The aim of this study was to develop and validate a Spanish-language version of the Scale for Contraversive Pushing, used to diagnose and measure pusher behaviour in stroke patients.
MethodsTranslation–back translation was used to create the Spanish-language Scale for Contraversive Pushing; we subsequently evaluated its validity and reliability by administering it to a sample of patients. We also analysed its sensitivity to change in patients identified as pushers who received neurological physiotherapy.
ResultsExperts indicated that the content of the scale was valid. Internal consistency was very good (Cronbach's alpha of 0.94). The intraclass correlation coefficient showed high intra- and interobserver reliability (0.999 and 0.994, respectively). The Kappa and weighted Kappa coefficients were used to measure the reliability of each item; the majority obtained values above 0.9. Lastly, the differences between baseline and final evaluations of pushers were significant (paired sample t test), showing that the scale is sensitive to changes obtained through physical therapy.
ConclusionsThe Spanish-language version of the Scale for Contraversive Pushing is valid and reliable for measuring pusher behaviour in stroke patients. In addition, it is able to evaluate the ongoing changes in patients who have received physical therapy.
El objetivo de este estudio es traducir y validar al español la Scale for Contraversive Pushing, usada para diagnosticar y medir el comportamiento empujador en pacientes que han sufrido un ictus.
MétodosSe realizó una traducción-retrotraducción de la Scale for Contraversive Pushing para la población española y, posteriormente, se evaluó la validez y fiabilidad de la misma a partir de una muestra de pacientes. Además, se analizó la sensibilidad al cambio en pacientes que resultaron ser empujadores y recibieron tratamiento de fisioterapia neurológica.
ResultadosLas respuestas de los expertos indicaron que la escala era válida en cuanto a su contenido. La consistencia interna, medida a través del alfa de Cronbach, obtuvo un resultado de 0,94. La fiabilidad intraobservador e interobservador, calculada por medio del coeficiente de correlación intraclase, presentó un valor de 0,999 y 0,994 respectivamente. Cuando se analizó la fiabilidad de cada ítem, por medio del coeficiente de kappa o kappa ponderado, la mayoría de ellos obtuvo una puntuación superior a 0,9. Por último, las diferencias obtenidas entre la valoración inicial y final de los pacientes empujadores fueron significativas (t de Student pareada), objetivando que la escala era sensible a los cambios obtenidos tras un tratamiento de fisioterapia.
ConclusionesLa Scale for Contraversive Pushing es válida y fiable para medir el comportamiento empujador en pacientes que han sufrido un ictus. Además, es capaz de evaluar los cambios ocurridos en los pacientes, tras recibir tratamiento de fisioterapia.
Pusher behaviour was first defined in 1985 as a set of symptoms characterised by pushing strongly towards the hemiplegic side in all positions and resisting any attempt at passive correction, i.e., correction of posture to bring the weight towards or over the midline of the body to the unaffected side.1 Contraversive pushing is mainly seen in patients with stroke,2 although it can also affect patients with head trauma or brain tumours3 affecting the thalamus or internal capsule.2,4,5 Distortion of the perceived midline6–8 results in loss of postural control, which negatively affects performance in the activities of daily living.9,10 Furthermore, pusher behaviour is frequent in patients who also present hemispatial neglect11 when lesions affect the brain regions involved in both alterations, which are located very close to one another.12
Its incidence ranges from 10.4% to 60%, according to the literature. This variability is explained by the wide range of diagnostic scales used, lesion types, and progression times of the patients included in each study.2,3,9,13 Pushing syndrome usually has a good prognosis, with most cases resolving within 6 months,14 although some authors report that it may persist for at least 2 years.15 Pushers tend to show higher levels of dependence or slower recovery from physical sequelae9,16,17: they need a mean of 3.6 weeks of additional treatment to reach the same functional outcome as other patients.9
Pusher behaviour may be misinterpreted as Wallenberg syndrome18,19 or hypercompensation of the less affected side. Different scales have been developed to accurately diagnose the condition and to measure the effects of rehabilitation. The most widely used is the Scale for Contraversive Pushing (SCP),20 a valid, reliable tool21 with items evaluating the main characteristics of pusher behaviour according to Davies1; the scale has been validated in Sweden, with good results.22 To our knowledge, the scale has not been validated to Spanish.
Given that pusher behaviour may delay recovery, and in view of the importance of establishing an accurate diagnosis, our study aimed to translate into Spanish and to validate the SCP for evaluating pusher behaviour in patients with stroke, and to evaluate the scale's sensitivity to change in a sample of patients.
Patients and methodsOur study was approved by the ethics committees of the School of Nursing, Physiotherapy, and Podology of Universidad Complutense de Madrid and the brain injury unit at Clínica San Vicente (Madrid). Patients were recruited from the latter centre. The validation process comprised 2 stages. We first translated into Spanish and validated the scale, and subsequently evaluated the scale's sensitivity to change in a group of patients displaying pusher behaviour.
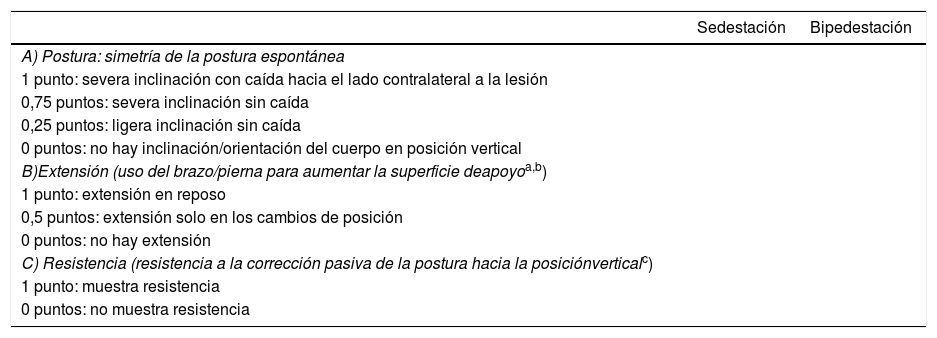
During the first stage, we conducted a cross-sectional psychometric study. Permission was obtained from the author of the original scale (Dr Karnath) and the scale was translated from English to Spanish by 2 independent physiotherapists specialising in neurology who were native Spanish speakers bilingual in English.23,24 A review committee comprising 3 physiotherapists specialising in neurology and an expert in Spanish philology generated a single Spanish translation, which was back-translated by 2 independent physiotherapists specialising in the topic, who were native English speakers bilingual in Spanish. The review committee evaluated this back-translated version to create the final Spanish-language version of the scale (Table 1).
Spanish-language version of the Scale for Contraversive Pushing.
| Sedestación | Bipedestación | |
|---|---|---|
| A) Postura: simetría de la postura espontánea | ||
| 1 punto: severa inclinación con caída hacia el lado contralateral a la lesión | ||
| 0,75 puntos: severa inclinación sin caída | ||
| 0,25 puntos: ligera inclinación sin caída | ||
| 0 puntos: no hay inclinación/orientación del cuerpo en posición vertical | ||
| B)Extensión (uso del brazo/pierna para aumentar la superficie deapoyoa,b) | ||
| 1 punto: extensión en reposo | ||
| 0,5 puntos: extensión solo en los cambios de posición | ||
| 0 puntos: no hay extensión | ||
| C) Resistencia (resistencia a la corrección pasiva de la postura hacia la posiciónverticalc) | ||
| 1 punto: muestra resistencia | ||
| 0 puntos: no muestra resistencia |
En sedestación, pedir al paciente que deslice su glúteo por la camilla hacia el lado no afecto, para realizar la trasferencia de la cama a la silla hacia el lado sano o ambos.
To confirm the viability of the Spanish-language version and the time needed to perform the assessment, an independent rater unfamiliar with the original scale evaluated whether it was easily understandable, analysed its content, and administered it to a patient with stroke who met the study's inclusion criteria, in order to evaluate the scale's reliability.25–28 The inclusion criteria were as follows: age between 18 and 90 years, stroke diagnosed at a neurology department, inclusion between 7 days and 6 months from stroke diagnosis,14 first-ever stroke, and informed consent to participate. The exclusion criteria were as follows29,30: lack of cooperation during assessment due to agitation or somnolence, bilateral involvement of stroke, dependence in activities of daily living prior to stroke, and history of orthostatic hypotension or orthopaedic disorders.
To assess the scale's psychometric properties, we first evaluated content validity with the Delphi method,23,31 with a panel of 10 experts expressing their opinions on the content of the scale. The panel was formed by physiotherapists experienced in treating this type of patients in different fields. During the exploratory phase, a 5-point Likert-type scale was used to ask experts whether each item was appropriate for measuring pusher behaviour. They were also asked an open-ended question on their opinions about the scale. Finally, results were synthesised.
We then analysed inter- and intraobserver reliability in a sample of patients. To calculate the sample size needed to evaluate reliability with the intraclass correlation coefficient (ICC), we used a 95% confidence interval and 2 observers or 2 intraobserver measurements. For an anticipated reliability of ≥ 0.9 and 83% probability of achieving a reliability ≥ 0.8, the minimum sample size was 50 patients.32 All eligible patients were informed of the purpose of the study and confidentiality of personal data was guaranteed; patients signed informed consent forms prior to inclusion in the study. During the recruitment phase, the inclusion and exclusion criteria were applied to a total of 57 patients, 50 of whom were finally included in the study. We gathered the following data from our sample: age, sex, lesion type, hemisphere involved, stroke location according to the Oxfordshire Community Stroke Project (OCSP) classification,33 and time since the stroke.
To evaluate intraobserver reliability, the scale was administered twice by a single physiotherapist, on 2 consecutive days. To evaluate interobserver reliability, another physiotherapist administered the scale to the same patient on the day between assessments by the first physiotherapist; the second physiotherapist was blinded to results from the previous day.29 All physiotherapists administering the scale were trained in neurological physiotherapy and experienced in treating neurological patients; they were trained to administer the scale before the study began.34
Data were analysed using the SPSS (version 22.0; IBM Corp., Armonk, NY, USA) and SAS statistical software (version 9.4; SAS Institute Inc., Cary, NC, USA). To evaluate the scale's psychometric properties, we used the ICC and the kappa and weighted kappa coefficients to calculate intra- and interobserver reliability; internal consistency was measured with the Cronbach alpha statistic.
During the second stage of the study, we evaluated the scale's sensitivity to change using those patients from the initial sample who were found to display pusher behaviour; as an additional inclusion criterion, they had to score more than 0 on all sections (A, B, and C) of the SCP30,35 (Table 1). Only 12 patients from the initial sample met the diagnostic criteria for pushing syndrome and received neurological physiotherapy; treatment aimed to reduce the associated complications. With the help of a physiotherapist, patients actively performed functional activities focused on placing weight on the non-paretic side; when possible, early standing and walking was also promoted.1,36 Each patient completed a total of 30 sessions lasting 50 minutes each (5 sessions per week). We analysed the mean difference between scores in the initial and final assessments using the paired-samples t test, both for global scores and for item subscores. The Bonferroni correction was applied to P values associated with changes in items. Effect size was calculated using Cohen's d.
ResultsOur sample included 50 patients with a mean (SD) age of 64.32 (12.77) years; 52% were men. Ischaemic strokes accounted for 56% of cases; the remaining 44% were haemorrhagic. According to the OCSP classification,33 70% of patients showed partial anterior circulation infarct, whereas 22% had posterior circulation infarct and 4% showed lacunar infarct. Lesions affected the right hemisphere in 52% of the patients; 84% were in the subacute phase of stroke, with less than 3 months of progression37 and a mean (SD) time of 59.7 (35.36) days between stroke diagnosis and assessment of pusher behaviour.
Content validity was determined according to the responses of the experts, who judged the relevance of each item for evaluating pusher behaviour (Table 2). Some of the experts’ observations in response to the open-ended question were as follows: “Although the test is useful for assessing contraversive pushing, in my opinion it does not cover all the aspects necessary for a good differential diagnosis”; “The difference between mild and severe is subjective”; “I recommend assessing pusher behaviour with the patient in the supine position; in extreme cases, pushing is so strong that it also affects the head”; “I would assess the transition from sitting to standing, since most patients who do not display pusher behaviour while seated do display contraversive pushing while getting up from a sitting position and cannot hold their stance.”
Opinions of the expert panel.
| Item | Frequency | Cumulative frequency | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| C1 | C2 | C3 | C4 | C5 | Total | C1 | C2 | C3 | C4 | C5 | |
| Item A (sit.) | 0 | 0 | 0 | 2 | 8 | 10 | 0 | 0 | 0 | 2 | 10 |
| Item A (sta.) | 0 | 0 | 1 | 4 | 5 | 10 | 0 | 0 | 1 | 5 | 10 |
| Item B (sit.) | 0 | 0 | 4 | 0 | 6 | 10 | 0 | 0 | 4 | 4 | 10 |
| Item B (sta.) | 0 | 0 | 4 | 2 | 4 | 10 | 0 | 0 | 4 | 6 | 10 |
| Item C (sit.) | 0 | 0 | 0 | 0 | 10 | 10 | 0 | 0 | 0 | 0 | 10 |
| Item C (sta.) | 0 | 0 | 0 | 0 | 10 | 10 | 0 | 0 | 0 | 0 | 10 |
C1: category 1, “absolutely inappropriate”; C2: category 2, “slightly inappropriate”; C3: category 3, “neutral”; C4: category 4, “slightly appropriate”; C5: category 5, “absolutely appropriate”; sit.: sitting; sta.: standing.
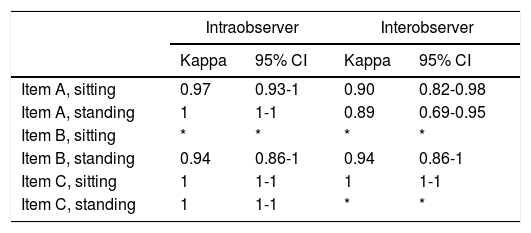
The reliability analysis (Cronbach alpha) revealed an internal consistency of 0.94. ICCs for intra- and interobserver reliability were 0.999 and 0.994, respectively, with slightly superior 95% confidence intervals for intraobserver reliability (0.997-0.999, vs 0.990-0.997 for interobserver reliability). When analysing each item separately, most kappa (section C) and weighted kappa coefficients (sections A and B) were above 0.9 (Table 3).
Reliability study using the weighted kappa coefficient for sections A and B, and the kappa coefficient for section C.
| Intraobserver | Interobserver | |||
|---|---|---|---|---|
| Kappa | 95% CI | Kappa | 95% CI | |
| Item A, sitting | 0.97 | 0.93-1 | 0.90 | 0.82-0.98 |
| Item A, standing | 1 | 1-1 | 0.89 | 0.69-0.95 |
| Item B, sitting | * | * | * | * |
| Item B, standing | 0.94 | 0.86-1 | 0.94 | 0.86-1 |
| Item C, sitting | 1 | 1-1 | 1 | 1-1 |
| Item C, standing | 1 | 1-1 | * | * |
95% CI: 95% confidence interval.
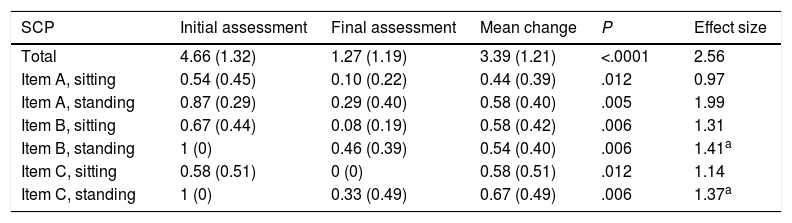
The scale was found to be sensitive to change; the sitting position item in section A was the least sensitive to change, and all differences between the initial and final assessments were statistically significant. All items showed a large effect size; effect size was considerably larger for global score (Table 4).
Differences between the initial and the final assessment.
| SCP | Initial assessment | Final assessment | Mean change | P | Effect size |
|---|---|---|---|---|---|
| Total | 4.66 (1.32) | 1.27 (1.19) | 3.39 (1.21) | <.0001 | 2.56 |
| Item A, sitting | 0.54 (0.45) | 0.10 (0.22) | 0.44 (0.39) | .012 | 0.97 |
| Item A, standing | 0.87 (0.29) | 0.29 (0.40) | 0.58 (0.40) | .005 | 1.99 |
| Item B, sitting | 0.67 (0.44) | 0.08 (0.19) | 0.58 (0.42) | .006 | 1.31 |
| Item B, standing | 1 (0) | 0.46 (0.39) | 0.54 (0.40) | .006 | 1.41a |
| Item C, sitting | 0.58 (0.51) | 0 (0) | 0.58 (0.51) | .012 | 1.14 |
| Item C, standing | 1 (0) | 0.33 (0.49) | 0.67 (0.49) | .006 | 1.37a |
SCP: Scale for Contraversive Pushing.
Data are expressed as means (standard deviation).
P values were calculated with the t test for paired samples. The Bonferroni correction was applied to all item results. Effect size: Cohen's d.
Our results suggest that the SCP is a valid tool, meaning that the items included in the scale adequately evaluate pusher behaviour in patients with stroke. The last 2 items were rated the highest by the expert panel; these items evaluate resistance to passive correction of tilted posture in both sitting and standing positions. This may be due to the fact that the last 2 items focus on one of the main features of contraversive pushing,1 and are also helpful in differential diagnosis. In response to the open-ended question, experts indicated that the SCP was insufficient for differential diagnosis and suggested that additional items be included, such as assessment of pusher behaviour in the supine position or during transition from sitting to standing. No study has evaluated the content validity of the original scale; therefore, our findings cannot be compared to those of other authors. However, several studies suggest that the scale may be useful for identifying patients with pusher behaviour despite failing to recognise some cases due to the lack of items evaluating contraversive pushing in the decubitus position or while walking, for example.38–40
Our results show that the Spanish-language version of the SCP has excellent reliability; in fact, it has greater reliability than the version validated in Sweden,22 with an ICC for global scale score of 0.994, vs 0.84 of the Swedish version. Furthermore, the Swedish researchers only calculated interobserver reliability for the first 2 sections, which assess spontaneous body posture and extension of the non-paretic limbs. The original scale shows similar interobserver reliability to that of our version (ICC=0.94), as well as similar internal consistency (Cronbach alpha coefficient of 0.91 in the original version and 0.94 in the Spanish-language version). These results are consistent with those of other validation studies including similar samples.34,41 The Spanish-language version also has slightly better inter- and intraobserver reliability than the Burke Lateropulsion Scale (BLS),29 another instrument for assessing contraversive pushing, which has ICCs of 0.93 and 0.94, respectively.
In terms of the scale's sensitivity to change, statistically significant differences were detected between scores obtained during the initial and final assessments, which suggests that the scale is useful for identifying changes caused by physiotherapy. According to other studies, however, the SCP is not useful for evaluating treatment effectiveness.30,38,39,42 In a study into the effects of physiotherapy on pusher behaviour, only the BLS was able to detect differences between pre- and post-treatment values, and the authors concluded that the BLS was the only instrument with sufficient sensitivity to change.40 This may be due to the fact that measurements were taken immediately after the physiotherapy session, which prevents comparisons being made against our own results. Despite these findings, the SCP is the most widely used tool for measuring the effects of physiotherapy on contraversive pushing36,38,43–45; while our study does present limitations, our results support the usefulness of the scale.
One limitation of the study is that we were unable to measure the scale's criterion validity, since no other instrument measuring pusher behaviour has been validated in Spanish. It would be interesting to establish correlations between the Spanish-language SCP and other scales measuring pusher behaviour. Furthermore, sensitivity to change was evaluated only in a small subsample; these results should therefore be interpreted with caution.
ConclusionsThe Spanish-language version of the SCP is valid and reliable for measuring pusher behaviour. Future studies should include larger samples to determine whether the scale can detect mild pusher behaviour and whether it is sufficiently sensitive to changes caused by physical therapy.
FundingThis study has received no external funding of any kind.
Conflicts of interestNone of the authors has any financial or personal relationship with other persons or organisations that may create conflicts of interest with regard to this article.
We wish to thank the brain injury unit at Clínica San Vicente for providing personnel and material support. This study would not have been possible without the participation of our patients and their families.
Please cite this article as: Martín-Nieto A, Atín-Arratibel MÁ, Bravo-Llatas C, Moreno-Bermejo MI, Martín-Casas P. Traducción y validación española de la Scale for Contraversive Pushing (SCP) para la valoración del comportamiento empujador. Neurología. 2021;36:577–583.