Arachnoid cysts are collections of cerebrospinal fluid (CSF) surrounded by an arachnoid membrane which is histologically indistinguishable from healthy arachnoid.1 Radiology studies display them as extra-axial lesions with liquid content and the same characteristics as CSF in the different sequences used in magnetic resonance imaging (MRI). They do not show contrast uptake. Most are congenital in origin, although cases secondary to infection or trauma have also been described. They are most frequently located in the supratentorial compartment,2 whereas spinal arachnoid cysts are rare. Most cysts are diagnosed incidentally when neuroimaging tests are being performed. When they are symptomatic, clinical manifestations will depend on cyst location and size; spinal cysts may cause local compression symptoms appearing as radiculopathy or myelopathy.3 In contrast, headache, and especially paroxysmal exercise-related headache, would be a very rare symptom.
We present the case of a 39-year old man with a history of episodes of lower back pain with no sciatica which had progressed for several years. He visited our department due to a 5-month history of headaches when bending down or performing Valsalva manoeuvres. The patient defines his pain as oppressive and acute; it starts in the occipital region and irradiates to the vertex before remitting with rest after a few minutes. He presented no nausea, vomiting, or visual disturbances. General and neurological examinations yielded normal results.
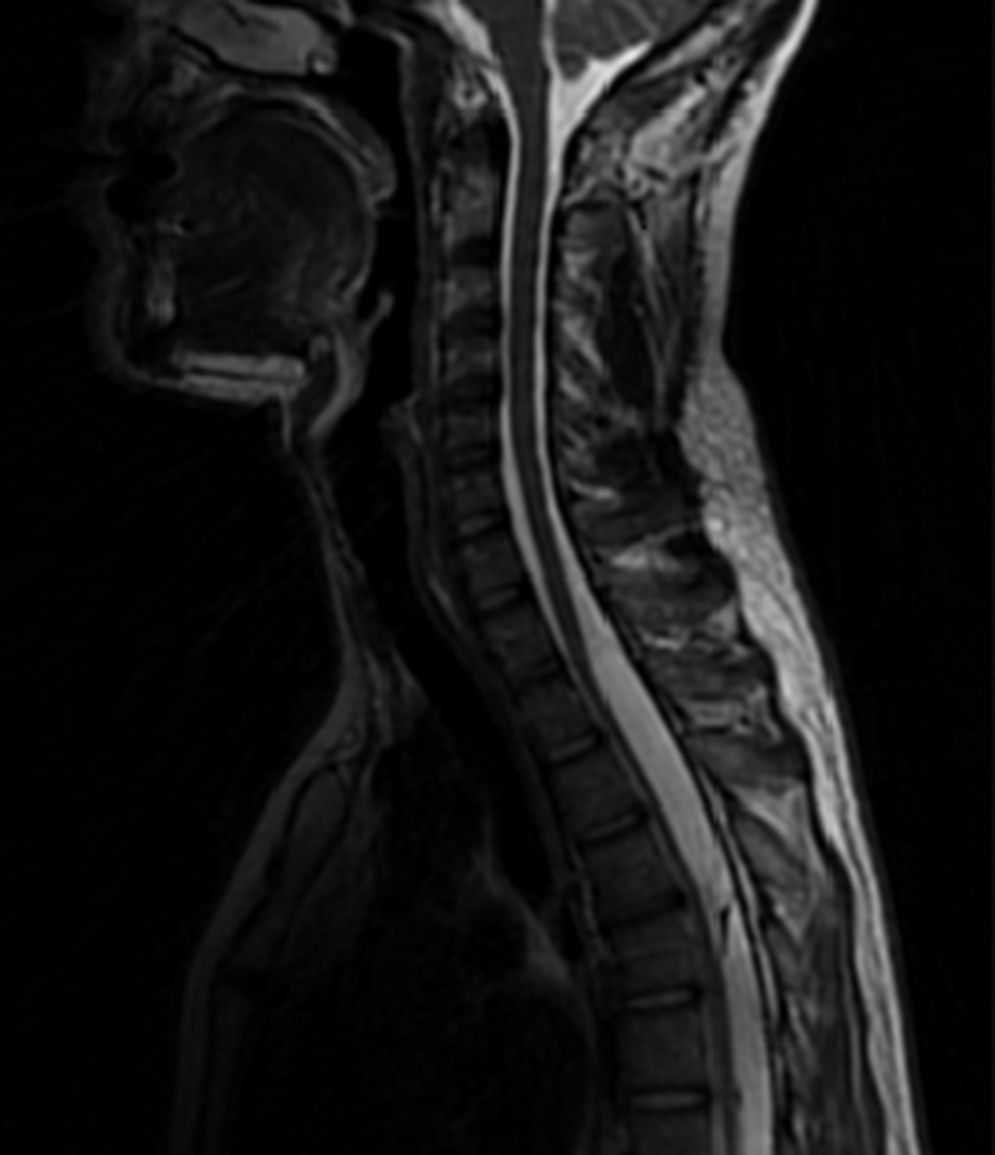
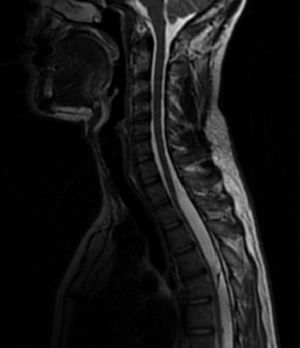
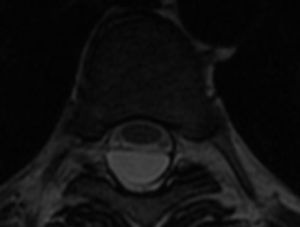
We performed a brain MRI with and without contrast and an MR angiography which ruled out space-occupying lesions, alterations in the occipitocervical junction, venous sinus thrombosis, or pathological contrast enhancement. A lumbar puncture revealed clear acellular CSF with an opening pressure of 15cm of water, normal glucose levels, and high protein levels (81mg/dL). Spinal MRI revealed liquid collections suggesting arachnoid cysts. They were intradural from T1-T2 level to T9 level (Fig. 1) and extradural (Fig. 2) from T11 level to L5 level, causing anterior displacement of the spinal cord and the roots of the cauda equina; no contrast enhancement was observed. The patient refused surgical treatment.
Published cases of paroxysmal headache triggered by Valsalva manoeuvres or certain body postures and secondary to spinal arachnoid cysts are exceptional, but such headaches have been shown to be due to transient rises in intracranial pressure.4 The spinal subarachnoid space's ability to expand, the compression of the cerebrospinal venous system, and CSF flow between the intracranial and spinal compartments are essential for protecting the brain from transient rises in intracranial pressure (ICP). Pressure spikes in the abdominal or thoracic cavity are transmitted to the epidural spinal venous plexus, resulting in increased volume in the intraspinal vascular compartment.5 This is immediately compensated by the distensibility of the subarachnoid space, therefore avoiding increases in ICP. Large spinal arachnoid cysts behave like space-occupying lesions and alter CSF flow dynamics, therefore preventing the expansion of the subarachnoid space. This space acts as an elastic reservoir which compensates for the physiological variations in intracranial pressure.6
Rupture of a spinal arachnoid cyst has been reported as a cause of CSF hypotension-hypovolaemia7,8 and there are published cases of exercise headache without any clear orthostatic component as the main manifestation of such ruptures.9 Spinal MRI studies in patients with CSF hypotension frequently reveal dilated venous plexi and liquid accumulating in the epidural space.10 In our case, CSF opening pressure was normal, brain MRI did not show meningeal enhancement, herniation of the cerebellar tonsils, or obliteration of prepontine or perichiasmatic cisterns, all of which are indirect signs of intracranial hypotension. Therefore, hypotension was not likely to be the cause of the headache.
In cases of exercise-induced headache, a brain MRI should always be performed to rule out focal lesions, occipitocervical junction malformations, or signs suggesting CSF hypovolaemia. In selected cases and depending on the clinical symptoms and results from complementary tests, a spinal MRI may be recommended.
FundingThis study has received no funding of any kind.
Please cite this article as: Arenaza Basterrechea N, Macarrón Vicente JL, Aícua Rapún I, Porqueres Bosch E. Quistes aracnoideos espinales, una causa inusual de cefalea de esfuerzo. Neurología. 2016;31:579–580.
Presented in poster format in the headache section at the 65th Annual Meeting of the Spanish Society of Neurology.