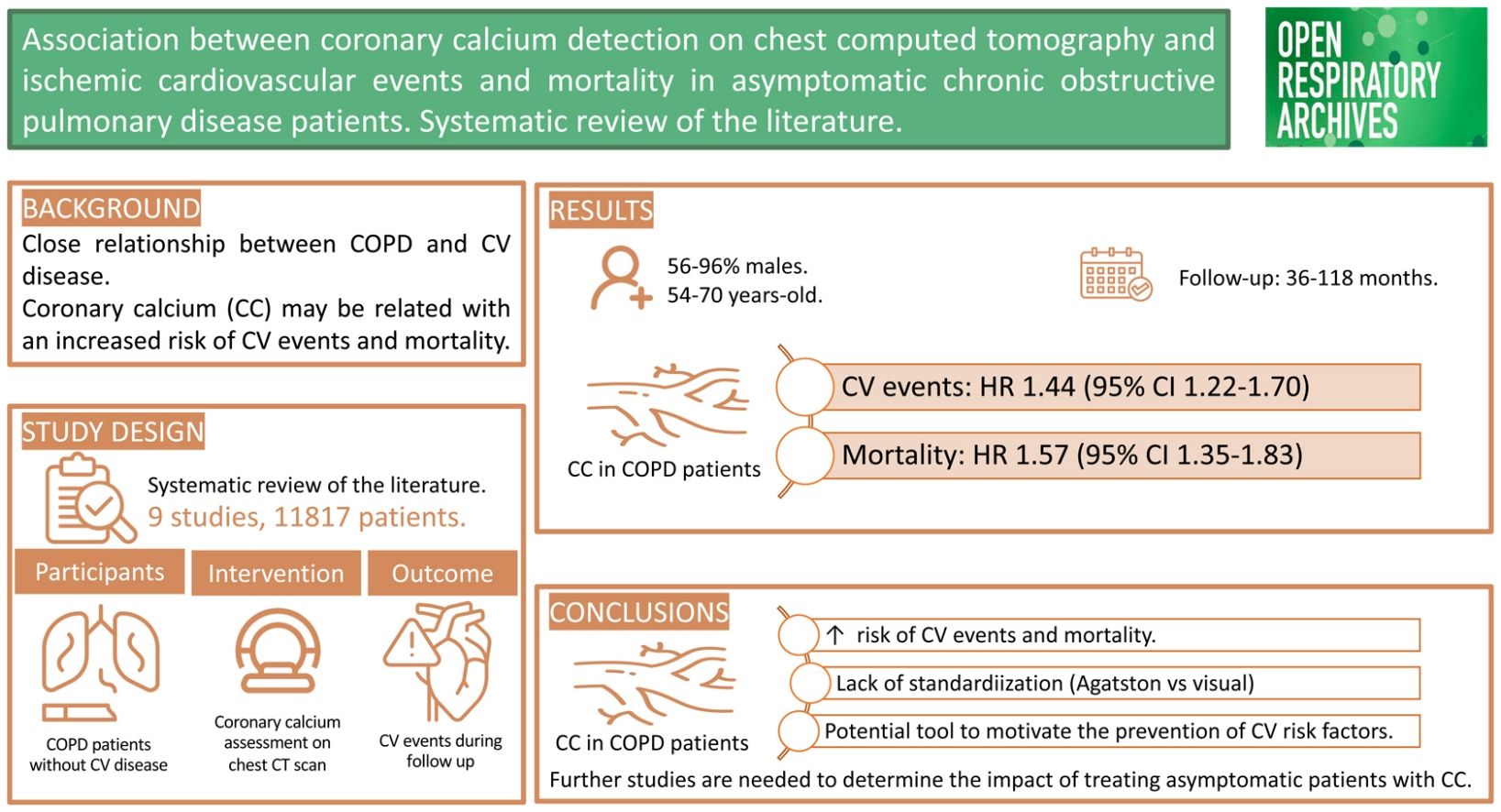
Literature suggests that there is a close relationship between chronic obstructive pulmonary disease (COPD) and cardiovascular (CV) disease. The aim of this study was to assess whether the presence of coronary calcium (CC) on chest computed tomography (CT) in asymptomatic COPD patients is associated with an increased risk of CV events and mortality.
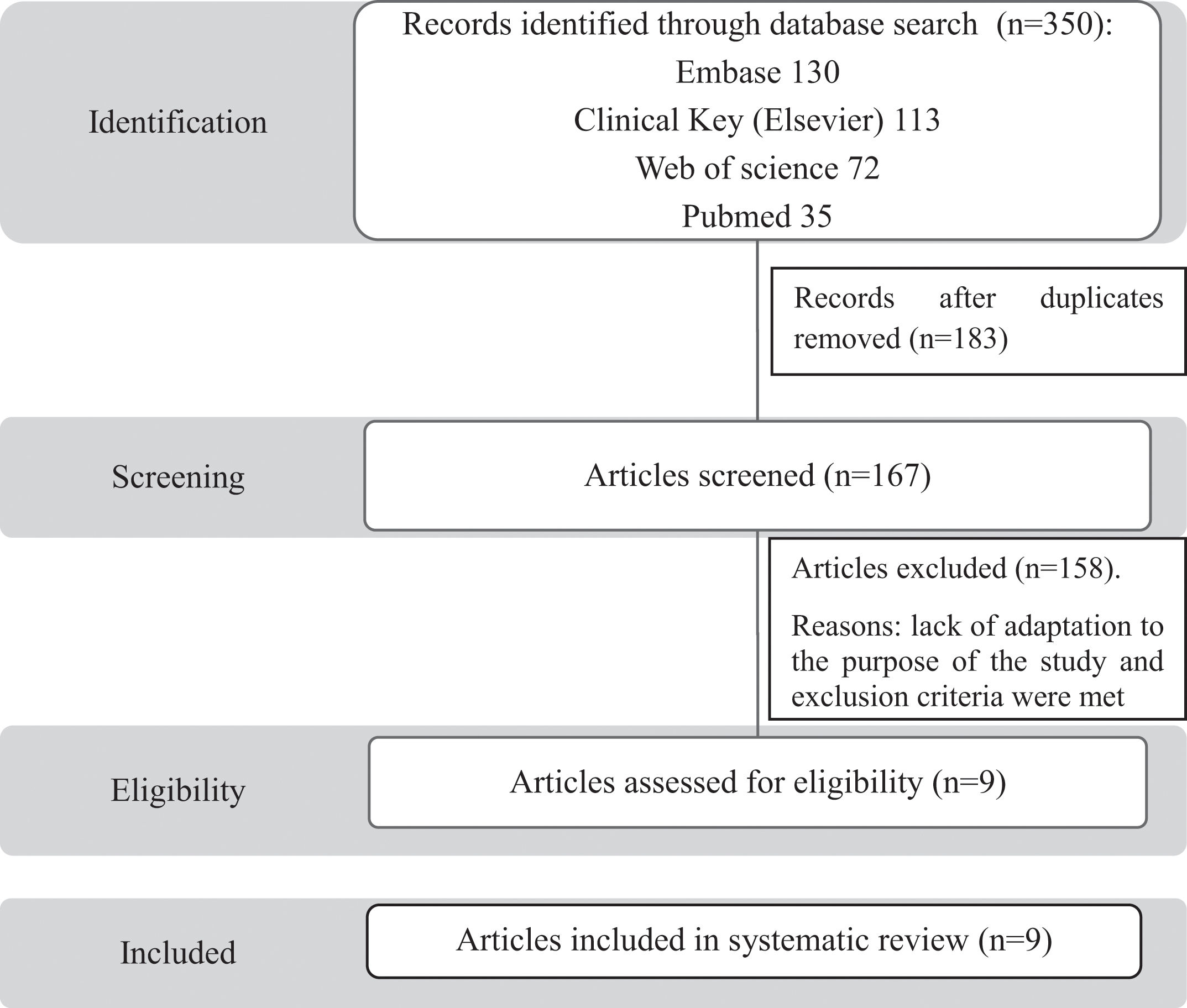
Material and methodsA systematic review of the literature was performed following PRISMA recommendations. Studies published in the last 20 years in four databases (PubMed, Web of Science, Embase and MEDLINE) were included.
ResultsThree hundred fifty articles were identified, eight of them met the selection criteria. The included studies, conducted between 2013 and 2024, were predominantly multicentre cohort studies. The meta-analysis showed that the presence of CC on chest CT of COPD patients is an independent predictor of CV events (hazard ratio 1.44, 95% CI 1.22–1.70) and associated with an increased mortality during the follow-up period (hazard ratio 1.57, 95% CI 1.35–1.83).
ConclusionsOur analysis suggests that the identification of CC on chest CT scans of COPD patients may be useful in the early detection and treatment of CV disease in asymptomatic patients. Prospective, multicentre studies confirming our findings are needed to explore the potential impact of early detection and treatment of CV risk in COPD patients.
La literatura sugiere que existe una estrecha relación entre la enfermedad pulmonar obstructiva crónica (EPOC) y la enfermedad cardiovascular (CV). El objetivo de este estudio fue evaluar si la presencia de calcio coronario (CC) en la tomografía computarizada (TC) torácica en pacientes asintomáticos con EPOC se asocia con un mayor riesgo de eventos CV y mortalidad CV.
Material y métodosSe realizó una revisión sistemática de la literatura siguiendo las recomendaciones PRISMA. Se incluyeron estudios publicados en los últimos 20 años en cuatro bases de datos (PubMed, Web of Science, Embase y MEDLINE).
ResultadosSe identificaron 350 artículos, ocho de los cuales cumplieron los criterios de inclusión. Los estudios fueron realizados entre 2013 y 2024, con un diseño de cohortes y de carácter multicéntricos. El metaanálisis concluyó que la presencia de CC en la TC torácica de pacientes con EPOC es un predictor independiente de eventos CV (hazard ratio: 1,44; IC 95%: 1,22-1,70), y se relacionó con un aumento de la mortalidad CV en el período de seguimiento (hazard ratio: 1,57; IC 95%: 1,35-1,83).
ConclusionesEl análisis sugiere que la identificación de CC en las TC torácicas de pacientes con EPOC puede ser útil en la detección precoz y en el tratamiento de la enfermedad CV en pacientes asintomáticos. Se necesitan estudios prospectivos multicéntricos que confirmen nuestros hallazgos para explorar el impacto potencial de la detección precoz y el tratamiento del riesgo CV en pacientes con EPOC.
Chronic obstructive pulmonary disease (COPD) is one of the leading causes of morbidity and mortality worldwide. Although the degree of airflow obstruction has traditionally been the way of assessing disease severity, there is a weak correlation between forced expiratory volume in the first second (FEV1), symptoms and health status. Since the publication of the BODE index1 (Body mass index, Obstruction, Dyspnoea, Exercise) in 2004, the disease is approached from a multidimensional perspective.
COPD is often associated with multiple comorbidities2,3: cardiovascular (CV) diseases (ischemic heart disease, arrhythmias, heart failure), metabolic/nutritional diseases (diabetes mellitus, dyslipidaemia, obesity, osteoporosis, sarcopenia), psychological disorders (anxiety, depression), lung cancer, respiratory sleep disorders and gastro-oesophageal reflux disease. However, COPD itself can mislead its identification and diagnosis, given the overlap of symptoms and the difficulty in performing certain diagnostic tests. Despite GOLD guidelines recommending its diagnosis and treatment, there is no consensus or guidance on an appropriate early detection approach for these comorbidities.3
CV diseases and COPD share similar risk factors, symptoms and pathogenic pathways, contributing to the high prevalence of CV disease in COPD patients.4 COPD patients are estimated to have a 2–5-fold increased risk of CV disease5 and their coexistence is associated with worse outcomes than either condition alone.6 Different pathophysiological mechanisms have been proposed to explain this association, such as chronic systemic inflammation, oxidative stress, hypoxia or hyperinflation.5 However, mechanisms are likely to be multifactorial and accurate risk prediction may require incorporating data from clinical phenotypes, blood and radiological biomarkers, genets and then demonstrating superiority to traditional risk prediction models.7
CV diseases are often under-diagnosed and under treated in patients with COPD.6 Especially, ischemic heart disease on which we will focus our analysis, may have an initial silent period. Early detection may help in a more aggressive management of CV risk factors than recommended by traditional CV risk scales. For early identification, several clinical and radiological markers of COPD have been described that appear to be related to CV disease. However, key international, regional and local guidelines provide limited recommendations on how manage patients with COPD and CV disease.5,6
Non-invasive markers of ischemic heart disease risk include coronary calcium (CC), which can be detected on chest computed tomography (CT) and quantified using the validated Agatston scale8 (Fig. 1) or visual estimation.9 Its measure allows an individualised assessment of risk,6 as the detection of CC is pathognomonic of subclinical coronary atherosclerosis and is widely used to identify and stratify the risk of CV disease.9 Although CC has been associated with an increase in CV disease in different studies,9–17 it remains a potentially useful and non-standardized tool in patients with COPD. It might be an interesting additional tool for the clinician and patient to motivate to initiate preventive interventions.18
The aim of the study was to conduct a systematic review of the available literature on the relationship between CC detection in COPD patients with the risk of ischemic CV events and mortality from this cause.
Material and methodsA comprehensive search for scientific evidence was conducted, focusing the clinical question on a PICO format (Patient, Intervention, Comparison, and Outcome).19
The systematic review of the literature protocol was designed following PRISMA principles.20 Bibliographic searches were performed on August 2024 across four databases (PubMed, Web of Science, Embase, MEDLINE), limiting the search to the last 20 years. The search strategy employed was [(“chronic obstructive pulmonary disease”) AND (“coronary artery calc*” OR “calcium score” or “calcium score test” OR “CST”) AND (“mortal*” OR “cardiovascular death” or “major cardiovascular event*”)] in the article title, abstract, and keywords (descriptors), with equivalent search fields in each consulted database. The review protocol was registered on PROSPERO.
The following types of articles were included: scientific articles and letters on the study's topic of interest. All other types of material were excluded: reviews, letters to the editor, comments, opinions, perspectives, guidelines, regulatory documents, opinion web pages, bibliographic selections, cases or case series, and congress or symposium abstracts or proceedings. Preprints or inaccessible full texts were excluded. Publication languages were limited to English or Spanish.
Articles were included if participants had a confirmed diagnosis of COPD based on the GOLD 20242 international diagnostic criteria. That is, patients with symptoms of the disease (chronic cough, phlegm, dyspnoea, wheezing and/or history of respiratory infections) with a post bronchodilator forced expiratory volume in the first second to forced vital capacity ratio (FEV1/FVC) less than 70% of predicted value, and a history of smoking (10-pack-year index). Comorbidities and CV risk factors were recorded according to the diagnostic criteria chosen in each study. Studies with patients presenting CV symptoms or previous history of revascularization were excluded. Regarding the intervention performed, studies were included if a chest CT and CC assessment (via automated or visual methods) had been conducted.
As outcomes, studies were included if they analysed mortality and major CV ischemic events associated with CC, defined as non-fatal stroke, angina, non-fatal myocardial infarction, and CV death.
PRISMA recommendations were followed for the systematic review process. The adaptation of selected articles to the study's purpose and inclusion criteria was conducted by both authors. The quality of studies included and evaluation risk of bias was assessed by two researchers using the Newcastle–Ottawa scale (NOS) (with a score ranging from 0 to 9 points), Table 1. Artificial intelligence was not used in the preparation of the review.21
Newcastle–Ottawa scale of studies included in the systematic review.
| First author | Selection | Comparability | Outcome | Total(max. 9 points) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Representiveness | Non exposed group | Ascertainment | Outcome of interest not present at start of study | Result not present at start of the study | Comparability for confounders | Assessment of outcome | Follow-up duration | Adequacy of follow-up | ||
| Bhatt et al.13 | * | * | * | * | * | * | * | * | * | 9 |
| Budoff et al.10 | * | * | * | * | * | * | * | 6 | ||
| Gaisl et al.14 | * | * | * | * | * | * | * | * | 8 | |
| O’Hare et al.11 | * | * | * | * | * | * | * | * | 8 | |
| Romme et al.12 | * | * | * | * | * | * | * | * | 8 | |
| Takei et al.16 | * | * | * | * | * | * | * | * | * | 9 |
| Williams et al.9 | * | * | * | * | * | * | * | * | 8 | |
| Yang et al.17 | * | * | * | * | * | * | * | * | * | 9 |
| Zagaceta et al.15 | * | * | * | * | * | * | * | * | * | 9 |
After the search for articles carried out in the different databases analysed, 350 studies met the selection criteria in accordance with the PRISMA statement. After removal of duplicate studies, 167 articles were identified for manual review (Fig. 2). Articles were independently screened by both authors to identify articles by the titles and abstract. In case of disagreement, it was discussed by both authors. Nine studies were finally chosen and included in the systematic review (Table 2).
Characteristics of included studies in the present systematic review.
| First author | Journal | Year published | Design | Participants | Intervention | Age, years (mean) | FEV1, %pred (mean) | Follow-up, months (mean) | Result |
|---|---|---|---|---|---|---|---|---|---|
| Bhatt et al.13 | Chest | 2018 | Multicentre, cohortsCOPD Gene | N=1017 | Agatston score 130–199; 200–299; 300–399; >400.Weston score: significative >7. | 61.8 | – | 69.6 | CV events: higher incidence in COPD (8.1% vs. 5.7%; p=0.041).FEV1 is indirectly related to CC.Visual scale corresponds to the Agatston. |
| Budoff et al.10 | Circulation | 2018 | Multicentre, cohortsCOPD Gene | COPDN=6482 | Chest CT scan, low dose.Agatston score: 0; 1–100; 100–400; >400. | – | – | 81.3 | Mortality: relation between GOLD stage and CC. |
| Gaisl et al.14 | PLoS One | 2015 | Cohorts 1/1 (Switzerland) | N=81 | SPECT/CT.Agatston score: <100; 100–400; >400. | 64.3 | 28% | 42.6 | No differences in CC between patients with and without COPD.Higher CV events in COPD patients (19 vs 9, p=0.030).No difference in mortality in COPD patients (26 vs 22, p=0.423). |
| O’Hare et al.11 | J Comput Assist Tomography | 2014 | Cohorts(Australia) | COPD without other comorbiditiesN=200 | Chest CT scan, high resolution.Visual score (0–12 points): no=0, low=1 (<1/3), mild=2 (1/3–2/3), severe=3 (>1/3). 2 radiologists. | 68.6 | 47% | 36 | All-cause mortality was related to higher CC. |
| Romme et al.12 | Respiratory Research | 2013 | Cohorts(United Kingdom) | N=119 | Chest CT scan, low dose.Agatston score: <100; 100–400; >400. | 67.8 | 46% | 65 | Mortality. All causes of mortality after adjustment for age, sex, FEV1 and pack-year. |
| Takei et al.16 | Respiratory Medicine | 2021 | Cohorts (Japan)Hokjaido and Kyoto | Kyoto COPD cohortN=128 | Chest CT.Agatston score. | 70 | 65% | 118 | Mortality. Score combining CC and pulmonary artery diameter greater sensitivity. |
| Williams et al.9 | Thorax | 2014 | Multicentre, cohortsECLIPSE | COPD (FEV1 <80%)N=672 | Chest CT scan, low dose.Agatston score: <100; 100–400; 400–1000; >1000. | 63.2 | 54% | 36 | Mortality, overall and adjusted for age/gender/pack-year/COPD severity/history of CV disease. |
| Yang et al.17 | Chest | 2024 | Multicentre, COPD Gene cohort | COPD (FEV1 <80%)N=2831 | Chest CT scan, inspiration and expiration.Agatston score. | 63.8 | 51% | 105 | Mortality and CV events. Assessment in different COPD subtypes. |
| Zagaceta et al.15 | Respiratory Research | 2017 | Cohorts (Spain) | COPD without exacerbations in the last 8 weeksN=287 | Chest CT scan, low dose.Visual score (0–12 points): no=0, low=1 (<1/3), mild=2 (1/3–2/3), o severe=3 (>1/3). 2 radiologists. | 64 | 70% | 65 | CC the strongest independent predictor of CV event. |
CC: coronary calcium; COPD: chronic obstructive pulmonary disease; CT: chest tomography; CV: cardiovascular; Pred: predicted.
These studies, were conducted between 2013 and 2024, were predominantly multicentre and used a cohort study design.
Subjects were predominantly male (ranging from 56% to 96%, depending on the study), with mean ages between 54 and 70 years old. There was considerable variability in sample sizes among the studies (as described in Table 2): five studies included between 81 and 287 subjects, while three studies included over a thousand patients (1017,13 283117 and 648210). The reported prevalence of smokers showed a high variability (from 19% in the study by O’Hare et al.11 to 50% in the one by Zagaceta et al.15). Prevalence and number of CV risk factors reported varied in the different studies included in the analysis: 8 reported the prevalence of hypertension (ranging from 10% to 63%), 7 reported diabetes mellitus prevalence (ranging from 4.1% to 20%), 6 reporting dyslipidaemia prevalence (ranging from 32% to 71%) and one study reported other CV risk factors such as chronic kidney disease.
The main reason for requesting a chest CT scan was lung cancer screening in high-risk patients (varying the criteria on the study protocol) as currently recommended by the GOLD guidelines.2 Most studies9,10,12,15 were conducted using a low-dose protocol, although one study3 used high-resolution and another6 employed SPECT/CT. Agatston score was the most used method to evaluate CC, although different cut-offs were used depending on the study, as shown in Table 2. Only two studies11,15 used visually CC assessment.
The mean follow-up period ranged from 36 to 118 months. There was limited standardization among studies in the way CV outcomes were evaluated.
In the study by Williams et al.,9 it was observed that after adjusting for age, sex, and pack-year index, patients with higher CC or CC percentile exhibited increased mortality risk, with hazard ratios of 1.42 (95% confidence interval 1.12–1.78) and 1.77 (95% confidence interval (CI)1.04–3.01), respectively. Similar results were obtained by other studies: Budoff et al.10 (1.68; 95% CI 1.30–2.03), Romme et al.12 (2.01; 95% CI 1.13–3.58) and O’Hare et al.11 (2.03; 95% CI 1.08–3.82). The meta-analysis of those studies showed a hazard ratio of 1.57 (CI 1.35–1.83) with a heterogeneity index (I2) of 0%. Fig. 3 depicts those findings in a forest plot. Interestingly, despite a strong association between GOLD stage and CC, it was noted that mortality was independently associated with CC across all GOLD stages. On the other hand, Takei et al.16 developed a model in which they found that the combination of CC and pulmonary artery diameter had higher sensitivity in predicting subject mortality.
The meta-analysis of the three studies13,15,17 which analysed the risk of major CV events, showed a hazard ratio of 1.44 (95% CI 1.22–1.70), with I2 of 0%. Fig. 4 represents these findings in a forest plot. When compared to all non-invasive markers of CV risk, Zagaceta et al.15 demonstrated that CC was the strongest independent predictor of CV events, including the well-established SCORE CV risk index. Gaisl14 and Bhatt et al.13 also found that CV events were more common in patients with CC; however, Gaisl et al.14 did not found a statistical difference in mortality. Yang et al.17 described a stronger association between CC and CV events in non-emphysema-predominant disease compared with those with emphysema-predominant disease and intermediate emphysema.
DiscussionThe main conclusion of this systematic review of the literature suggests that CC detection in chest CT scans of asymptomatic COPD patients is associated with an increased ischemic CV event and a higher risk of mortality from this cause.
Screening techniques for asymptomatic patients are effective when reliable, cost-effective diagnostic tests are available for early asymptomatic detection, along with effective treatments that can reduce mortality from the detected condition. A recently validated example is low-dose chest CT for early lung cancer detection in asymptomatic high-risk patients, which has been shown to reduce mortality from lung cancer.22,23 In addition to early lung cancer screening, chest CT scan may be useful for identifying other relevant findings in COPD management such as the presence of emphysema, bronchiectasis, CC, increased diameter of the pulmonary and aortic arteries, hepatic steatosis, psoas density or osteoporosis24. However, its routine use for these purposes is not standardized in COPD patients.
In the current context of developing and implementing lung cancer screening programs, GOLD guidelines included the recommendation of including COPD patients due to their high risk.2 The use of screening chest CTs would allow us to diagnose and potentially treat asymptomatic COPD patients with high CV risk.
The most validated method for CC assessment is the Agatston scale, which combines both plaque volume and density in its assessment (Fig. 1).13 Its evaluation was first described in electrocardiogram (ECG) gated chest CT (which may limit result generalization), but recent studies have shown good agreement between ECG gated CT scans and those without it.25,26 Additionally, its measurement is not standardized, and some studies score plaque density in different ways. As it is an observer-dependent parameter, to avoid biases, the included studies detailed how radiologists had to be experienced, and adequate inter-observer correlation was checked. In the study by Bhatt et al.,13 different scales were applied to COPD patients, and it was found that, besides detecting CV events, there was a correlation between the Agatston and visual (Weston) scores. Among the advantages of visual scoring is its easy application and intra- and inter-observer agreement.
To understand the impact of a diagnostic technique, the study design is of vital importance. The variability of results may be influenced by different research protocols. Pairing groups as in the study by Gaisl et al.14 may help to avoid errors in external validity. Additionally, biases may arise due to differences in the severity of COPD patients, which can limit the external validity of the results. Significant variability was observed in smoking habits across studies, which can affect result interpretation, as former smokers may have a lower CV risk.27 Most studies reported the presence of other CV risk factors (hypertension, diabetes mellitus, smoking habits, …), although the parameters reported (both diagnostic criteria, cut-offs and treatment) varied between the studies. Some patients had concomitant CV risk factors that could influence CV outcomes. Despite the limitation for the interpretation of the results, it could better represent the real-life situation of combination of several CV risk factors. Only one study (Zagaceta et al.15) calculated CV risk using scores (Framingham and SCORE scales). None of the studies reported the level of physical activity, despite it is a recognized CV risk factor. The NAVIGATOR study28 highlighted this by showing that even small reductions in daily physical activity (for example, 2000 fewer steps) corresponded with increased CV risk in high-risk populations.
In addition to the importance of CC assessment in stable patients, studies such as that of Leong et al.29 have reported that 35% of patients admitted for exacerbation of COPD had severe CC (Agatston score higher than 400 points). Recently, Xu et al.30 have also highlighted the potential usefulness of CC as a predictor of CV mortality in the exacerbated patient. This suggests that exacerbations may be a good time to assess this CV risk marker to optimize treatment and follow-up of these high-risk patients. However, Wade et al.31 did not discover an association between CC and exacerbation risk.
Our systematic review has limitations related to the characteristics of the study as discussed above. The most important, as in any systematic review of the literature, the methodology used in the studies is often different, as well as the characteristics of the population included in the analysis, sample size, analysis of other risk factors, consideration of interventions for CV risk modification, potential impact of COPD treatments on CV risk,2 and so on. Moreover, the included studies had an observational design, and common biases related with that design may have occurred: absence of chance, confusion bias and selection bias, observing that none of them adjusted the odds ratio in the article with the consequent possible loss of precision. Further prospectively designed, multicentre studies are needed to appropriately answer the proposed question. In addition, it would be useful to know whether the detection and treatment of CV risk detected in these asymptomatic patients through CC screening translates into a reduction in ischemic CV events and mortality.
ConclusionsDespite the lack of standardization in terms of determination of CC and the lack of direct intervention data, the present systematic review of the literature suggests that CC detection is associated with an increased risk of ischemic CV events and CV mortality. It may be a potential additional tool for the clinician and patient to motivate to initiate preventive interventions. Further studies are needed to determine if detecting CC in COPD patients allows early treatment of ischemic CV disease with a consequent impact on CV events and mortality.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors’ contributionsBoth authors contributed equally to this manuscript.
Conflicts of interestThe authors declare not to have any conflicts of interest that may be considered to influence directly or indirectly the content of the manuscript.