treat (ie, considering the first treatment administered), given that many patients received several treatments.
| Case series | Patients | No. (%) | Anticoagulants | Fibrinolysis | Surgical thrombectomy | Endovascular thrombectomy | Fibrinolysis | Conservative treatment |
|---|---|---|---|---|---|---|---|---|
| Kronik et al.5 (1989) | Treated | 48 | 14 (29.2) | 5 (10.4) | 22 (45.8) | – | – | 7 (14.6) |
| Mortality | 21 (43.8) | 9 (64.3) | 2 (40) | 7 (31.8) | – | – | 3 (42.9) | |
| Chartier et al.1 (1999) | Treated | 38 | 8 (21.1) | 9 (23.7) | 17 (44.7) | 4 (10.5) | – | – |
| Mortality | 17 (44.7) | 5 (62.5) | 2 (22.2) | 8 (47.1) | 2 (50) | – | – | |
| Pierre Justin and Pierard2 (2005) | Treated | 12 | 5 (41.6) | 7 (58.3) | – | – | – | – |
| Mortality | 4 (25) | 3 (60) | 1 (14.3) | – | – | – | – | |
| Ferrari et al.3 (2005) | Treated | 18 | 1 (5.6) | 16 (88.9) | 1 (5.6) | – | – | – |
| Mortality | 0 | 0 | 0 | 0 | – | – | – | |
| Dzudovic et al.9 (2013) | Treated | 3 | 1 (33) | 2 (67) | – | – | – | – |
| Mortality | 0 | 0 | 0 | – | – | – | – | |
| Burgos et al.8 (2018) | Treated | 207 | 44 (21.3) | 66 (31.8) | 89 (43) | 3 (1.4) | 4 (1.9) | 1 (0.4) |
| Mortality | 44 (21.3) | 16 (36.4) | 12 (18.2) | 16 (18) | 0 | 0 | 0 | |
| Total | Treated | 326 | 73 (22.1) | 105 (31.6) | 129 (39.6) | 7 (2.1) | 4 (1.2) | 8 (2.4) |
| Mortality | 86 (26.4) | 33 (45.2) | 17 (16.2) | 31 (24) | 2 (28.6) | 0 | 3 (37.5) |
Floating right heart thrombi are rarely detected prior to thromboembolic events; their prevalence in patients with acute ischaemic stroke is unknown. However, they are associated with high mortality rates, and their treatment is controversial. Future studies should aim to determine the optimal treatment for these patients. Bedside ultrasound cardioscopy performed at the stroke unit by a vascular neurologist may enable early diagnosis and treatment of floating right heart thrombi and lead to suspicion of paradoxical embolism as the cause of stroke, which improves patient prognosis.
FundingThe authors have received no funding for this study.
We would like to thank the specialist nurse Elisabet González, who performed most ultrasound studies.
Please cite this article as: Mayà-Casalprim G, Rodríguez-Vázquez A, Sarto J, Llull L. Trombo flotante en cavidades cardíacas derechas causante de embolismo pulmonar en paciente con ictus isquémico agudo. Caso clínico y revisión de la literatura. Neurología. 2020;35:661–663.