We report the case of a 48-year-old male patient, never-smoker, with no respiratory symptoms of any kind, whose history includes right hemibody epileptic seizures secondary to surgery for a WHO grade I meningioma in 2007.1
He was referred to respiratory medicine for study of at least 10 bilateral pulmonary nodules of soft tissue density, homogeneous, with smooth and well-defined contours that were discovered incidentally after a chest computed tomography scan performed due to multiple injuries sustained after a car accident in March 2023.
The study was completed with a positron emission tomography that confirmed the presence of these bilateral lung nodules that were indeterminate from a metabolic point of view. These nodules showed low avidity for fluorodeoxyglucose (FDG), and low-grade tumor processes or metastases could not be ruled out.
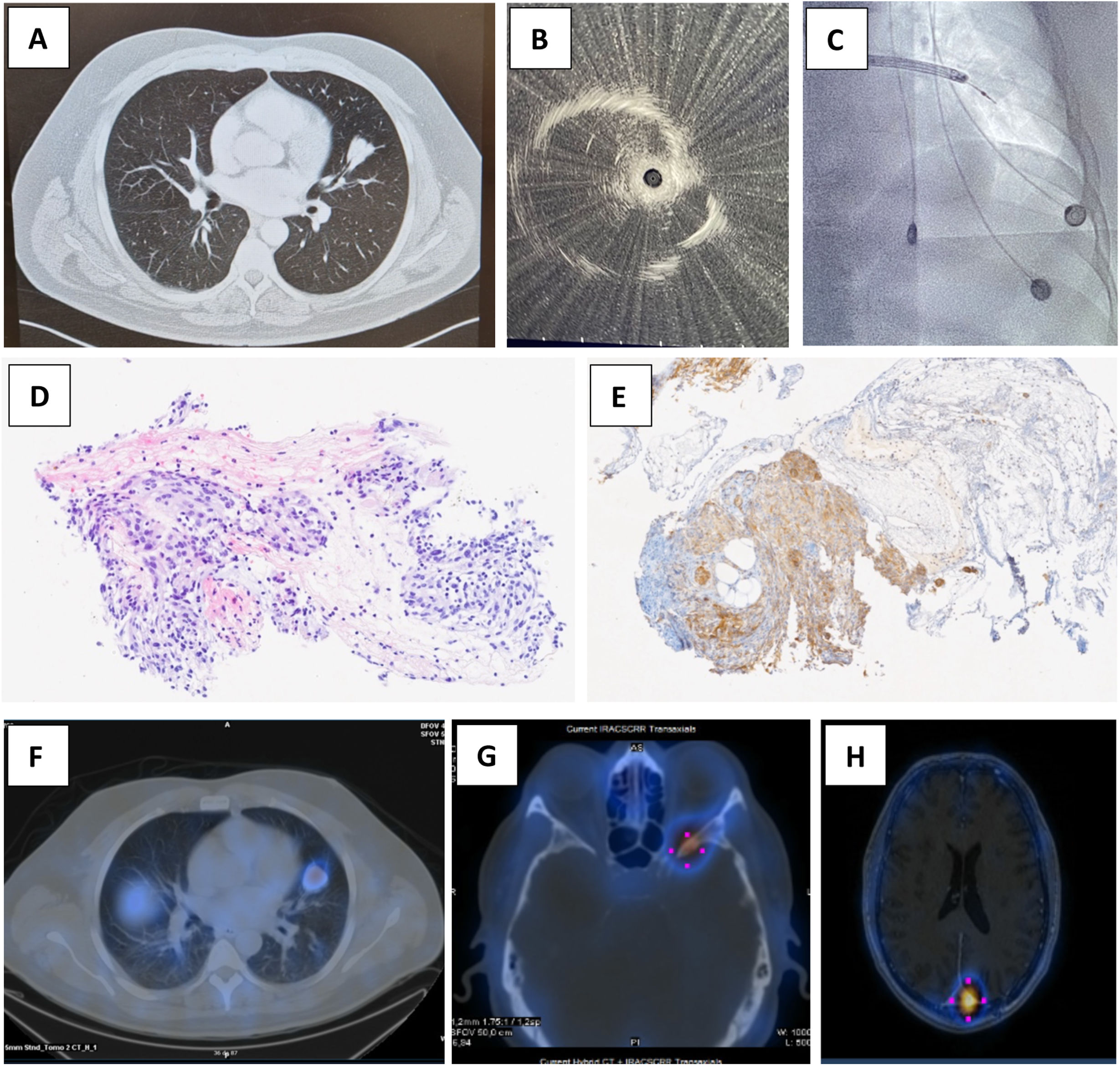
Once the anatomical location of the lesions had been assessed, we decided to attempt a histological characterization of one of the nodules, opting for the one located in the upper segment of the lingula, since it was the largest and because it had a drainage bronchus accessible by radial endobronchial ultrasound (EBUS) (Fig. 1A).
Computed tomography image of the biopsied nodule and its draining bronchus (A). Radial EBUS images of lung lesion by ultrasound (B) and fluoroscopy (C). Histological section stained with hematoxylin–eosin showing a small nest of cells with a meningotheloid appearance in the interstitium (D) and focal positivity (brown) for somatostatin receptors in the complementary immunohistochemistry study (E). Uptake increase in SPECT associated with lung lesions (F) and bone metastasis (G and H).
In July 2023, radial EBUS was performed, with localization of the lesion by both ultrasound and fluoroscopy (Fig. 1B and C). Five brushings and 5 forceps biopsies were performed on the nodule and a bronchial aspirate was obtained from the guide sheath.
Bronchial aspirate and brushing cytology testing was negative. In contrast, the endoscopic biopsy showed meningothelioid cell nests with positivity for progesterone and vimentin receptors. A histological diagnosis consistent with meningothelial-like nodule/meningioma was established (Fig. 1D).2,3 A complementary study with immunohistochemistry was also performed with somatostatin receptors that showed focal positivity (Fig. 1E).4,5
The diagnostic process was completed with a somatostatin receptor scintigraphy (SPECT), which showed an increase in tracer uptake in lung nodules associated with lesions that express somatostatin receptors,4,5 which also suggested that they corresponded to metastatic meningioma lesions (Fig. 1F). The SPECT itself also revealed focal uptake in the left parietal region (tumor remains of the already known primary meningioma) (Fig. 1G) and in the greater wing of the left sphenoid (Fig. 1H).6
The extraordinary feature of this case lies in the presence of pulmonary metastases from a primary meningioma that was initially benign and controlled, 17 years after the diagnosis of the primary lesion. It is significant that the finding was incidental because the patient is asymptomatic both at respiratory and neurological levels, despite the fact that the neoplastic disease is progressing. Meningioma is the most common primary brain tumor. Within this group, the majority are WHO grade I (75%), defined as benign. The recurrence of a well-treated grade I meningioma is 3% at 5 years,1–3 while metastatic disease is extremely rare (<0.1%).6 The most common metastatic sites are the lung, bones, liver and soft tissues.6
Furthermore, the case was diagnosed using a unusual bronchoscopic technique that is not available in all centers, in which the images were indistinguishable from a primary lung tumor. So far, there is no published article that describes the diagnosis of pulmonary meningioma metastasis using radial EBUS. The overall diagnostic yield of this technique varies between 40% and 70% depending on the size of the lesion, location, experience of the team, etc. The most frequent complications are bleeding and pneumothorax.7
Regarding treatment, the FDA/EMA does not currently approve any specific medication for the treatment of metastatic meningioma and any pharmacotherapy is experimental.3 It has been shown that all categories of meningiomas overexpressed the somatostatin receptor subtype 2 (SSTR2). For this reason, SPECT is a valuable tool for diagnosis based on this general expression of SSTR2. However, a positive octreotide scan is only indicative of presence and is not sufficient to predict response.4,5 The use of somatostatin analogs may be a promising treatment for patients with metastatic meningiomas since it stabilizes or slows tumor progression for months, but more studies are required to confirm this suspicion and establish therapeutic recommendations.6,8
In conclusion, in a patient with multiple lung lesions with a history of meningioma, especially with local recurrence, one of the differential diagnoses to consider is metastatic meningioma.
Informed consentThe authors declare that they have the patient's consent for publication.
In this article, our hospital protocols on the publication of patient data have been followed and patient privacy has been respected.
FundingThis research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Authors’ contributionsAll authors have contributed substantially to the conception and drafting of the clinical case and to a critical reading prior to the submission of the manuscript.
Conflicts of interestThe authors declare no conflicts of interest that might directly or indirectly influence the content of the manuscript.