This document proposes a value-based care model to improve adherence and health outcomes in patients with obstructive sleep apnea (OSA) treated with CPAP. The current care model for OSA management adopts a uniform, volume-based approach for all patients, limiting personalized care and reducing service quality without providing objective outcome data. The value-based care model proposed here focuses on guiding all interventions towards improving treatment adherence, aiming to enhance health outcomes by increasing patients’ quality of life and comfort with treatment. Key strategies to be implemented include education and support programs at the beginning of treatment, enhancing comfort in mask use, telemonitoring of adherence, patient involvement in the treatment progress, patient stratification based on adherence, and identifying individuals who may benefit from alternative treatments. A results-based funding model is also recommended to optimize resource allocation. Expected outcomes from these measures include a reduction in home visits and in-person consultations for stable patients, fewer non-adherent patients, more optimally treated patients, and overall improvements in treatment quality and effectiveness. Key indicators to evaluate the success of this approach include quality of life (measured through quality-of-life questionnaires), adherence levels (via telemonitoring), and CPAP comfort. Collectively, these strategies allow for a comprehensive approach, optimizing resources and ensuring personalized care that improves the experience and outcomes of OSA patients.
Este documento propone un modelo asistencial basado en valor para mejorar la adherencia y resultados en salud de pacientes con apnea obstructiva del sueño (AOS) tratados con CPAP. El modelo asistencial actual del manejo de la AOS sigue un enfoque único y estandarizado para todos los pacientes y está basado en volumen de pacientes, lo que limita la atención personalizada y disminuye la calidad del servicio sin ofrecer datos objetivos de resultados. El modelo asistencial basado en valor propuesto en este documento se basa en orientar todas las intervenciones en la mejora de la adherencia al tratamiento, con el objetivo de mejorar los resultados en salud aumentando la calidad de vida e incrementando el grado de confort de los pacientes con el tratamiento. Las estrategias clave a implementar incluyen: programas de educación y soporte al inicio del tratamiento, mejora del confort en el uso de mascarillas, telemonitorización de la adherencia, hacer partícipe al paciente de la evolución de su tratamiento, estratificación de los pacientes según su adherencia e identificación de aquellos que puedan beneficiarse de tratamientos alternativos. Además, se sugiere un modelo de financiación basado en resultados para optimizar los recursos. Con la implementación de todas las medidas descritas se espera conseguir una: reducción de revisiones domiciliarias y visitas presenciales para pacientes estables; reducción en el porcentaje de pacientes no adherentes y aumento en aquellos con tratamiento óptimo; mejora en la calidad y efectividad del tratamiento. Los indicadores para evaluar el éxito de este itinerario incluyen: la calidad de vida (medida mediante cuestionarios de calidad de vida), el grado de adherencia al tratamiento (mediante telemonitorización) y el nivel de confort con la CPAP. En conjunto, estas estrategias permiten un enfoque integral, optimizando los recursos y garantizando una atención personalizada que mejora la experiencia y resultados del paciente con AOS.
Obstructive sleep apnea (OSA) is a highly prevalent disease that significantly impairs quality of life and is associated with an increased risk of cerebrovascular and cardiovascular events, accidents, and mortality. Continuous positive airway pressure (CPAP) is the treatment of choice for OSA patients, as it has been shown to effectively reduce sleep fragmentation, respiratory events, and nocturnal desaturation, thereby improving symptoms and associated risks. However, low adherence to CPAP remains a notable issue, with current adherence rates (defined as use for more than 4h/night on 70% of nights) of around 60% among actively treated patients and a significant proportion of patients with very low adherence (use less than 1h/night).1 Good adherence not only ensures symptom control and enhances patients’ quality of life but is also a key factor in secondary cardiovascular prevention for OSA patients.2
For these reasons, it is essential to establish a care management model adapted to the specific needs of each patient group to improve treatment adherence. This document focuses on OSA patients undergoing CPAP therapy and proposes a value-based care model, centered on interventions and activities that provide health outcomes with the highest quality and safety but at a minimal cost. To achieve optimal efficiency, the value of care should be measured by the results obtained rather than the volume of services provided. A patient-centered care model requires service provider funding based on the value delivered rather than intervention costs alone.
In light of this approach, the objectives of this document are to highlight the value of home respiratory therapies for OSA patients based on existing evidence, and to identify the problems and challenges of the current care model, as well as the key actions necessary to offer a value-based care model, thereby accelerating the implementation of a value-based funding model.
Current care model for OSA: problems and challengesSleep apnea is a chronic condition that requires an integrated and coordinated care model involving all health professionals and home respiratory therapy (HRT) providers. Managing this disease exclusively from specialized units results in increased waiting lists and high follow-up costs.3 Therefore, a multidisciplinary approach is proposed, combining risk factor prevention with specific treatments adjusted to each patient's characteristics.
HRT funding in Spain may come from the National Health System (NHS), private insurers, or directly from patients. Most treatments (95%) are funded by the NHS, with an estimated annual budget of €214 million according to the Spanish Ministry of Health. The contracting model for the provision of HRT services in the public sector is based on competitive tenders, involving two main payment modalities: one with a fixed economic amount per treatment and another based on payment for the provision of services. The regulation dated March 3, 1999, governs HRT techniques under the NHS, setting conditions such as clinical stability, acceptance of treatment, and adherence to recommended hygiene and health measures. However, in the current context of deficit in healthcare spending and a progressive increase in the number of patients, public tenders are increasing the volume of patients without proportionally increasing the price of the service, making it difficult to implement a value-based model.
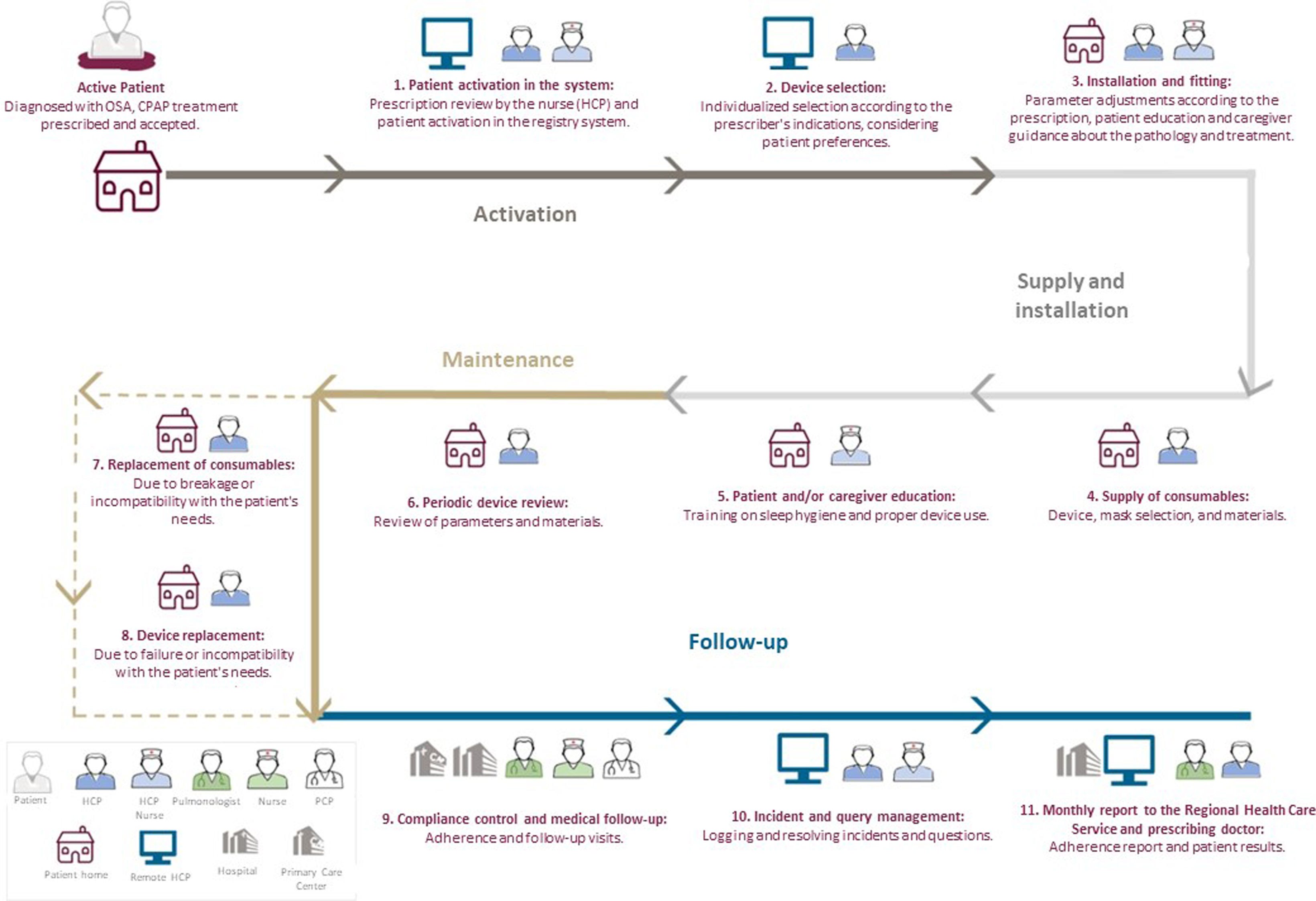
To analyze the current care model, the OSA patient pathway has been outlined based on the following sources of information: meetings with experts, input from HRT providers, patient interviews, and a literature review. This pathway focuses on the active patient already diagnosed with OSA who has been prescribed and accepted CPAP treatment (Fig. 1). The patient's interactions with each of the agents involved in his or her treatment and follow-up have been defined, determining the type of activity and the location where it is performed. Finally, the challenges and problems of each stage of the current itinerary have been identified.
The device activation stage begins when the patient accepts the prescribed treatment. The provider receives the prescription and activates the patient's profile in their system, selecting the most appropriate device according to the physician's recommendations. A key challenge at this stage is selecting and adapting the device to the patient's needs, optimizing resources.
Supply and installationThe device is supplied to the patient within a maximum of 2 days, either at home or in a specialized unit, where parameters of the device and masks are adjusted according to medical instructions. During installation, the patient receives guidance on device use and sleep hygiene measures. An important challenge here is ensuring patient adaptation from day 1 and engaging them in managing their therapy to promote adherence. There also remains a clear need to enhance education for both patients and caregivers.
MaintenanceThe provider performs periodic device revisions between 1 and 4 times a year, depending on contractual specifications. Consumable materials are replaced, and, if necessary, the device is repaired or replaced. A key challenge is to ensure an individualized maintenance service, tailored to each patient's needs, with early detection of potential issues to optimize resources.
Follow-upBetween the first and second month of treatment, the patient attends an in-person visit or is contacted remotely to assess treatment satisfaction and effectiveness. After the initial months, visits are scheduled semi-annually or annually, depending on patient stability. If treatment is effective and there are no side effects, follow-up is transferred to Primary Care. A crucial aspect is continuous monitoring of patient adherence to treatment. Providers generate monthly reports shared with health systems and physicians, so that adherence issues can be identified and reinforcing actions taken as needed.
Key challenges in follow-up include the need to stratify patients by adherence level and ensure closer follow-up for individuals with low adherence or complex conditions (e.g., professional drivers or patients with central apneas), measuring and analyzing health outcomes obtained through patient monitoring, and maintaining patient engagement with their treatment by immediately addressing any reported issues, doubts, or suggestions.
In summary, improving patient stratification, adjusting care to their specific needs, and reinforcing adherence monitoring are all essential. Patient and caregiver education should also be enhanced to promote correct device use. Moreover, the current price-based financing model does not place sufficient emphasis on the patient. It is crucial to offer patient-centered approach which prioritizes the outcomes that are important to the patient and fosters more open communication between patient and healthcare professional.
The next step in improving OSA management is to identify which outcomes are most important to patients, in order to establish an ideal pathway to optimize their treatment and follow-up, thereby improving quality of life and health outcomes.
Toward a value-based model for managing OSACurrently, OSA is managed following a standardized approach for all patients, with CPAP as the gold standard treatment. However, the diversity of patients with different needs, conditions, or degrees of adherence, suggests that there is a need to explore alternative therapies (such as mandibular advancement devices or positional therapy) that may be better suited to specific profiles or for individuals intolerant to CPAP. Both therapies have been shown to be effective in controlling daytime sleepiness, apnea-hypopnea index (AHI) and quality of life, with good tolerance and adherence.4–6
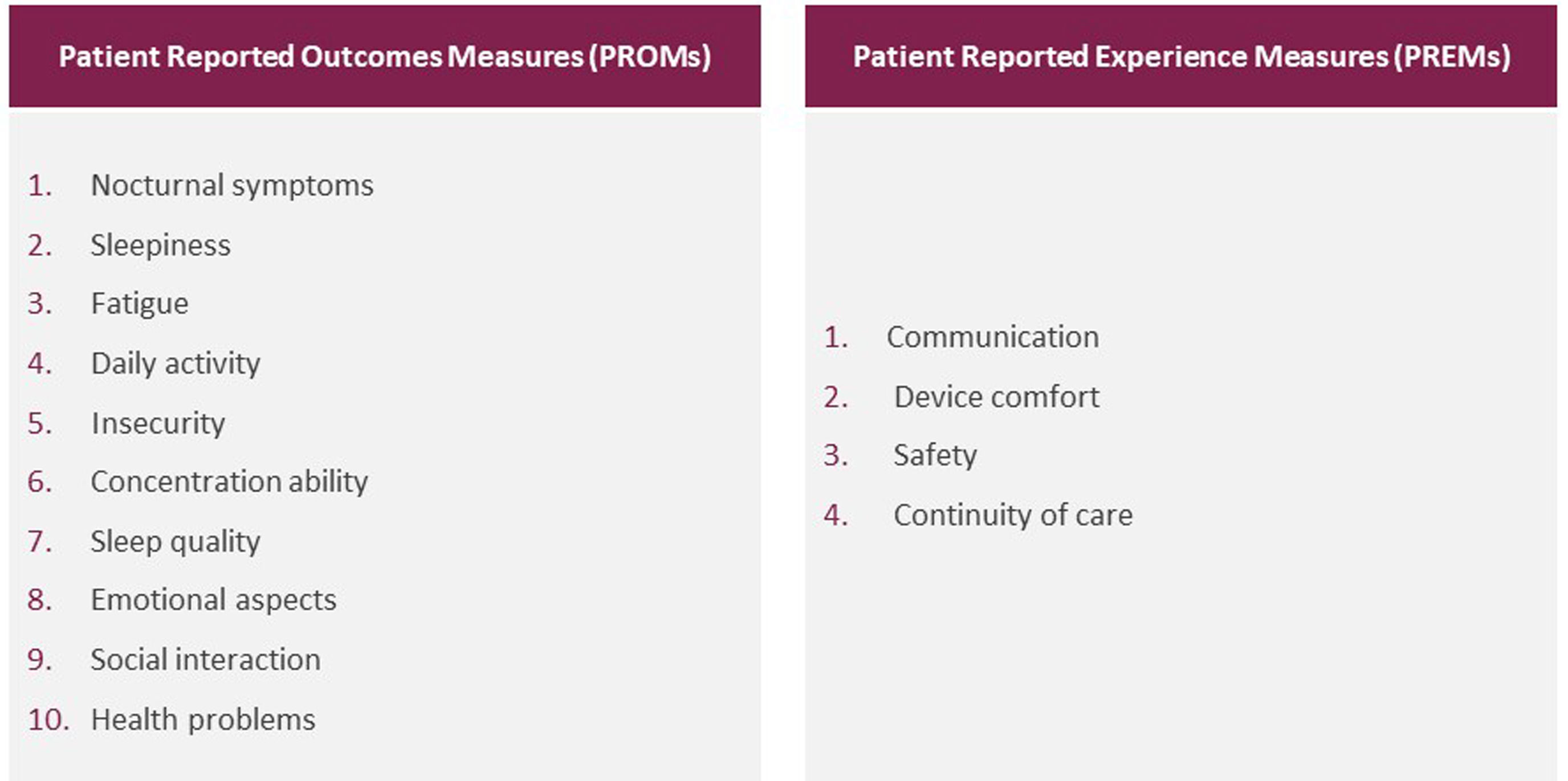
In a value-based care model, consideration must be given to the diverse profiles and needs of patients, taking into account expected health outcomes (Patient-Reported Outcomes Measures, PROMs) and patient care experience expectations (Patient-Reported Experience Measures, PREMs). This model also considers the variety of therapies available, the latest technologies, and a close relationship between the Sleep Unit team and the service provider responsible for ensuring service integrity and unity, regardless of the therapy provided.
After a literature review7,8 and interviews with OSA patients, a total of 10 PROMs and 4 PREMs were identified for consideration in a value-based care model (Fig. 2). Finally, our expert committee decided that the objective of the value-based intervention model should focus on improving one PROM – quality of life, that encompasses several identified measures – and one PREM – comfort with device use or treatment.
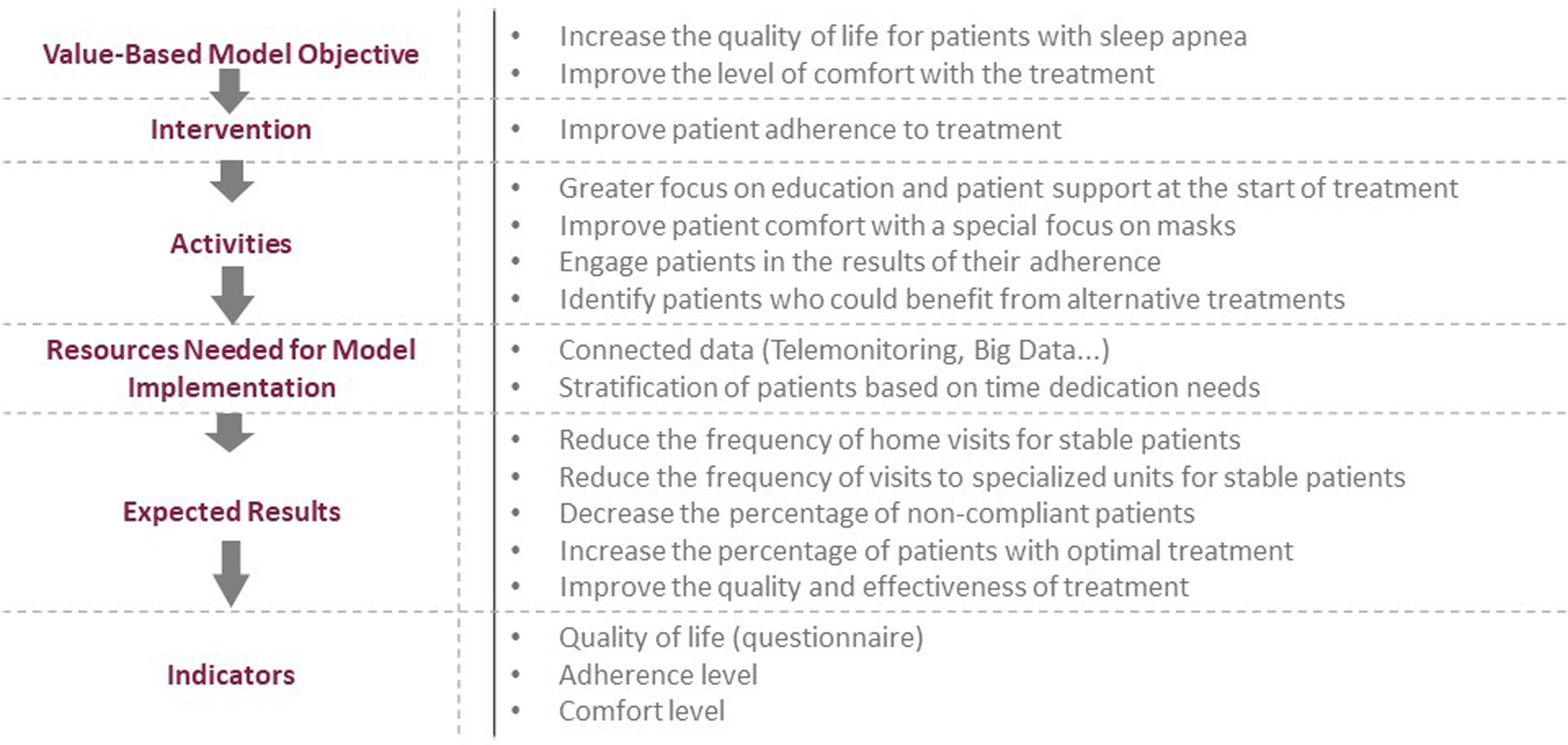
Intervention model to improve quality of life and comfort in OSA treatmentTo achieve the goals of improved quality of life and enhanced patient comfort, it is essential to improve adherence to treatment. The following proposals are suggested to enhance adherence:
- 1.
Patient education and support: It is essential, especially at the start of treatment, to provide comprehensive information on OSA, treatment and the importance of adherence. This includes verbal and written instructions on equipment use and maintenance and healthy habits.
- 2.
Improving device comfort: Selecting the most appropriate mask and device for each patient can increase comfort and thus adherence. Customizing equipment selection, such as pressure adjustments or humidifier use, is also crucial.
- 3.
Active patient participation: Encouraging patient engagement in treatment and device care can improve adherence. Patients should be informed of their progress and play an active role in managing their disease.
- 4.
Identification of non-adherent patients and alternative treatments: Identifying non-adherent CPAP patients who might benefit from alternative therapies, such as mandibular advancement devices or positional therapy, is crucial. Organizing this care process through a single service provider, regardless of the therapy provided, would be beneficial.
One essential resource for implementing this model involves the use of new technologies that allow data connectivity within large databases (Big Data), facilitating adherence assessment under real-world conditions. Proper data management will enable patient stratification based on needs and establish review protocols between HRT providers and sleep units, thereby improving clinical outcomes. CPAP adherence follow-up via telemonitoring has also proven effective and cost-efficient, facilitating the tracking of parameters such as air leaks, apnea-hypopnea index (AHI), and treatment compliance. Telemonitoring facilitates not only real-time patient tracking but also early intervention when problems are detected, reducing care burden and optimizing resource management. Studies by Turino et al.9 and Juarros Martínez et al.10 have shown that this approach is cost-effective and improves therapeutic compliance.
Implementation of these measures is expected to achieve the following outcomes: fewer home and in-person visits for stable patients; a decrease in the percentage of non-adherent patients and an increase in those optimally treated; and improvements in treatment quality and effectiveness. Success indicators for this pathway include quality of life (measured through quality-of-life questionnaires), treatment adherence level (via telemonitoring), and CPAP comfort level.
Fig. 3 presents a schematic overview of the main aspects.
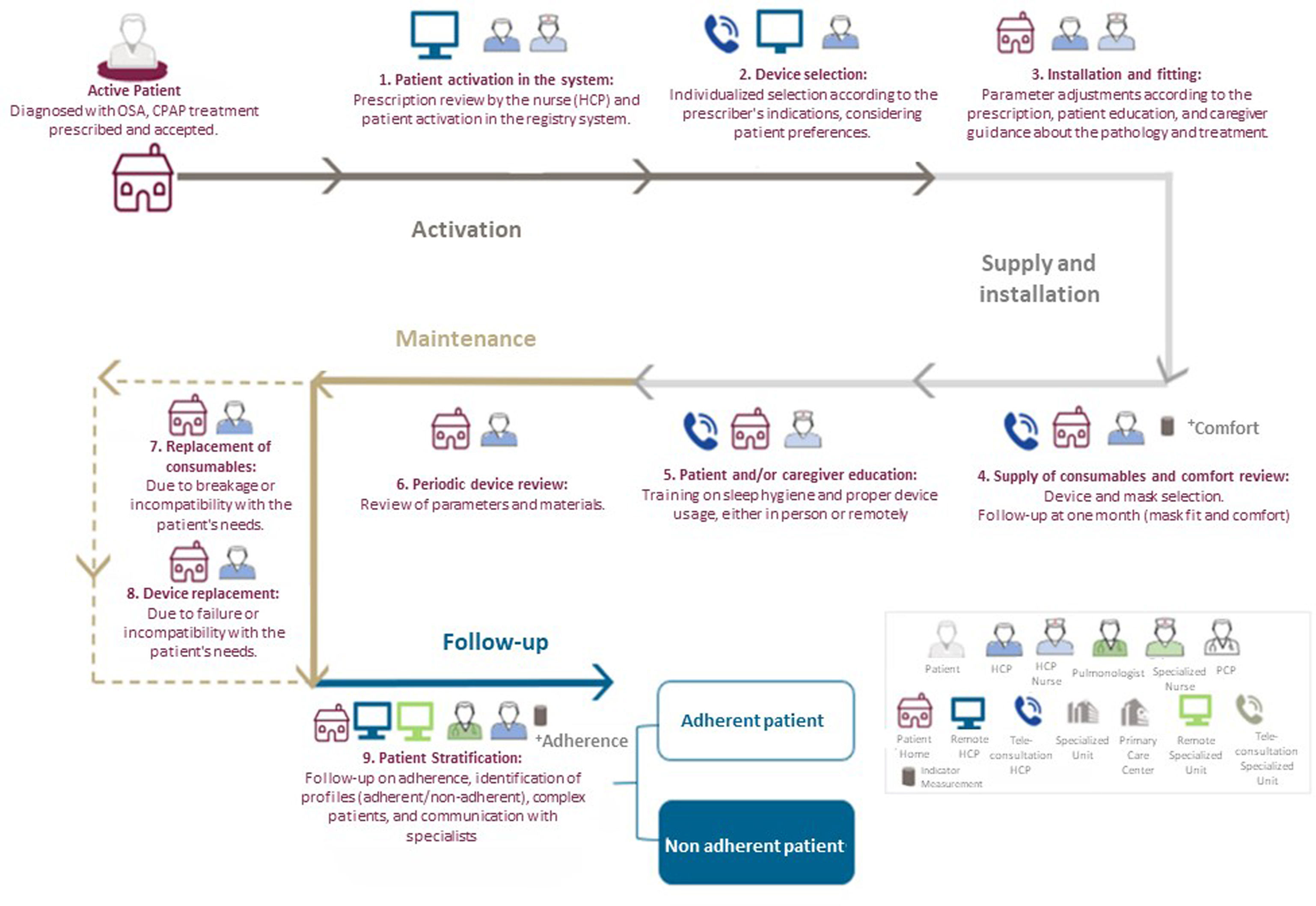
Ideal pathway in the value-oriented modelThe ideal itinerary for OSA patients on CPAP treatment to improve their quality of life has been defined. This itinerary builds on the real-world pathway and incorporates identified challenges. Furthermore, since not all patients adhere to their treatment to the same degree, telemedicine has been integrated into the pathway to foster an individualized approach that considers each patient's specific needs.11 Patient needs will differ based on adherence and, consequently, the activities and resources required will vary. Thus, the itinerary distinguishes two groups of patients according to CPAP adherence: adherent patients (CPAP use ≥4h/night) and non-adherent patients (use <4h/night). The cut-off point of 4h helps stratify the patient and assign them to an initial pathway, which can be adjusted during follow-up based on adherence levels. The ultimate goal is an optimal adherence of at least 6h per night, a threshold that has shown cardiovascular and symptomatic benefits.12,13
The ideal pathway for OSA patients on CPAP is outlined from the activation stage through the first part of the follow-up stage, when patients have not yet been classified as adherent or non-adherent. For the design of this itinerary, we have taken into account the SEPAR Guide for Home Respiratory Therapies14 (Fig. 4).
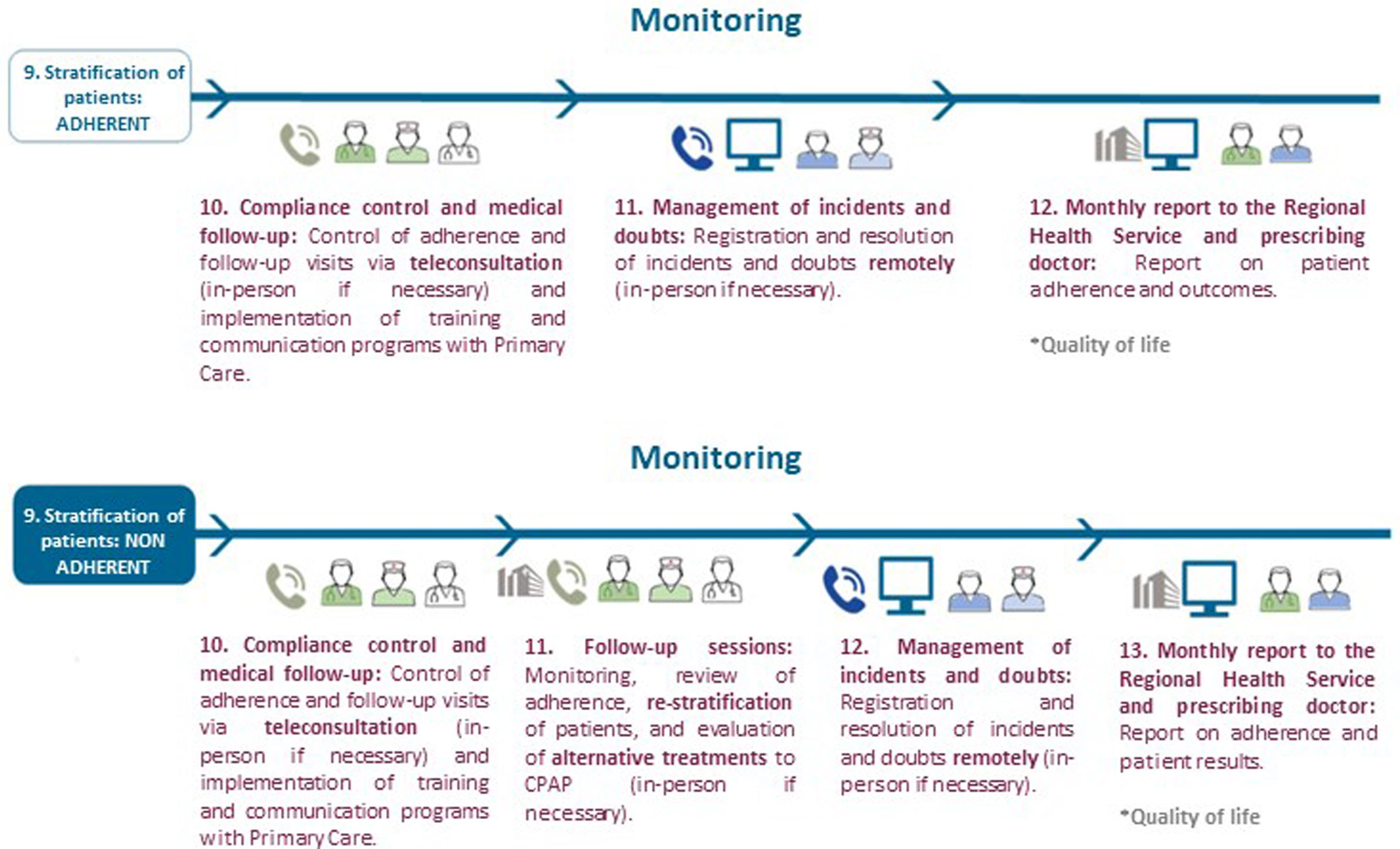
The initial stages of the pathway are the same for all patients; however, they diverge after follow-up and adherence evaluation. From that point onward, activities and resources vary. In the activation phase, the device is selected based on medical indications and patient preferences, as determined in a phone interview. During the supply and installation phase, pressure tolerance, interface suitability, and proper use of all equipment elements are verified. Cleaning and maintenance instructions are also provided (with periodic reviews every 6 months), along with an action protocol for potential adverse events. In the follow-up phase, weekly evaluations are conducted during the first month to monitor adherence. Subsequently, the provider classifies patients as “adherent” or “non-adherent”, adapting the pathway according to compliance profiles (Fig. 5). Complex patients requiring closer follow-up regardless of adherence (e.g., professional drivers with drowsiness, central apneas, etc.) are also identified.
For adherent patients, follow-up is prioritized through teleconsultation, with in-person consultations reserved for necessary situations. In this pathway, the role of Primary Care professionals is essential. Adequate training is crucial to enable these professionals to properly monitor the adherent patients, and continuing education programs and information-sharing methods should be implemented to ensure that this healthcare group is familiar with the intervention network.
For non-adherent patients, the pathway includes teleconsultations and, if necessary, in-person follow-up to enable early intervention in cases of side effects or poor compliance. These patients are offered the option to attend a CPAP school led by an expert patient who shares their experience, and follow-up sessions are conducted to understand the reasons for non-adherence, adapting them to each patient's needs. These sessions also enable patient re-stratification and the evaluation of alternative treatments for individuals who cannot adapt to CPAP, such as positional therapy or mandibular advancement devices.
This ideal pathway provides a structured framework for managing OSA treatment, aligning resources and activities according to patient adherence and promoting a more effective and personalized treatment approach. The success of the proposed care model depends on the effective implementation of the strategies mentioned. Individualized treatment, continuous patient education, resource optimization, and integration of alternative treatments for individuals who cannot tolerate CPAP are key elements to improving the quality of life of OSA patients.
RecommendationsBased on the analysis conducted, six recommendations are proposed to improve the care of sleep apnea patients (Fig. 6).
Telemonitoring enables real-time data access and treatment personalization through data generation (Big Data), facilitating the identification of specific patient needs. There are two types of telemonitoring: synchronous (real-time) and asynchronous (deferred data): the latter is easier to implement and is recommended as an initial method.11 Patient stratification allows resources to be allocated according to adherence level, focusing on individuals who need more support. It is also essential to tailor treatments to each patient's needs by incorporating personalized therapeutic options to optimize comfort and quality of life. Centralizing service management by a single provider ensures coordinated and continuous care, promoting collaboration among providers, manufacturers, and healthcare professionals. This collaboration is key to the follow-up and the implementation of shared protocols. Measuring adherence, quality of life, and comfort is indispensable to identify areas for improvement and ensure that the model objectives are achieved. Moving from a price-based financing model to a value-based model with integrated outcome indicators would focus care on achieving results that genuinely benefit patients. This new model would improve care quality, that is currently compromised under the existing model, and would ensure resource optimization. In summary, these strategies provide a comprehensive approach, optimizing resources and ensuring personalized care that enhances the experience and outcomes for OSA patients.
FundingThis study was not supported by any grant. ResMed and OxigenSalud contributed to the organization of the pulmonologist expert group meetings and patient interviews.
Ethical considerationsGiven the characteristics of the study, which develops a model for the management of a pathology in which no patients were directly involved, it was not necessary to request informed consent or to submit it to the Ethics Committee.
Authors’ contributionsIrene Cano-Pumarega contributed to the study design, conducted the systematic literature review, participated in all consensus meetings, contributed to the development of the recommendations, drafted the initial manuscript, and approved the final version.
Candela Caballero-Eraso contributed to the study design, conducted the systematic literature review, participated in all consensus meetings, contributed to the development of the recommendations, and read and approved the final manuscript.
Valentín Cabriada contributed to the study design, conducted the systematic literature review, participated in all consensus meetings, contributed to the development of the recommendations, and read and approved the final manuscript.
Mar Mosteiro contributed to the study design, conducted the systematic literature review, participated in all consensus meetings, contributed to the development of the recommendations, and read and approved the final manuscript.
Juan Fernando Masa contributed to the study design, conducted the systematic literature review, participated in all consensus meetings, contributed to the development of the recommendations, and read and approved the final manuscript.
Ferran Barbé contributed to the study design, conducted the systematic literature review, participated in all consensus meetings, contributed to the development of the recommendations, and read and approved the final manuscript.
Conflicts of interestNone declared.
The authors would like to acknowledge the collaboration of the other professionals involved in the preparation of this document: Resmed (Sara Correia, Hugo Almeida, Lucile Blaise, Anne Josseran) as a manufacturer of respiratory therapy equipment, Oxigen Salud (Jordi Blanco, Ana Mayoral) as a service provider, and Antares Consulting, allowing us to develop a model that would be sustainable and accepted by all potential participants in the project. The design, content and final drafting of the proposed document was entirely carried out by the pulmonologists involved in the project.