Recent studies have reported an increasing incidence of ischaemic stroke among young adults. However, the strength of the association between traditional vascular risk factors has not been fully established.
MethodsWe compared 120 patients with a first ischaemic stroke before the age of 55 years admitted to the stroke unit of our centre with 600 healthy non-stroke controls from a population-based cohort study (HERMEX), matched for sex. Risk factors assessed included: hypertension, obesity, auricular fibrillation, current smoking, estimated glomerular filtration rate (eGFR), total cholesterol, low-density lipoprotein cholesterol (LDL-C), triglycerides, high-density lipoprotein cholesterol (HDL-C) and diabetes mellitus. We used logistic regression analysis and calculated population attributable risk. We performed an overall analysis, by sex and aetiological subgroup.
ResultsUsing logistic regression analysis, we found that overall, the significant risk factors were: hypertension (OR: 1.58; 95%CI: 1.01-2.50), atrial fibrillation (OR: 4.77; 95%CI: 1.20-19.00), low eGFR (OR: 4.74; 95%CI: 1.3-21.94) and low HDL-C (OR: 5.20; 95%CI: 3.29-8.21), as well as smoking for males (OR: 1.86; 95%CI: 1.14-3.03). LDL-C showed an inverse association with stroke. The population attributable risk for HDL-C was 37.8% and for hypertension 21.1%. In terms of aetiological subgroups, only low HDL-C was associated with stroke of undetermined aetiology.
ConclusionsHypertension, auricular fibrillation, low eGFR, and low HDL-C, plus tobacco use in men, are the main risk factors among patients under 55 years of age with a first ischaemic stroke. We believe that it would be of particular interest to further explore the management of low HDL-C levels as part of preventive strategies in young stroke patients.
Estudios recientes han informado una incidencia creciente del ictus isquémico entre adultos jóvenes. Sin embargo, la fuerza de la asociación entre los factores de riesgo vascular tradicionales no se ha establecido por completo.
MétodosComparamos a 120 pacientes con un primer ictus isquémico antes de los 55 años ingresados en la unidad de ictus de nuestro centro con 600 controles sanos sin ictus de un estudio de cohorte basado en la población (HERMEX), con emparejamiento según el sexo. Los factores de riesgo evaluados incluyeron: hipertensión, obesidad, fibrilación auricular, tabaquismo actual, tasa de filtración glomerular estimada (eGFR), colesterol total, colesterol de lipoproteínas de baja densidad (LDL-C), triglicéridos, colesterol de lipoproteínas de alta densidad (HDL-C) y diabetes mellitus. Utilizamos un análisis de regresión logística y calculamos el riesgo atribuible a la población. Realizamos un análisis global, por sexo y subgrupo etiológico.
ResultadosMediante análisis de regresión logística comprobamos que globalmente los factores de riesgo significativos fueron: hipertensión (OR: 1,58; IC 95%: 1,01-2,50), la fibrilación auricular (OR: 4,77; IC 95%: 1,20-19,00), una eGFR baja (OR: 4,74; IC 95%: 1,3-21,94) y un HDL-C bajo (OR: 5,20; IC 95%: 3,29-8,21), así como el consumo de tabaco para los varones (OR: 1,86; IC 95%: 1,14-3,03). El LDL-C mostró una asociación inversa con el ictus. El riesgo atribuible a la población para el HDL-C fue del 37,8% y para la hipertensión del 21,1%. En cuanto a los subgrupos etiológicos, destaca que tan solo el HDL-C bajo se relaciona con el ictus de etiología indeterminada.
ConclusionesLa hipertensión, la fibrilación auricular, una eGFR baja y un HDL-C bajo, añadiendo el consumo de tabaco en varones, son los principales factores de riesgo entre los pacientes menores de 55 años con un primer ictus isquémico. Especial interés creemos que puede tener profundizar en el manejo de los niveles bajos de HDL-C dentro de las estrategias preventivas en pacientes jóvenes con ictus.
Ischaemic stroke is much rarer in young adults than in older patients, although the underlying pathologies and risk factors are more diverse.1 For this reason, the challenge in the diagnosis of cerebrovascular disease in young adults may be in differentiating it from stroke mimics and identifying the underlying cause or pathogenesis.2
Recent epidemiological studies suggest a significant upward trend in the incidence of ischaemic stroke in young adults.3,4 In current series, approximately 10%-20% of all strokes occur in patients aged between 18 and 50 years.5
Traditional stroke risk factors, which are frequent among older adults (hypertension, dyslipidaemia, diabetes mellitus, smoking, and obesity), have been shown also to be common among younger patients with a first stroke.6,7
In these young patients with stroke, who seem to present a growing prevalence of traditional vascular risk factors,8 it is debated whether these factors contribute to the cause of stroke and to what extent, especially in patients younger than 55 years.8 However, there are also young patients presenting no classical risk factors, who may present other conditions with a weak or uncertain association with stroke. These diseases frequently represent a risk factor that may be strictly specific to young age.9
Their aetiological heterogeneity and the increased complexity of their classification suggest that the high prevalence of risk factors in young adults with ischaemic stroke does not translate into a high frequency of patients classified with typical causes of early-onset stroke.10
Differences are reported in the population attributable risk (PAR) of classical risk factors between young men and women with stroke; hypertension, diabetes, smoking, and alcohol consumption seem to be more prevalent in men, and sedentary lifestyle and obesity are more prevalent in women.11
The aim of this study was to determine the strength of association between 10 vascular risk factors and ischaemic stroke in young adults, stratifying the analysis by sex and the main stroke aetiologies.
MethodsWe compared patients with a first ischaemic stroke before the age of 55 against a randomly selected sample of stroke-free controls or subjects with a symptomatic vascular disease from a population cohort study (Harmonizing Equations of Risk in Mediterranean Countries – Extremadura [HERMEX]).12 This study was performed at the neurology department of Hospital Universitario de Badajoz and was approved by the hospital’s ethics committee.
Population of casesThe stroke registry includes all patients younger than 55 years who were consecutively admitted in the last 2 years to our hospital’s stroke unit with a diagnosis at discharge of first ischaemic stroke. Data on stroke risk factors were obtained from medical records and laboratory tests. Stroke subtypes were classified according to the modified criteria of the Trial of ORG 10172 in Acute Stroke Treatment (TOAST) study13: 1) large-artery atherosclerosis, 2) cardioembolism, 3) small-vessel occlusion, and 4) stroke of undetermined aetiology. Strokes meeting criteria for stroke of undetermined aetiology due to mixed causes, with one of these being a high-risk cardioembolic source, were classified as cardioembolic; and cases with other determined aetiology were classified as stroke of undetermined aetiology. All patients had undergone an exhaustive aetiological study, and a brain MRI study was performed during hospitalisation in all cases.
Informed consent was not necessary in this study, as it was based on hospital records.
Control populationThe HERMEX project emerged from the need to generate information on the prevalence of risk factors and the frequency of cardiovascular disease onset in the population of Extremadura.12 From a cohort of 2833 individuals aged between 25 and 79 years, we selected a random sample of 600 individuals aged between 25 and 55 years. Information on each individual was collected in an interview on their history of cardiovascular risk factors, pharmacological treatments received, and symptoms and history of cardiovascular disease, similarly to the methods of the MONICA project coordinated by the World Health Organization (WHO).14
We examined 10 well-established vascular risk factors, from which we extracted comparable variables: arterial hypertension, obesity, dyslipidaemia, diabetes, atrial fibrillation (AF), current smoking habit, estimated glomerular filtration rate (eGFR), high low-density lipoprotein cholesterol (LDL-C) level, low high-density lipoprotein cholesterol (HDL-C) level, and high triglyceride (TG) level.
Definition of risk factorsHypertension was defined as treatment with antihypertensive drugs, previous diagnosis of hypertension, or diagnosis according to the 2003 WHO criteria (systolic arterial pressure ≥ 140 mm Hg or diastolic arterial pressure ≥ 90 mm Hg). Atrial fibrillation (AF) was defined as a diagnosis of AF or atrial flutter. Obesity was defined as a body mass index (BMI) ≥ 30, both in cases and in controls. In cases, current smoking was defined as smoking ≥ 1 cigarettes per day during the year prior to the stroke. Controls who currently smoked or had stopped smoking less than one year before inclusion in the HERMEX study were considered smokers. Diabetes mellitus in cases was defined as treated diabetes or history of diabetes before the stroke, with fasting plasma glucose levels ≥ 7 mmol/L (126 mg/dL) or a 2-hour oral glucose tolerance test results of ≥ 11.1 mmol/L (200 mg/dL), according to the data available in the medical records. In controls, diabetes was established in case of self-reported diagnosis in the questionnaire, diagnosis of diabetes in participants’ medical records, or prescribed medication for diabetes due to a fasting plasma glucose level ≥ 7 mmol/L (126 mg/dL) or glycated haemoglobin values > 6.5%. The eGFR was calculated using the Modification of Diet in Renal Disease formula, and was considered low for values < 60 mL/min/1.73m2. We defined the dichotomous variables of dyslipidaemia as high LDL-C (≥ 116 mg/dL), low HDL-C (< 39 mg/dL), and high triglyceride levels (≥ 177 mg/dL). An alternative dyslipidaemia variable was defined as treated dyslipidaemia, history of dyslipidaemia, or high total cholesterol level (≥ 193 mg/dL). To measure lipid levels in cases, fasting blood samples were collected on the first working day after the stroke and were analysed at the hospital laboratory. Among controls, fasting blood samples were collected in medical check-up visits. The LDL-C level was calculated using the Friedenwald equation in all cases. If this equation could not be used due to very high triglyceride levels, the binary variable LDL-C was recorded as high.
Statistical analysisStatistical analysis was conducted using SPSS version 22.0 for Mac. P-values < .05 were considered statistically significant.
First, we used the chi-square test and the Fisher exact test to compare groups. Prior to dichotomisation of the continuous variables (systolic and diastolic arterial pressure, LDL-C, HDL-C, TG, and eGFR), we confirmed that all these variables were normally distributed. To remove multicollinearity, we calculated variance inflation factors using a linear regression analysis and Cramer’s V statistic for measuring association.
We calculated the univariate odds ratio (OR) for the 10 dichotomous risk factors. Subsequently, we introduced place, age, and each risk factor in a multivariate binary logistic regression model, for which we calculated adjusted OR and 95% confidence intervals. We used a backward stepwise logistic regression analysis with a statistical significance level of P < .10.
We calculated PAR percentages from significant OR and 95% confidence interval values using the formula: prevalence of cases × [(OR – 1)/OR] × 100.
In addition to the analysis of the whole study population, we conducted an analysis by sex and aetiology. In the analysis by specific aetiology, the whole control group was used as controls.
ResultsWe selected 159 patients from the stroke registry, and excluded 32 cases of haemorrhagic strokes, 6 cases of stroke mimics, and one patient who was younger than 25 years, as no control was available. Therefore, the study population in the univariate analysis included 120 cases aged between 26 and 54 years (34 women and 86 men) and 600 controls (170 women and 430 men); the case:control ratio for both sexes was 1:5. The mean age of cases was 46.8 (SD: 7.0) years, and controls were younger (42.4 [7.9]). Cases presented a mean of 1.8 (1.5) risk factors, whereas controls presented a mean of 1.4 (1.2); this was a significant difference (P = .017).
In the study population, the risk factors analysed were more prevalent among cases than in controls, with the exception of dyslipidaemia, obesity, and high LDL-C level. In the multivariate logistic regression analysis, the risk factors with significant strength of association were low eGFR, AF, low HDL-C level, and hypertension. High LDL-C level and obesity were inversely associated with ischaemic stroke (Table 1).
Univariate and multivariate logistic regression analysis of risk factors for ischaemic stroke in young patients.
| Patients | Controls | Unadjusted | Adjusted* | ||
|---|---|---|---|---|---|
| N = 120; n/N (%) | N = 600; n/N (%) | OR (95% CI) | OR (95% CI) | PAR (95% CI) | |
| Hypertension | 44/120 (36.7) | 118/600 (19.7) | 2.36 (1.55-3.61) | 1.58 (1.01-2.50) | 21.1 (10.3-32.0) |
| Obesity | 25/120 (20.8) | 182/600 (30.3) | 0.60 (0.38-0.97) | 0.53 (0.33-0.86) | –12.0 (–20.4 to 1.5) |
| Dyslipidaemia | 26/120 (21.7) | 162/600 (27.0) | 0.75 (0.47-1.20) | 0.56 (0.37-0.96) | –6.8 (–15.7 to 4.2) |
| Diabetes mellitus | 16/120 (13.3) | 34/600 (5.7) | 2.56 (1.36-4.81) | 1.76 (0.92-3.39) | 8.1 (1.4-14.8) |
| Tobacco use | 60/120 (50.0) | 265/600 (44.2) | 1.26 (0.85-1.87) | 1.38 (0.91-2.07) | 10.4 (–6.7 to 27.7) |
| Atrial fibrillation | 5/120 (4.2) | 4/596 (0.7) | 6.48 (1.71-24.50) | 4.77 (1.20-19.00) | 4 (0.6-14.8) |
| eGFR (< 60) | 4/120 (3.3) | 3/600 (0.5) | 6.86 (1.51-31.07) | 4.74 (1.3-21.94) | 2.8 (–1.8 to 7.4) |
| High LDL-C level | 43/120 (35.8) | 382/599 (63.8) | 0.31 (0.21-0.48) | 0.23 (0.15-0.36) | –43.5 (–51.8 to –31.9) |
| Low HDL-C level | 49/120 (40.8) | 69/599 (11.5) | 5.30 (3.41-8.25) | 5.20 (3.29-8.21) | 37.8 (23.5-52.2) |
| High TG level | 30/120 (25.0) | 94/600 (15.7) | 1.79 (1.12-2.86) | 1.55 (0.96-2.51) | 3.1 (–8.9 to 15.2) |
Adjustment for age and each risk factor was necessary for inclusion in the multivariate model. 95% CI: 95% confidence interval; eGFR: estimated glomerular filtration rate; HDL-C: high-density lipoprotein cholesterol; LDL-C: low-density lipoprotein cholesterol; n/N: number of subjects divided by the total number of subjects; OR: odds ratio; PAR: percentage of population-attributable risk; TG: triglycerides.
Regarding the risks attributable to the whole young population with stroke, we found higher percentages of attributable risk for low HDL-C level, followed by hypertension, smoking, diabetes, and AF, which together would explain more than 70% of all strokes (Table 1; Fig. 1).
In the sex-specific analysis (Table 2), hypertension, diabetes, and low HDL-C level were significantly associated with ischaemic stroke in both sexes. However, smoking, high TG levels, and AF were only identified as significant risk factors in men. Obesity and high LDL-C levels were inversely associated with stroke in men, with no such association in women.
Univariate and multivariate logistic regression analysis of risk factors of ischaemic stroke in young patients, stratified by sex.
| Men | Patients | Controls | Unadjusted | Adjusted* |
|---|---|---|---|---|
| N = 86; n/N (%) | N = 430; n/N (%) | OR (95% CI) | OR (95% CI) | |
| Hypertension | 31/86 (36.0) | 95/430 (22.1) | 1.98 (1.21-3.26) | 1.15 (0.67-1.96) |
| Obesity | 17/86 (19.8) | 140/430 (32.6) | 0.51 (0.29-0.90) | 0.43 (0.24-0.78) |
| Dyslipidaemia | 23/86 (26.7) | 131/430 (30.5) | 0.83 (0.49-1.40) | 0.65 (0.38-1.12) |
| Diabetes mellitus | 12/86 (14.0) | 28/430 (6.5) | 2.32 (1.13-4.78) | 1.35 (0.64-2.88) |
| Tobacco use | 51/86 (59.3) | 196/430 (47.9) | 1.74 (1.09-2.78) | 1.86 (1.14-3.03) |
| Atrial fibrillation | 4/86 (4.7) | 3/430 (0.7) | 6.94 (1.52-31.60) | 5.63 (1.20-28.37) |
| eGFR (< 60) | 2/86 (2.3) | 2/430 (0.5) | 5.09 (0.71-36.68) | 3.43 (0.45-25.71) |
| High LDL-C level | 28/86 (32.6) | 284/429 (66.2) | 0.24 (0.15-0.40) | 0.18 (0.11-0.31) |
| Low HDL-C level | 45/86 (52.3) | 64/429 (14.9) | 6.26 (3.80-10.32) | 6.32 (3.73-10.70) |
| High TG level | 26/86 (30.2) | 85/430 (19.8) | 1.76 (1.05-2.95) | 1.45 (0.85-2.49) |
| Women | N = 34; n/N (%) | N = 170; n/N (%) | ||
| Hypertension | 13/34 (38.2) | 23/170 (13.5) | 3.96 (1.74-8.98) | 3.79 (1.58-9.10) |
| Obesity | 8/34 (23.5) | 42/170 (24.7) | 0.94 (0.40-2.23) | 0.87 (0.37-2.10) |
| Dyslipidaemia | 3/34 (8.8) | 31/170 (18.2) | 0.43 (0.12-1.51) | 0.37 (0.10-1.32) |
| Diabetes mellitus | 4/34 (11.8) | 6/170 (3.5) | 3.64 (1.00-13.70) | 3.46 (0.91-13.16) |
| Tobacco use | 9/34 (26.5) | 69/170 (40.6) | 0.53 (0.23-1.20) | 0.56 (0.24-1.29) |
| Atrial fibrillation | 1/34 (2.9) | 1/170 (0.6) | 5.12 (0.31-83.95) | 3.88 (0.23-66.03) |
| eGFR (< 60) | 2/34 (5.9) | 1/170 (0.6) | 10.56 (0.93-110.9) | 8.93 (0.77-103.52) |
| High LDL-C level | 15/34 (44.1) | 98/170 (57.6) | 0.58 (0.28-1.22) | 0.46 (0.21-1.01) |
| Low HDL-C level | 4/34 (11.8) | 5/170 (2.9) | 4.40 (1.12-17.34) | 4.04 (1.01-16.10) |
| High TG level | 4/34 (11.8) | 9/170 (5.3) | 2.40 (0.70-8.25) | 2.24 (0.64-7.79) |
Adjustment for age and each risk factor was necessary for inclusion in the multivariate model. 95% CI: 95% confidence interval; eGFR: estimated glomerular filtration rate; HDL-C: high-density lipoprotein cholesterol; LDL-C: low-density lipoprotein cholesterol; n/N: number of subjects divided by the total number of subjects; OR: odds ratio; TG: triglycerides.
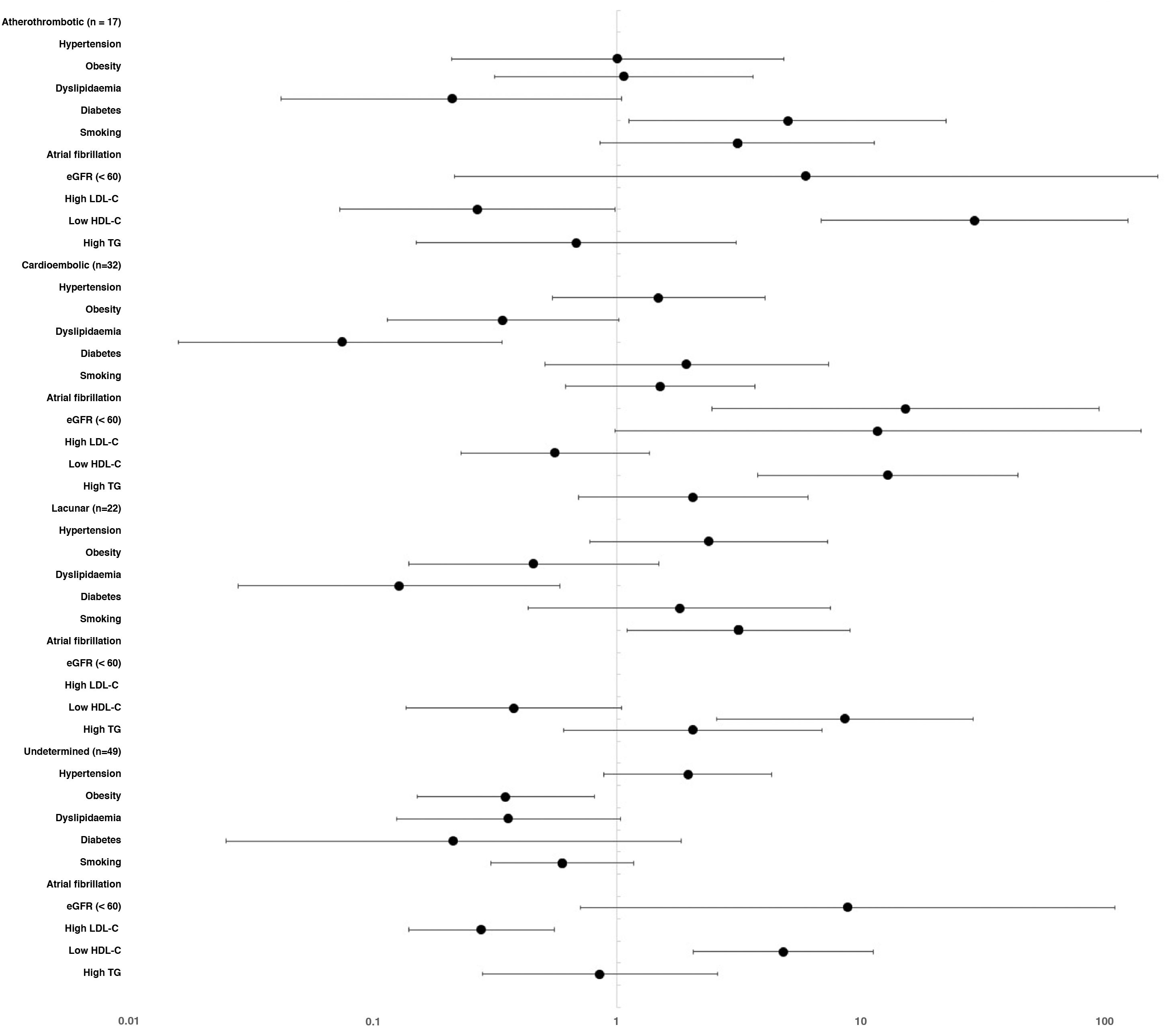
In the analysis by aetiological subtype (Table 3), large artery atherosclerosis showed significant associations with hypertension, smoking, diabetes, low eGFR, and low HDL-C level. Cardioembolic aetiology was significantly associated with AF, hypertension, diabetes, low eGFR, low HDL-C level, and high TG level. For small-vessel disease, hypertension, smoking, diabetes, low HDL-C level, and high TG level were identified as risk factors. Only low HDL-C level showed a significant association as a risk factor in stroke of undetermined aetiology. In these 4 aetiological groups, high LDL-C level was inversely associated with stroke, although this association was not significant in the case of cardioembolic stroke. Due to the absence of cases with a positive risk factor, AF could not be analysed in subgroups other than the cardioembolic stroke group, and eGFR could not be analysed in the subgroup of lacunar infarcts (Fig. 2).
Prevalence of risk factors per aetiological group.
| Atherothrombotic | Cardioembolic | Lacunar | Undetermined | Controls | |
|---|---|---|---|---|---|
| N = 17; n/N (%) | N = 32; n/N (%) | N = 22; n/N (%) | N = 49; n/N (%) | N = 600; n/N (%) | |
| Age in years, mean (SD) | 48.5 (6.3) | 49.7 (4.8) | 46.6 (7.5) | 44.5 (7.7) | 42.4 (7.9) |
| Sex (women) | 1 (0.6) | 8/32 (25.0) | 3/22 (13.6) | 22/49 (44.9) | 170/600 (28.3) |
| Hypertension | 7/17 (41.2) | 14/32 (43.8) | 9/22 (40.9) | 14/49 (28.6) | 118/600 (19.7) |
| Obesity | 6/17 (35.3) | 6/32 (18.8) | 4/22 (18.2) | 9/49 (18.4) | 182/600 (30.3) |
| Dyslipidaemia | 7/17 (41.2) | 6/32 (18.8) | 5/22 (22.7) | 8/49 (16.3) | 162/600 (27.0) |
| Diabetes mellitus | 6/17 (35.3) | 5/32 (15.6) | 4/22 (18.2) | 1/49 (2.0) | 34/600 (5.7) |
| Tobacco use | 12/17 (70.6) | 16/32 (50.0) | 16/22 (72.7) | 16/49 (32.7) | 265/600 (44.2) |
| Atrial fibrillation | 0/17 (0.0) | 5/32 (15.6) | 0/22 (0.0) | 0/49 (0.0) | 4/596 (0.7) |
| eGFR (< 60) | 1/17 (5.9) | 2/32 (6.3) | 0/22 (0.0) | 1/49 (2.0) | 3/600 (0.5) |
| High LDL-C level | 4/17 (23.5) | 15/32 (46.9) | 8/22 (36.4) | 16/49 (32.7) | 382/599 (63.8) |
| Low HDL-C level | 12/17 (70.6) | 13/32 (40.6) | 10/22 (45.5) | 14/49 (28.6) | 69/599 (11.5) |
| High TG level | 5/17 (29.4) | 11/32 (34.4) | 8/22 (36.4) | 6/49 (12.2) | 94/600 (15.7) |
eGFR: estimated glomerular filtration rate; HDL-C: high-density lipoprotein cholesterol; LDL-C: low-density lipoprotein cholesterol; n/N: number of subjects divided by the total number of subjects; SD: standard deviation; TG: triglycerides.
Multivariate logistic regression analysis of risk factors of early-onset ischaemic stroke, stratified by aetiology (odds ratio and 95% CI).
Adjusted for age and each risk factor included in the study. eGFR: estimated glomerular filtration rate; HDL-C: high-density lipoprotein cholesterol; LDL-C: low-density lipoprotein cholesterol; TG: triglycerides.
Our study shows a strong association between stroke in young patients and hypertension, AF, low eGFR, and low HDL-C level, as well as smoking among men. Furthermore, we found differences in the risk profiles between aetiological subgroups. Interestingly, stroke of undetermined aetiology, the most prevalent subtype, was not significantly associated with any of these classical risk factors except for low HDL-C level; therefore, we should insist on the search for new risk factors that might help us to explain this type of stroke and design new prevention strategies.
Whereas the prevalence of certain risk factors has been decreasing in the general population, the prevalence of modifiable vascular risk factors (hypertension, smoking, or diabetes) is increasing among younger patients with stroke.6,9,15
Some studies show that young patients with stroke present approximately twice as many risk factors as their peers in the general population.8 If the risk of cerebrovascular events increases in association with the number of risk factors, this may explain the observed increase in stroke prevalence4; however, this is still to be clarified.16
The data collected in large cohort studies that have reported on risk factors from a global perspective show that a small subset of risk factors explain a large proportion of strokes internationally.17 We do not know whether these findings are applicable to young patients with stroke, as the analysis was not stratified by age. The INTERSTROKE study, in which only 11.8% of patients were younger than 45 years, only showed differences between patients younger and older than 55 years in some risk factors.18 To date, few studies have analysed the strength of association between stroke in young patients and vascular risk factors.8,11,19
HypertensionIn our study, 36.7% of cases presented hypertension, a rate similar to the prevalence rates published by other studies.11,15,20 The Stroke in Young Fabry Patients (SIFAP) study showed that hypertension was the most important individual risk factor for ischaemic stroke, with a PAR of 25.5%, showing a significant association with stroke in young adults (OR: 2.3; 95% CI: 2.0-2.6)21; these data are similar to ours. A recent Finnish study detected somewhat smaller differences (PAR of 12.2% and OR of 1.43 [95% CI: 1.71-1.75]).19
ObesityObesity is an independent vascular risk factor for stroke.22,23 Obesity, defined as a body mass index higher than 30, has been observed in more than 10% of young adults who present stroke.24 We detected a higher percentage in our study (20.8%), but did not observe a positive association with stroke. The SIFAP study found that abdominal obesity was one of the main risk factors in women with stroke.21 The study by Aigner et al.11 showed that obesity in young adults was associated with greater risk of stroke, with a PAR of 6.9% (OR: 1.2% 95% CI: 1.5-2.3).11
DyslipidaemiaSome studies report a prevalence of approximately 50% of dyslipidaemia in young patients with stroke, with higher rates in men than in women.1,20 In our study, we did not find a significant association between dyslipidaemia and stroke, even in the analysis by sex. We even found a clear inverse association between stroke and LDL-C level, which has also been observed in other studies.19
This may be explained by the aetiological heterogeneity of stroke: in some aetiologies, dyslipidaemia may not be a risk factor, with the exception of stroke due to atherosclerosis or small-vessel disease. The subgroup analysis shows a higher prevalence of dyslipidaemia in the atherothrombotic stroke group than among controls (41.2% vs 27%). This has also been observed by other researchers.8,11
Another explanation for why dyslipidaemia may not significantly contribute to the risk of ischaemic stroke in young adults may be that the majority of studies defined dyslipidaemia as a high LDL-C or low HDL-C level, but did not analyse the association between different lipid variables and stroke, which may be of clinical interest. For example, a Brazilian study revealed that the apolipoprotein B/apolipoprotein A-I ratio was strongly associated with ischaemic stroke (OR: 4.03; 95% CI: 1.62-10.03).25
We assessed additional lipid variables in our study. We found a clear and consistent association between low HDL-C level and stroke, both in the overall analysis and in the analysis by sex and stroke subtype. This has also been observed by other authors.19,26,27 Experimental, epidemiological, genetic, and clinical studies suggest an independent inverse correlation between HDL-C levels and vascular disease.28 Low HDL-C levels are the most prevalent lipid abnormality in patients with early atherosclerotic disease.29 Furthermore, studies performed in cell cultures and in animal models have shown that HDL-C particles exert a vasoprotective effect.30 In fact, the antiatherogenic effect of HDL-C seems to involve several mechanisms, including reverse cholesterol transport and cardiovascular, antioxidant, antiplatelet, anti-apoptotic, and anti-inflammatory protective action, which are not necessarily associated with cholesterol homeostasis.31 The discovery of new genes and pathways participating in HDL-C metabolism may lead us to place greater emphasis on the diagnosis and management of low HDL-C levels in prevention strategies for young patients with stroke.32
Furthermore, low HDL-C level is not only a good marker of vascular risk, but may also indicate poorer health status due to concomitant factors that have not been analysed in our study, such as sedentary lifestyle or lower socioeconomic status.33,34
High TG level is a risk factor frequently overlooked by neurologists, although the number of studies showing an association between high TG levels and stroke is increasing.35 Hypertriglyceridaemia may increase the risk of ischaemic stroke, as it predisposes patients to atherosclerosis, thrombosis, and hyperviscosity.36 In our study, this risk factor was more prevalent among cases and is non-independently associated with stroke and some aetiological subtypes.
DiabetesIn our study, diabetes acted as a global risk factor, for both sexes and for the atherosclerosis and small-vessel disease aetiological subgroups.
The studies performed to date have shown great variation in the strength of association between diabetes and stroke in young patients.37 According to some authors, diabetes is present in up to 10% of young patients with stroke15,16; our study found a prevalence of 13%. Recent studies report PAR values ranging between 4.8% and 6.5%,11,19 with our study showing 8.1%. Considering these data, we should be concerned by the increase in the incidence of diabetes type 2 in young adults, which contributes to the increase in the rate of stroke at earlier ages.16
Although there are no considerable differences between sexes in the prevalence of diabetes type 2,21 the risk of stroke, according to some studies, would be higher in women than in men (hazard ratio: 2.8 vs 2.2).38 In our study, we also observed that the strength of association of diabetes with stroke was stronger in women.
It is noteworthy that 2 of the most potent atherogenic components of diabetic dyslipidaemia are the increase in residual particles of TG and low HDL-C levels,39 which we also observed in our series (data not shown).
SmokingThe proportion of smokers among young patients with stroke is high, with recent studies reporting that up to 50% of these patients are smokers.8,10 Furthermore, during the last decade, the prevalence of smoking has increased among young adults.40 According to our study, smoking contributes to stroke in men, and was more frequently reported among patients with stroke of atherothrombotic or lacunar aetiology. Similar findings have been reported in other studies.18,40 Compared to adults older than 55 years, the dose-response relationship with stroke seems to be stronger at younger ages, both in men and in women.41
Glomerular filtration rateOur study shows that eGFR acts as a potent risk factor and is specifically associated with all aetiological subtypes, with the exception of stroke of undetermined cause. In individuals with a moderate decrease in eGFR (30-59), the risk of cardiovascular death is up to 3 times higher than in subjects with normal eGFR values.42 The applicable guidelines consider that all subjects with moderately decreased eGFR present a high risk of vascular disease, including stroke.43 Kidney function, as determined by the eGFR, shows an inverse association, with a clearly increasing risk of stroke as the kidney function worsens.44 Some authors have shown that proteinuria itself is a little-known risk factor for stroke, regardless of arterial pressure and diabetes; this, together with reduced kidney function, substantially increases the risk of stroke.45
LimitationsThe limitations of our study include the potential biases inherent to case-control studies. Although we made thorough efforts to homogenise risk factors, some residual bias may remain. The prevalence of AF and low eGFR in controls was low; consequently, the estimated OR for these infrequent risk factors should be interpreted with caution. Furthermore, these variables could not be analysed in all aetiological subgroups.
With regard to smoking, we could not analyse the dose-response relationship between smoking and stroke. We did not include any factor specifically related with risk among women, such as the use of contraception or migraine, or the risk inherent to childbearing age in women. With respect to the measurement of kidney function, subjects were classified according to a single eGFR determination, and although this is the typical practice in epidemiological studies, it is also known that calculations based on creatinine may present some limitations.
All models were adjusted for vascular risk factors, but not for use of statins, renin-angiotensin system inhibitors, or antiplatelet drugs. Neither did we include the progression time of risk factors, or other concomitant diseases, neoplasms, physical activity, socio-economic factors, or pollution, which have been also associated with cerebrovascular disease.
ConclusionsHypertension, AF, low eGFR, low HDL-C level, and smoking are the main risk factors for stroke among individuals younger than 55 years. We consider it particularly important to conduct further studies into the management of low HDL-C levels with a view to developing prevention strategies for young patients with stroke. We should also seek to improve kidney health through the development of awareness campaigns, health education, and renal insufficiency prevention campaigns, at least in specific risk groups. The considerable differences in the risk profile between aetiological subgroups corroborate the significant pathogenic complexity of early-onset stroke. We should continue in the search of new risk factors may that might explain this type of stroke and focus on new prevention strategies.