Catastrophic thought refers to a negative cognitive and emotional response to pain, and is thought to contribute to pain chronification. We aimed to evaluate pain catastrophising (PC) in a population of patients with migraine.
MethodsWe collected sociodemographic data and clinical data on migraine from patients attended at a tertiary hospital headache unit between January and June 2015. PC was measured with the Spanish-language version of the Pain Catastrophizing Scale (PCS). We compared presence of PC in patients with episodic and chronic migraine, and its correlation with clinical impact (measured by the Headache Impact Test-6 [HIT-6] scale), comorbid depression and anxiety (measured with the Hospital Anxiety and Depression Scale [HADS]), and the presence of medication overuse.
ResultsThe study included 96 patients (16 men and 80 women); 67 (69.8%) were diagnosed with chronic migraine and 29 (30.2%) with episodic migraine. Migraine impact was at least moderate (HIT-6≥56) in 85.4% of cases, and 24% exceeded the cut-off point for anxiety and 9.4% for depression. A total of 34.4% presented PC. Patients with chronic migraine scored higher than those with episodic symptoms on the HADS for anxiety (P<.001) and depression (P<.001) and on the HIT-6 (P<.001).
ConclusionsPC is common among patients with migraine. It is related to migraine severity and to comorbid anxiety and depression. PC does not appear to increase the likelihood of migraine chronification or medication overuse.
El Pensamiento Catastrófico (PC) hace referencia a un tipo de respuesta cognitiva y emocional negativa ante el dolor y se considera que contribuye a su cronificación. Pretendemos evaluar su presencia en una población de pacientes migrañosos.
MétodosPacientes atendidos en una Unidad de Cefaleas de un hospital terciario (enero-junio de 2015). Se recogieron datos sociodemográficos y características de la migraña. Se midió el PC mediante la versión española de la Pain Catastrophizing Scale (PCS). Se comparó la presencia de PC en pacientes con migraña crónica y episódica y su correlación con las medidas de impacto (Escala HIT-6), de depresión y ansiedad (Escala Hospitalaria de Ansiedad y Depresión (HADS) y la presencia de uso excesivo de medicación (UEM).
ResultadosSe incluyeron 96 pacientes (16 varones y 80 mujeres). 67 (69,8%) con Migraña Crónica (MC) y 29 (30,2%) Migraña Episódica (ME). El 85,4% presentó un impacto de la migraña al menos moderado (HIT-6≥56), el 24% superó el punto de corte para la ansiedad y el 9,4% para depresión. El 34,4 % de la muestra superó el punto de corte de la PCS. En el grupo de pacientes con PC, mayor puntuación en la escala HADS-ansiedad (p<0,001), HADS-depresión (p<0,001) y HIT-6 (p<0,001).
ConclusionesEl Pensamiento Catastrófico es frecuente en pacientes con migraña. Se relaciona con la severidad de la misma y la asociación a ansiedad y depresión. Su presencia parece no incrementar la cronificación de la migraña ni el uso excesivo de medicación sintomática.
Psychiatric comorbidity in patients with migraine has been the main focus of many recent research studies.1,2 As may be expected, the psychiatric disorders most commonly associated with migraine are affective disorders, with prevalence rates 2 to 10 times higher than in the general population; 25% of patients with migraine meet criteria for depression and anxiety.3,4
These conditions are more prevalent in patients with chronic migraine (CM) than in those with episodic migraine (EM), and are considered risk factors for migraine transformation.5–7
Another key factor in migraine transformation is pain catastrophising (PC), which is the main focus of this article. It is defined as a persistent negative cognitive and emotional response to painful sensations; patients with PC present a tendency to overestimate or exaggerate pain threat or severity. The main aspects to be considered in the assessment of this type of thought are rumination, magnification, and helplessness. Patients with PC present more intense pain, more severe anxiety and depression symptoms, increased use of analgesics, and longer hospital stays, with a significant association between pain catastrophising and pain outcomes. Neurological findings suggest that alterations in endogenous pain modulation systems and the development of a state of hyperalgesia are responsible for the relationship between emotional alterations and catastrophic processing of unpleasant sensations.8
To assist in detecting this type of thought in patients with chronic pain, Sullivan et al.8 developed the Pain Catastrophizing Scale (PCS), whose Spanish-language version has been validated in a multi-centre, observational, prospective study of patients with fibromyalgia.9
Taking this tool as a reference, and considering pain coping methods according to the catastrophising model, we analyse the usefulness of detecting and measuring PC, with a view to including it as a variable to be taken into account when assessing patients with migraine.10
Material and methodsOur study included consecutive patients visiting the headache unit of a tertiary hospital for the first time between January and June 2015. Patients were diagnosed with EM, CM, or medication overuse (MO) based on the criteria listed in the third edition of the International Classification of Headache Disorders, beta version (ICHD-3 beta).11 No patient was evaluated during a migraine event. We excluded all patients with some medical or psychiatric disorder or intellectual deficit that may limit their ability to understand or complete the questionnaire.
We prospectively recorded the sociodemographic and clinical characteristics of patients, including the number of pain days and migraine days per month, monthly consumption of symptomatic medications, years of migraine progression, and months of CM progression. We excluded patients with high-frequency EM (between 10 and 14 migraine days per month) because we consider that, although they may be classified as belonging to the group of patients with EM, their characteristics overlap with those of patients with CM. We recorded history of psychiatric disorders, drug habits, and the use of psychiatric medication or preventive treatment for migraine in the previous months.
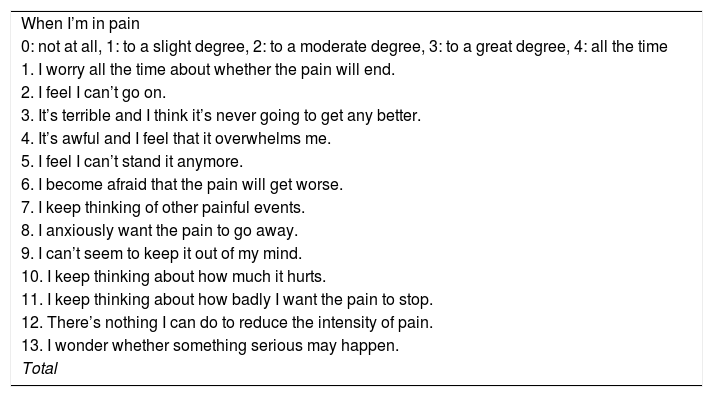
After collecting these data, we administered 3 scales, following the same order for every patient. We assessed the impact of migraine with the Headache Impact Test-6 (HIT-6),12 which establishes 4 categories of disability: severe (≥ 60), substantial (56-59), some (50-55), and no impact (≤ 49). To assess mood disorders, we used the Hospital Anxiety and Depression Scale (HADS),13 a self-administered test addressing patients’ symptoms in the previous week, which includes 14 items grouped into 2 subscales (one for anxiety and another for depression); the cut-off point for each subscale is 10 points. Finally, we used the Pain Catastrophizing Scale (PCS)9 to assess PC. In this scale, patients are asked about past painful experiences and the presence of 13 thoughts or feelings when they experience pain; each of these thoughts is assigned a score of 0 (not at all) to 4 (all the time) (Table 1). A total score (range, 0-52) is obtained from 3 subscales assessing rumination, magnification, and helplessness. Scores of 30 or higher are considered to indicate clinically significant levels of PC; this cut-off point has shown good validity in the assessment of migraine populations.14
Pain Catastrophizing Scale.
| When I’m in pain |
| 0: not at all, 1: to a slight degree, 2: to a moderate degree, 3: to a great degree, 4: all the time |
| 1. I worry all the time about whether the pain will end. |
| 2. I feel I can’t go on. |
| 3. It’s terrible and I think it’s never going to get any better. |
| 4. It’s awful and I feel that it overwhelms me. |
| 5. I feel I can’t stand it anymore. |
| 6. I become afraid that the pain will get worse. |
| 7. I keep thinking of other painful events. |
| 8. I anxiously want the pain to go away. |
| 9. I can’t seem to keep it out of my mind. |
| 10. I keep thinking about how much it hurts. |
| 11. I keep thinking about how badly I want the pain to stop. |
| 12. There’s nothing I can do to reduce the intensity of pain. |
| 13. I wonder whether something serious may happen. |
| Total |
We compared the frequency of PC and PCS scores between populations with EM and CM, correlating these values with migraine impact, presence of anxiety and depression, and MO.
We used the IBM SPSS statistical software (version 23) for data analysis; the chi-square or t test were used for hypothesis testing in the comparison of variables, as appropriate. Statistical significance was set at P<.05.
The study was approved by our hospital’s Clinical Research Ethics Committee (ref. no: 13.123), and all patients signed informed consent forms.
ResultsWe included 96 patients in the study (16 men, 80 women). Sixty-seven patients (69.8%) had been diagnosed with CM and 29 (30.2%) with EM; 52 patients (54.2%) met diagnostic criteria for MO. Mean age (standard deviation [SD]) at the time of inclusion was 37.1 (11.2) years (range, 18-70) and latency between migraine onset and assessment was 19.2 (12.7) years (range, 1-60). At the time of inclusion, patients with CM had had the condition for 53.3 (47) months (range, 3-300).
Mean score on the HIT-6 scale was 63.2 (6.6) points (range, 44-74). Substantial or severe impact (HIT-6≥56) was observed in 85.4% of patients.
Regarding HADS scores, patients scored a mean of 7.5 (4.7) (range, 0-19) on the anxiety subscale and 3.5 (4.2) (range, 0-17) on the depression subscale. Twenty-three patients (24%) scored higher than the cut-off point for anxiety and 9 (9.4%) scored higher than the cut-off point for depression.
Mean PCS score in our population was 23.6 (12.5) (range, 1-51), with 33 patients (34.4%) scoring higher than the cut-off point.
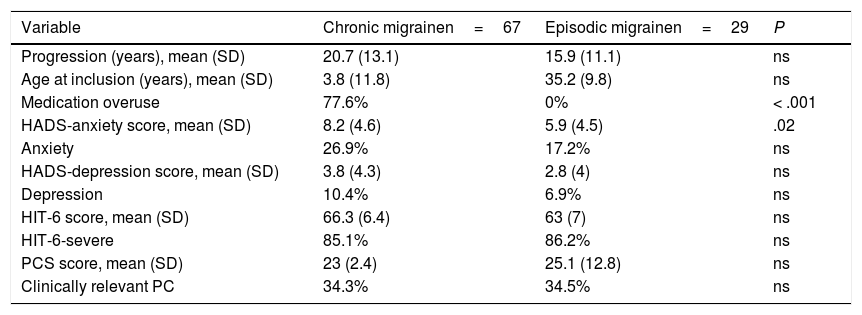
First, we compared populations with CM and EM (Table 2). Patients with CM scored higher on the HADS anxiety subscale, with no significant differences in the remaining variables analysed.
Characteristics of the patient sample by type of migraine.
| Variable | Chronic migrainen=67 | Episodic migrainen=29 | P |
|---|---|---|---|
| Progression (years), mean (SD) | 20.7 (13.1) | 15.9 (11.1) | ns |
| Age at inclusion (years), mean (SD) | 3.8 (11.8) | 35.2 (9.8) | ns |
| Medication overuse | 77.6% | 0% | < .001 |
| HADS-anxiety score, mean (SD) | 8.2 (4.6) | 5.9 (4.5) | .02 |
| Anxiety | 26.9% | 17.2% | ns |
| HADS-depression score, mean (SD) | 3.8 (4.3) | 2.8 (4) | ns |
| Depression | 10.4% | 6.9% | ns |
| HIT-6 score, mean (SD) | 66.3 (6.4) | 63 (7) | ns |
| HIT-6-severe | 85.1% | 86.2% | ns |
| PCS score, mean (SD) | 23 (2.4) | 25.1 (12.8) | ns |
| Clinically relevant PC | 34.3% | 34.5% | ns |
HADS: Hospital Anxiety and Depression Scale; HIT-6: Headache Impact Test; ns: not significant; PCS: Pain Catastrophizing Scale, PC: pain catastrophising; SD: standard deviation.
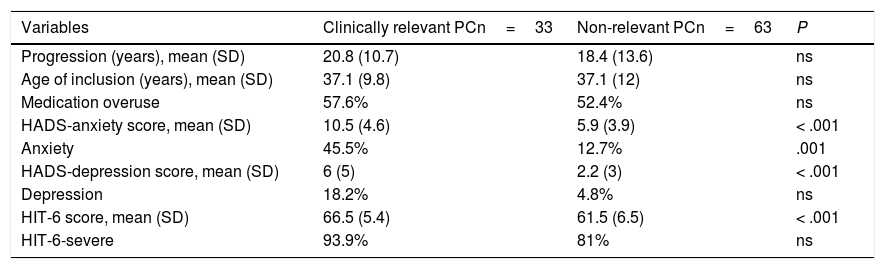
We then independently assessed the group of patients with clinically relevant PC, comparing the impact of migraine, frequency of anxiety or depression, and scores on the different scales in both populations (Table 3). We observed higher scores on the HIT-6 and HADS scales (both on the anxiety and the depression subscales) in patients with clinically relevant PC.
Comparison between patients with and without pain catastrophising.
| Variables | Clinically relevant PCn=33 | Non-relevant PCn=63 | P |
|---|---|---|---|
| Progression (years), mean (SD) | 20.8 (10.7) | 18.4 (13.6) | ns |
| Age of inclusion (years), mean (SD) | 37.1 (9.8) | 37.1 (12) | ns |
| Medication overuse | 57.6% | 52.4% | ns |
| HADS-anxiety score, mean (SD) | 10.5 (4.6) | 5.9 (3.9) | < .001 |
| Anxiety | 45.5% | 12.7% | .001 |
| HADS-depression score, mean (SD) | 6 (5) | 2.2 (3) | < .001 |
| Depression | 18.2% | 4.8% | ns |
| HIT-6 score, mean (SD) | 66.5 (5.4) | 61.5 (6.5) | < .001 |
| HIT-6-severe | 93.9% | 81% | ns |
HADS: Hospital Anxiety and Depression Scale; HIT-6: Headache Impact Test; ns: not significant; SD: standard deviation.
The association between migraine and the presence of psychological and cognitive factors that have an impact on pain is a wide field of study and has recently become the focus of many researchers. Anxiety and depression are the most widely studied psychological disorders, and have been observed more frequently in association with forms of CM, in which they favour transformation to chronic pain. Another factor that has become increasingly relevant in recent years, and also favours pain maintenance, is PC; patients with PC present a more pessimistic cognitive perception of painful sensations than those not presenting PC.
The prevalence of PC among patients with migraine in our study is similar to the rates previously described by other authors who have analysed catastrophising both in migraine and other diseases involving chronic pain.14,15 Furthermore, as may be expected,16,17 we observed a significant association between presence of clinically relevant PC and anxiety, depression, and greater migraine impact.
The risk factors involved in the transformation of EM to CM constitute another interesting field of study with a view to establishing a possible preventive approach.18 Researchers have proposed that PC may be a predictor of transformation to chronic pain in patients with significant disability or limitations associated with pain.19–21 However, in our study, neither PCS score nor the frequency of clinically relevant PC showed significant differences between the groups of patients with EM and CM. Another factor favouring transformation to chronic pain and specifically transformation of migraine is MO; our results suggest that there is no association between MO and PC. The only variable showing a difference between patients with CM and EM in our series is the presence of anxiety, identified by other authors as a factor favouring migraine transformation.19
The lack of a relevant association between catastrophising and transformation to chronic migraine seems to contradict the findings of studies suggesting an increased risk of transformation to chronic pain among patients with higher PCS scores; however, none of these studies addresses migraine pain.22,23 The results of studies assessing PC in patients with migraine coincide with ours with regard to the association between presence of catastrophising and anxiety, depression, and increased migraine impact. A study conducted in a group of women with obesity and migraine suggested that PC favours transformation to chronic migraine14; a study with a more heterogeneous group of patients, which resembled ours in terms of sample size and the recruitment of patients from a tertiary hospital, did not replicate this association.16 Studies including patients from tertiary hospitals probably incur a selection bias, which may result in greater migraine impact in patients with EM; in fact, HIT-6 scores in our series were similar in both patient groups.
Our study has a number of limitations, including the small size of our sample. Due to its cross-sectional design, we cannot assess the true relevance of PC in favouring transformation to chronic migraine; this analysis would have been possible with a longitudinal study. In our analysis, we did not consider such sociodemographic variables as the patients’ family setting or level of education. Finally, our study presents some differences with other studies in the batteries used to assess mood disorders and the impact of migraine.17
It is difficult to establish recommendations for clinicians regarding management of PC. The psychotherapeutic or psychosocial approaches proposed to date are outside the scope of a standard consultation. Being aware of the presence of PC and correctly informing patients with migraine about the multiple therapeutic resources available and the absence of risks of developing other health problems may at least prevent worsening of PC.
ConclusionIn conclusion, clinically relevant PC is frequently present in patients with migraine. Although this phenomenon has not been clearly established as a risk factor for migraine transformation, its presence seems to be associated with mood disorders and greater migraine impact.
Our next step in this line of research will be to assess whether catastrophising has an impact on patients’ response to symptomatic or preventive treatments for migraine. In the future, presence of PC may be considered one of the variables to consider when recommending a psychotherapeutic approach for patients with migraine.
Conflicts of interestThe authors have no conflicts of interest to declare.
This study has received no specific grant from any public, commercial, or non-profit agency.
Please cite this article as: Alvarez-Astorga A, García-Azorín D, Hernández M, de la Red H, Sotelo E, Uribe F, et al. Pensamiento catastrófico ante el dolor: presencia en una población de migrañosos. Neurología. 2021;36:24–28.
Part of this study was presented as an oral communication at the 67th Annual Meeting of the Spanish Society of Neurology, Valencia, November 2015.