Fragile X-Tremor/Ataxia syndrome (FXTAS) is an adult-onset neurodegenerative disease caused by a premutation in the Fragile X mental retardation (FMR1) gene. For patients with limited daily-life activities due to medically intractable tremor, neurofunctional surgery approaches should be considered. Recent studies have demonstrated the effectiveness and safety of unilateral MRI-guided focused ultrasound (MRIgFUS) thalamotomy for Essential Tremor (ET)1 and tremor dominant Parkinson Disease (PD) patients.2 To date, scarce knowledge is available when it comes to FXTAS patients and MRIgFUS. So far, only 2 FXTAS cases treated with unilateral MRIgFUS thalamotomy have been published.3,4 Nevertheless, no long-term follow-up information is available.
Case reportHerein, we describe a 3-year follow-up of right VIM (Ventralis Intermediate Nucleus) MRIgFUS thalamotomy in a left-handed patient with a confirmed FMR1 mutation (86 repeats). Postural left-hand tremor initiated in the adult age and worsened progressively over the years. Neurological examination at baseline revealed severe rest, postural and intentional left-hand assessed by Essential Tremor Rating Scale Fahn-Tolosa Marin (ETRS). At that time, the patient was neither able to drink, eat nor write unaided. On basal evaluation, slight instability when performing tandem gait testing (BBS=54) was observed. The Berg Balance Score (BBS) is a 14-item objective measure that assesses static balance and fall risk in adults. A global score can be calculated out of 56; a higher score indicates better balance. Cerebral MRI showed moderate atrophy of the cerebellar parenchyma and loss of white matter intensity in dentate nuclei and middle cerebellar peduncles. Due to the outstanding limitation in daily-life activities, neurofunctional surgical treatments were offered. Patient decided for MRIgFUS thalamotomy based on the limited experience previously published. MRIgFUS thalamotomy was accepted as compassionate use treatment by health authorities. Informed consent was signed by the patient.
Regarding surgery, the VIM nucleus contralateral to the most disabled hand was indirectly targeted on a preoperative MRI scan. Targeting methods have been described elsewhere.5 Based on previous experience,6 our group adopted some procedural changes that included: (a) centering the lesion 2mm above the depth of the intercommisural line and (b) increasing the rate at which sonication power is raised over the course of the treatment.5 Final tremor arrest was accomplished with an average peak target temperature of 58°C reached after a total of 6 sonications. Only transient dizziness sensation was noticed during the procedure.
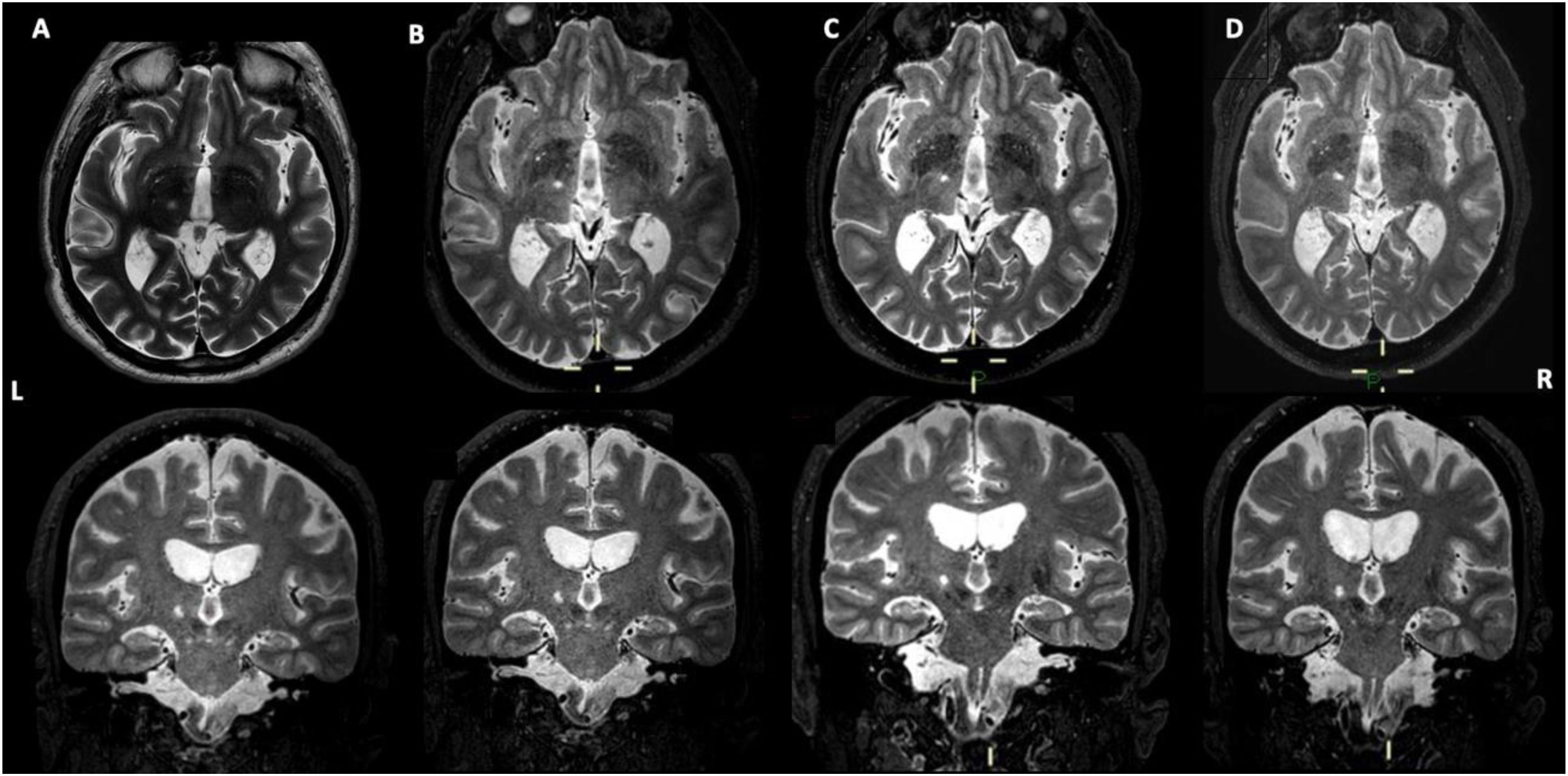
On the follow-up visits, remarkable improvement of the treated hand tremor score (subsection part A+B ETRS, range 0–32) was noticed at all visits: 88% at 1 month, 74% at 1 year and 60% at 3 years, when comparing with basal evaluation (25 points) as seen in Table 1. Disability scores (part C of ETRS, range 0–28) ameliorated. Other quality of life assessments also improved (QUEST and EQ-5D Questionnaires). To elucidate the natural evolution of balance after the procedure, gait function was specifically assessed with BBS (range 41–56 indicating independent walking). Although at 1 month, BBS score decreased 5 points (49 points) reflecting mild balance impairment, at 1 year balance recovered to basal situation (53 points). At 3 years BBS score was 50 points. Natural evolution of the lesion (including peripheral oedema and central necrosis) was also assessed by subsequent MRI timepoints controls (Fig. 1).
Since the introduction of MRIgFUS, many centres have successfully treated patients with medication-refractory tremor, mainly ET patients. However, no literature is available when it comes to MRIgFUS treated FXTAS patient series. It is well known that gait impairment is one of the most common complaint encountered during the first 3 months after surgery.7 Accordingly, in this case report, the decline noticed in BBS at the first month and its recovering at 1 year may probably be due to the perilesional oedema. However, the mild worsening of balance at 3 years follow-up points to the intrinsic progression of the disease.
ConclusionTo our knowledge this is the first long-term reported follow up of a FXTAS patient treated with unilateral MRIgFUS thalamotomy. Thus, it suggests acceptable safety and effectiveness of this technique when applied to FXTAS patients. Nevertheless, the own progression of this neurodegenerative condition may negatively impact the future outcome of MRIgFUS, consequently patients should be assessed and informed with caution. Equally, accurate surgical targeting and technique optimization are two critical aspects of this novel technique that should be addressed. The reduced number of sonications accomplished in this patient highlights this direction and may guarantee special safety when it comes to balance. Our experience points out that conducting standardized and homogeneous assessments that objectively measure balance status before surgery may help clinicians to identify patients who are at higher risk of developing unsteadiness. This approach may be relevant in certain conditions such as FXTAS.
Author roles- 1.
Research project: A Conception, B. Organization, C. Execution;
- 2.
Statistical analysis: A. Design, B. Execution, C Review and Critique;
- 3.
Manuscript preparation: A. Writing the first draft, B: Review and Critique.
MCR 1A, 1B, 1C, 2A, 2B, 3A
RCS 1A, 1B, 2C, 3B
JLLG 1A, 1B, 2C, 3B
ISB 1A, 1B, 1C, 2C, 3B
Ethical compliance statementThe authors confirm that the approval of an institutional review board was not required for this work. Written informed consent was obtained from the patient for publication of this case report and the accompanying images. We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this work is consistent with those guidelines.
Financial disclosures for the previous 12 monthsIMT has received honoraria from Palex for lecturing.
AML is a consultant for Insightec.
The rest of authors report no conflicts of interest and no sources of funding.
Declaration of generative AI and AI-assisted technologies in the writing processDuring the preparation of this work the author(s) did not use any writing aid tool. The author(s) reviewed and edited the content as needed, taking full responsibility for the content of the publication.
Funding sourcesThis research has not received specific support from public sector agencies, the commercial sector or non-profit entities.
Conflict of interestNo conflict of interest has been found in the preparation of this manuscript.
We thank the patient and his family for the patience and cooperation.