Sinus pericranii (SP) is an infrequent vascular malformation consisting of direct venous communication between the intracranial dural sinuses and epicranial veins, causing varicose dilation of these veins.1 The literature reports approximately 200 cases, half of which were diagnosed before the second decade of life.2 Diagnosis in early childhood is infrequent. We present the case of an infant presenting the malformation from birth.
The patient was a 2-month-old boy with no relevant history and normal psychomotor development for his age. From birth, a soft purplish nodule of 3mm diameter was present on the scalp; its size fluctuated with Valsalva manoeuvres and crying (Fig. 1).
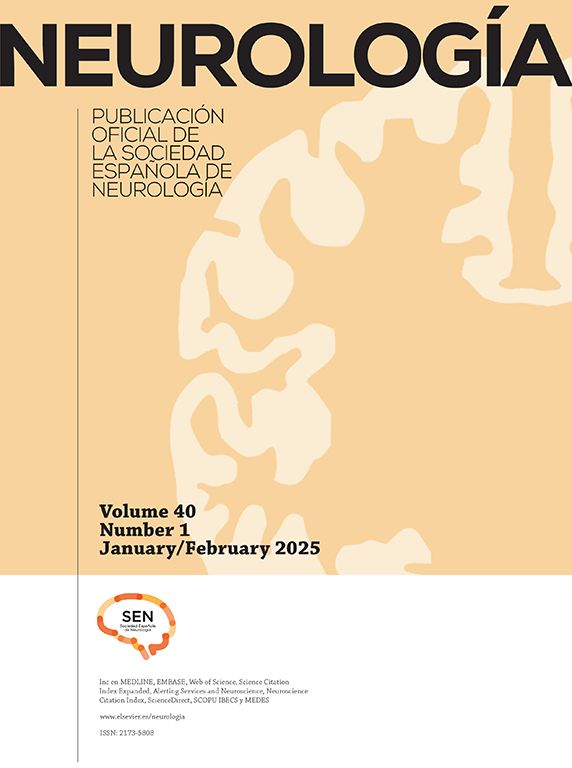
(A) Sagittal T2-weighted MRI sequence. The white arrow (signal voids) points to the varicose vein draining to the sagittal sinus. (B) Coronal slice at the level of the varicose vein (white arrow). Protrusion is observed at the surface. (C) Axial sequence showing the lesion at the midline. (D) External appearance of the Sinus pericranii. A macule is visible on the scalp; its size fluctuated during examination.
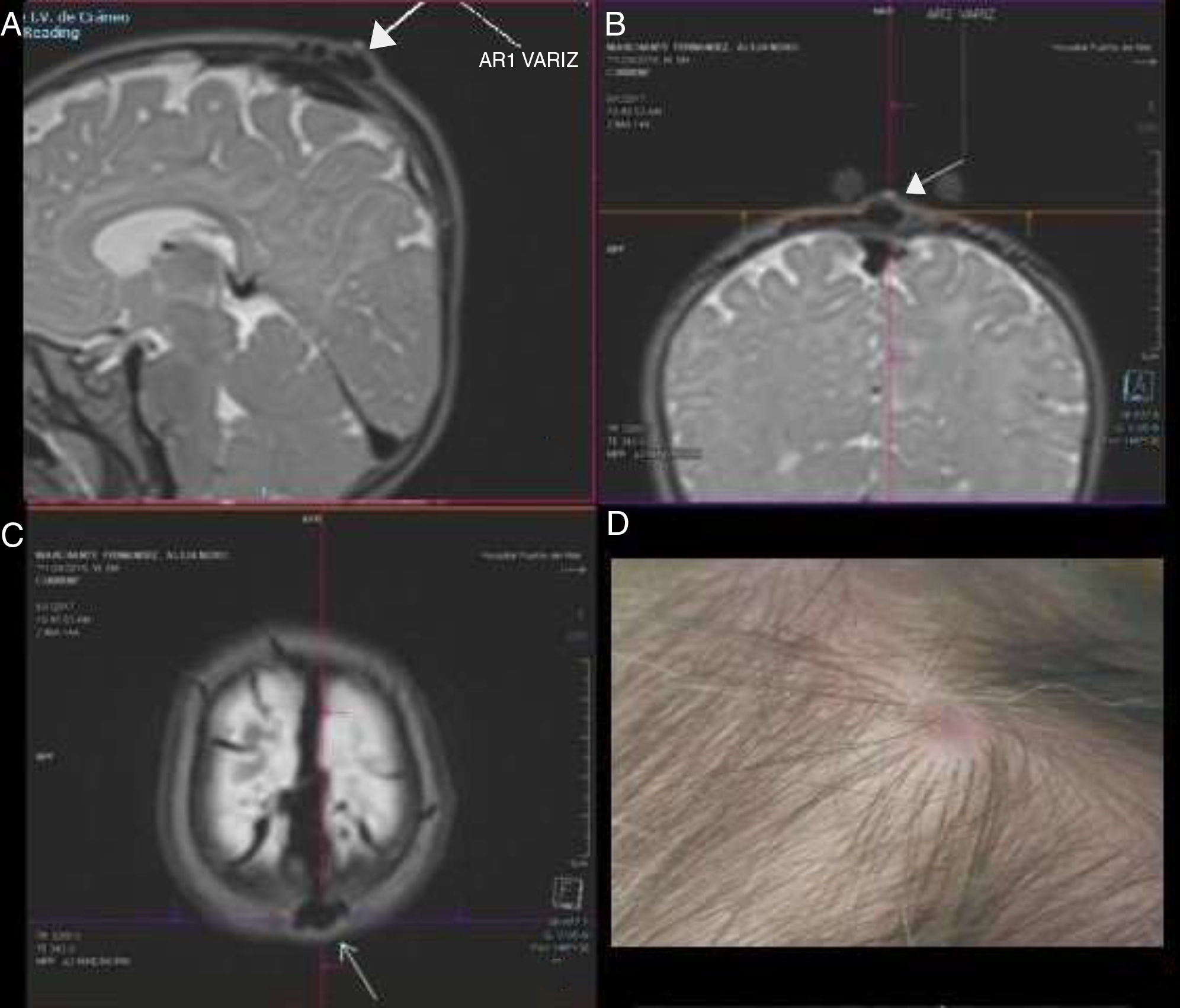
A cranial Power Doppler ultrasound showed a vascular lesion that increased in size with crying, draining into the superior sagittal sinus. Given suspicion of SP, we performed a non-contrast-enhanced MRI angiography of the venous sinus, with maximum intensity projection reconstruction. The study confirmed the vascular communication, showing a varicose vein draining into a pericranial vein, both of small size and located on the scalp. The varicose vein was receiving venous blood from the superior sagittal sinus through a transosseous vein. We opted for conservative treatment considering the patient's age and the characteristics of the malformation. The patient is currently asymptomatic and no changes have been observed in the lesion.
SP is the most frequent venous anomaly observed in diploic veins.3 The most frequent location is the midline, especially in the frontal region, although other locations have also been described.4,5 Most cases are congenital, due to probable transient hypertension during the embryonic period.3 However, diagnosis is usually delayed. The most frequent secondary causes include head trauma, which causes avulsion of the emissary veins.3,6 Our patient presents a congenital SP and is one of the earliest diagnosed cases in the literature.
From a clinical viewpoint, progression is usually asymptomatic; examination typically reveals a bluish tumour of soft consistency that increases in size with Valsalva manoeuvres. Cases related to headache, skin pain, seizures, nausea, vertigo, ataxia, etc. have been described in adults.3,7–9 Furthermore, SP has been related to some vascular and lymphatic malformations or to syndromic symptoms, which was not the case in our patient.3,4,7,10
Diagnosis is clinical, although it is confirmed with radiology. There is no consensus on the test of choice. Computed tomography scans display associated bone defects, and magnetic resonance imaging is useful to rule out accompanying venous malformations (Fig. 1).11–13 MR angiography provides the highest sensitivity; in our case, these images were very characteristic and were valuable in selecting the management approach (Fig. 2). Doppler ultrasound is a non-invasive method of visualising blood flow; in our patient, it was essential to orient the diagnosis. More cutting-edge techniques, such as digital subtraction angiography, show high sensitivity and more precise haemodynamic evaluation. Differential diagnosis includes other vascular malformations,14 eosinophilic granulomas, epidermoid tumours, meningoceles, encephaloceles, and traumatic leptomeningeal cysts.1,4
Most reported cases support conservative treatment, with treatment performed for aesthetic reasons.9 Some studies discuss performing the intervention to prevent complications. These authors advocate the block resection of the cranial mass with ligation of the communicating vessels, although this is contraindicated when SP is part of the main cerebral venous drainage. Haemorrhage is the most frequent complication.1,7
After assessing the risks and benefits of the treatment, we deem it reasonable to maintain a watchful waiting approach in asymptomatic patients. Published cases report good progression and prognosis, with no neurological deficits or reappearances in cases of intervention.15
Please cite this article as: Lubián-Gutiérrez M, Sánchez-Códez MI, Peromingo-Matute E, Zuazo-Ojeda A. Sinus pericranii: diagnóstico precoz en el lactante. Neurología. 2020;35:70–72.