The term Home Respiratory Therapies (HRT) includes long-term oxygen therapy, continuous positive airway pressure (CPAP), and diverse forms of ventilatory support.1 Despite the undeniable benefits of HRT, it is important to acknowledge their significant impact on patients and their families, with high rates of anxiety, depression and caregiver burden syndrome being reported.2,3
In the last years, the evaluation of the patient's experience within the healthcare system has gained substantial prominence.4,5 In this context, Patient-Reported Experience Measures (PREM) and Patient-Reported Outcome Measures (PROM) have served as valuable tools for assessing the quality of care.6 PROM are results provided by patients based on their perception of their health status, quality of life, symptoms, mental health and functional condition associated with the care they receive or a treatment. There are both generic PROM (developed for general measurement) and specific PROM (developed for a specific health problem or population).7–9 Our group has been at the forefront of applying PREM and PROM to patients on HRT.10–12
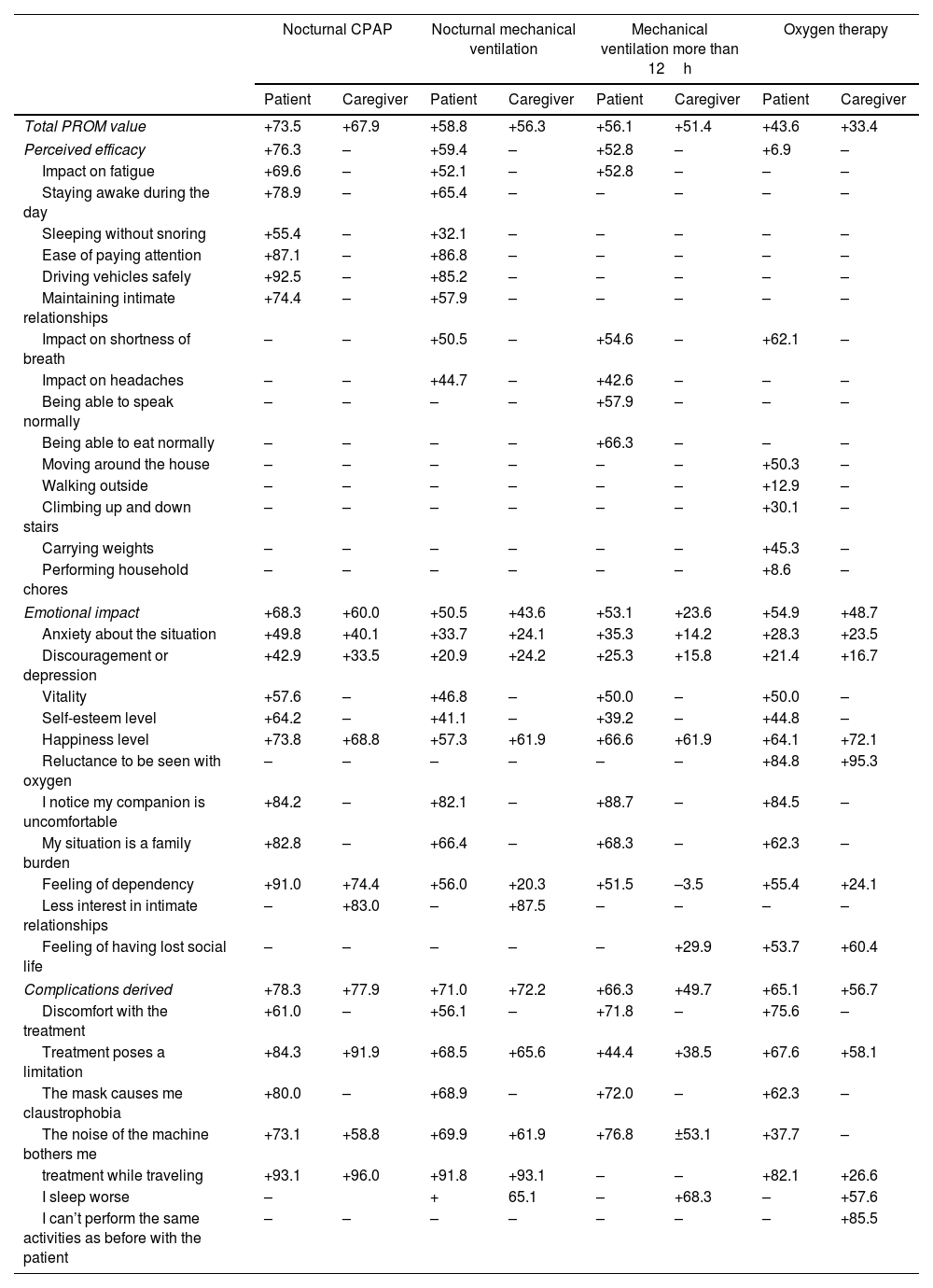
To our knowledge, there are no published studies in the literature that compare PROM results between patients and caregivers. To address this issue, we have designed a study with the objective of comparing specific PROM across four distinct patient groups: those receiving nocturnal CPAP, patients on nocturnal mechanical ventilation (MV), patients requiring mechanical ventilation for more than 12h per day (MV>12h), and those undergoing oxygen therapy at home. The study also evaluated the specific PROM for their caregivers.
A computer assisted telephone interviewing (CATI) was conducted in patients undergoing HRT and registered in the database of the home care provider company OXIMESA Nippon Gases (Spain), as well as their caregivers. The PROM questionnaires for patients addressed 18 variables specific for patients and therapies, grouped around five dimensions: general health status, impact of the disease, perceived efficacy, emotional impact, and complications arising from treatment. Caregiver's PROM was similar excluding the “impact of the disease” dimension. The obtained PROM value was not an average or a direct percentage, but a weighted and rescaled percentage within a range from −100 (the worst possible situation) to +100 (the best possible situation). This means that statistical tests such as standard deviations or confidence intervals have not been applied to these data.
CATI was conducted on a selection of patients chosen through simple random sampling. A Spanish representative sample was calculated according to profile and therapy with a maximum sampling error of ±5% for an infinite universe and a confidence level of 95.5%, in the assumption of maximum indeterminacy (p=q=0.5). The survey was carried out by a specialized company in performing CATI studies (adn marKet), and patients were asked for their collaboration. Participants were assured of their anonymity, and they gave their consent to be included in the study. The study was approved by the CEIC. The collected data were analyzed classifying the scores into quartiles and directly comparing the results between patients and caregivers.
In the period May 2022–April 2023, 3200 PROM questionnaires were conducted. The net response rate (valid surveys/positive phone contacts) was of 70.4%. The distribution of patients and caregivers involved, according to the type of HRT prescribed, was 1600 patients (440 oxygen, 440 CPAP, 390 VM, 280MV>12h), and 1600 caregivers (440 oxygen, 440 CPAP, 390 VM, 280 VM>12h). The distribution of patients by duration of therapy was balanced to reflect real-world scenarios (89% of the included patients had been on therapy for more than 1 year). The main PROM results of patients are shown in Table 1. According to the Global PROM value, CPAP was the best rated therapy (+73.5) and oxygen therapy the worst (+43.6). CPAP was also perceived as the most effective therapy by patients, with a score of +76.3. On the other hand, oxygen therapy was perceived as the least effective, with a score of +6.9. The therapy that produced the most emotional impact was VM (+50.5), while CPAP had the least emotional impact (+68.3). Interestingly, patients with VM>12h reported less emotional impact (+53.1) than those with VM (+50.5). Treatment complications were mild and especially reported by patients with oxygen therapy (+65.1) compared to those with CPAP (+78.3). The PROM of caregivers showed lower global values in all therapies and a greater emotional impact (e.g., VM>12h patients +53.1 vs caregivers +23.6). Certain emotional aspects were interesting. For example, caregivers scored higher the effect on the libido of CPAP (+83.0) than patients did (+74.4).
Main PROM value obtained in patients and caregivers. Higher values mean less impact of the dimension analyzed.
| Nocturnal CPAP | Nocturnal mechanical ventilation | Mechanical ventilation more than 12h | Oxygen therapy | |||||
|---|---|---|---|---|---|---|---|---|
| Patient | Caregiver | Patient | Caregiver | Patient | Caregiver | Patient | Caregiver | |
| Total PROM value | +73.5 | +67.9 | +58.8 | +56.3 | +56.1 | +51.4 | +43.6 | +33.4 |
| Perceived efficacy | +76.3 | – | +59.4 | – | +52.8 | – | +6.9 | – |
| Impact on fatigue | +69.6 | – | +52.1 | – | +52.8 | – | – | – |
| Staying awake during the day | +78.9 | – | +65.4 | – | – | – | – | – |
| Sleeping without snoring | +55.4 | – | +32.1 | – | – | – | – | – |
| Ease of paying attention | +87.1 | – | +86.8 | – | – | – | – | – |
| Driving vehicles safely | +92.5 | – | +85.2 | – | – | – | – | – |
| Maintaining intimate relationships | +74.4 | – | +57.9 | – | – | – | – | – |
| Impact on shortness of breath | – | – | +50.5 | – | +54.6 | – | +62.1 | – |
| Impact on headaches | – | – | +44.7 | – | +42.6 | – | – | – |
| Being able to speak normally | – | – | – | – | +57.9 | – | – | – |
| Being able to eat normally | – | – | – | – | +66.3 | – | – | – |
| Moving around the house | – | – | – | – | – | – | +50.3 | – |
| Walking outside | – | – | – | – | – | – | +12.9 | – |
| Climbing up and down stairs | – | – | – | – | – | – | +30.1 | – |
| Carrying weights | – | – | – | – | – | – | +45.3 | – |
| Performing household chores | – | – | – | – | – | – | +8.6 | – |
| Emotional impact | +68.3 | +60.0 | +50.5 | +43.6 | +53.1 | +23.6 | +54.9 | +48.7 |
| Anxiety about the situation | +49.8 | +40.1 | +33.7 | +24.1 | +35.3 | +14.2 | +28.3 | +23.5 |
| Discouragement or depression | +42.9 | +33.5 | +20.9 | +24.2 | +25.3 | +15.8 | +21.4 | +16.7 |
| Vitality | +57.6 | – | +46.8 | – | +50.0 | – | +50.0 | – |
| Self-esteem level | +64.2 | – | +41.1 | – | +39.2 | – | +44.8 | – |
| Happiness level | +73.8 | +68.8 | +57.3 | +61.9 | +66.6 | +61.9 | +64.1 | +72.1 |
| Reluctance to be seen with oxygen | – | – | – | – | – | – | +84.8 | +95.3 |
| I notice my companion is uncomfortable | +84.2 | – | +82.1 | – | +88.7 | – | +84.5 | – |
| My situation is a family burden | +82.8 | – | +66.4 | – | +68.3 | – | +62.3 | – |
| Feeling of dependency | +91.0 | +74.4 | +56.0 | +20.3 | +51.5 | –3.5 | +55.4 | +24.1 |
| Less interest in intimate relationships | – | +83.0 | – | +87.5 | – | – | – | – |
| Feeling of having lost social life | – | – | – | – | – | +29.9 | +53.7 | +60.4 |
| Complications derived | +78.3 | +77.9 | +71.0 | +72.2 | +66.3 | +49.7 | +65.1 | +56.7 |
| Discomfort with the treatment | +61.0 | – | +56.1 | – | +71.8 | – | +75.6 | – |
| Treatment poses a limitation | +84.3 | +91.9 | +68.5 | +65.6 | +44.4 | +38.5 | +67.6 | +58.1 |
| The mask causes me claustrophobia | +80.0 | – | +68.9 | – | +72.0 | – | +62.3 | – |
| The noise of the machine bothers me | +73.1 | +58.8 | +69.9 | +61.9 | +76.8 | ±53.1 | +37.7 | – |
| treatment while traveling | +93.1 | +96.0 | +91.8 | +93.1 | – | – | +82.1 | +26.6 |
| I sleep worse | – | + | 65.1 | – | +68.3 | – | +57.6 | |
| I can’t perform the same activities as before with the patient | – | – | – | – | – | – | – | +85.5 |
PROM: Patient-Reported Outcome Measures.
Our results highlights that the impact of various HRT differs among patients, according to their different profiles and characteristics. Patients with obstructive sleep apnoea (OSA) reported a greater perceived efficacy and lesser emotional impact than patients with other types of HRT, being the patients on oxygen therapy those with the worst results. Most OSA patients experience a significant improvement in symptoms after starting CPAP treatment, making it easy to perceive the effectiveness of the treatment. This contrasts, for example, with patients receiving oxygen therapy, who are usually diagnosed with advanced chronic diseases and generally have significant associated comorbidities, what means more symptomatic patients despite of the treatment. Studies have shown us that oxygen therapy had a major psychological impact on the daily lives of both patients and their families, and cause social isolation.13
A great finding has been that in all therapies analyzed, the therapy impacted emotionally more on caregivers than on patients. It is well known the risk of caregiver burden syndrome in people caring for complex patients, such as those dependent on mechanical ventilation. Our findings highlight that the emotional impact also extends to caregivers in other HRT, giving us the opportunity to appreciate the relevance to develop strategies focused on them.
Our study has limitations related to selection bias, technological barriers, response bias, and biases inherent in the CATI methodology. In conclusion, PROM in HRT allow a better discrimination of the efficacy perceived and emotional impact of each of the therapies on patients and caregivers and help us to consider alternatives care approaches.
FundingThis manuscript has not been supported by any funding or grant.
Authors’ contributions- -
Salvador Díaz Lobato has contributed to the conception, development, discussion and writing of this manuscript.
- -
Johanny Vargas Rodriguez has contributed to the conception, development, discussion and writing of this manuscript.
- -
David Sampedro has contributed to the conception of the study, the development and administration of the questionnaires, the analysis of the results, the discussion, and the writing of the manuscript.
- -
Jesús García Camacho has contributed to the conception of the study, the development and administration of the questionnaires, the analysis of the results, the discussion, and the writing of the manuscript.
- -
Catia Caneiras has contributed to the conception, development, discussion and writing of this manuscript.
- -
Sagrario Mayoralas Alises has contributed to the conception, development, discussion and writing of this manuscript.
Authors declare not to have any conflict of interest related to this manuscript.