To identify preoperative factors associated with surgical time and conversion of the laparoscopic cholecystectomy (LC) to open surgery in subjects with acute cholecystitis (AC).
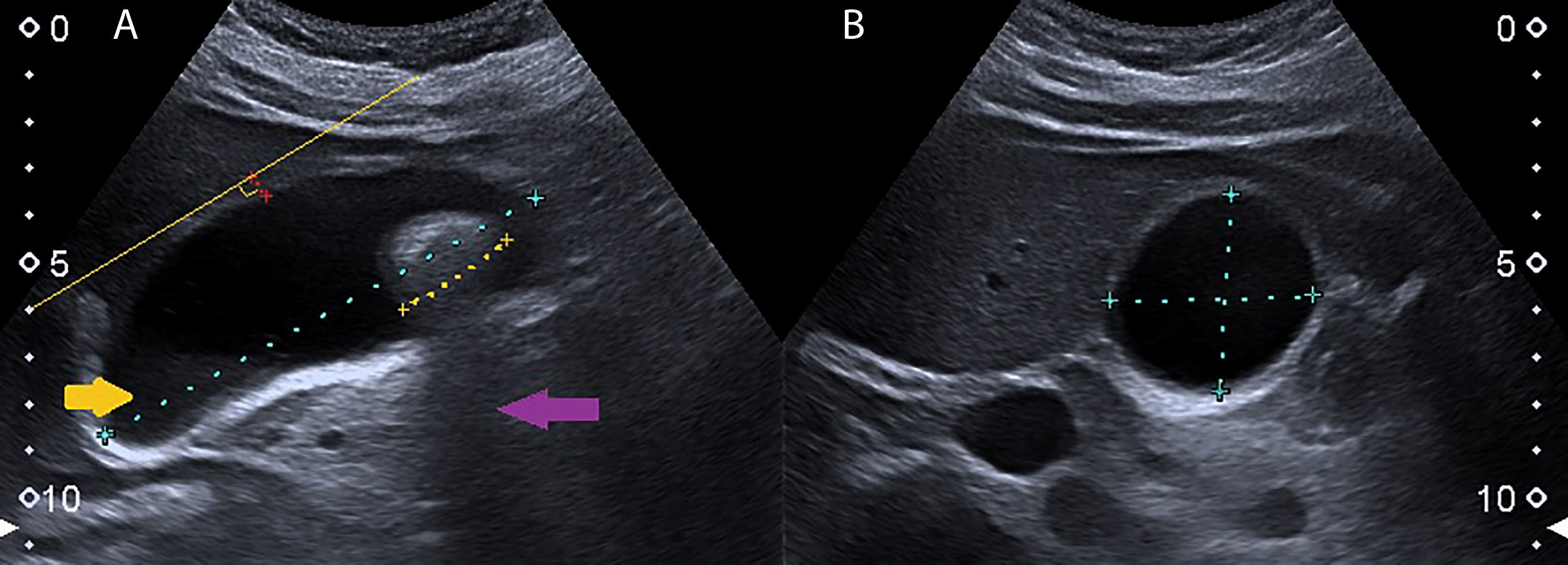
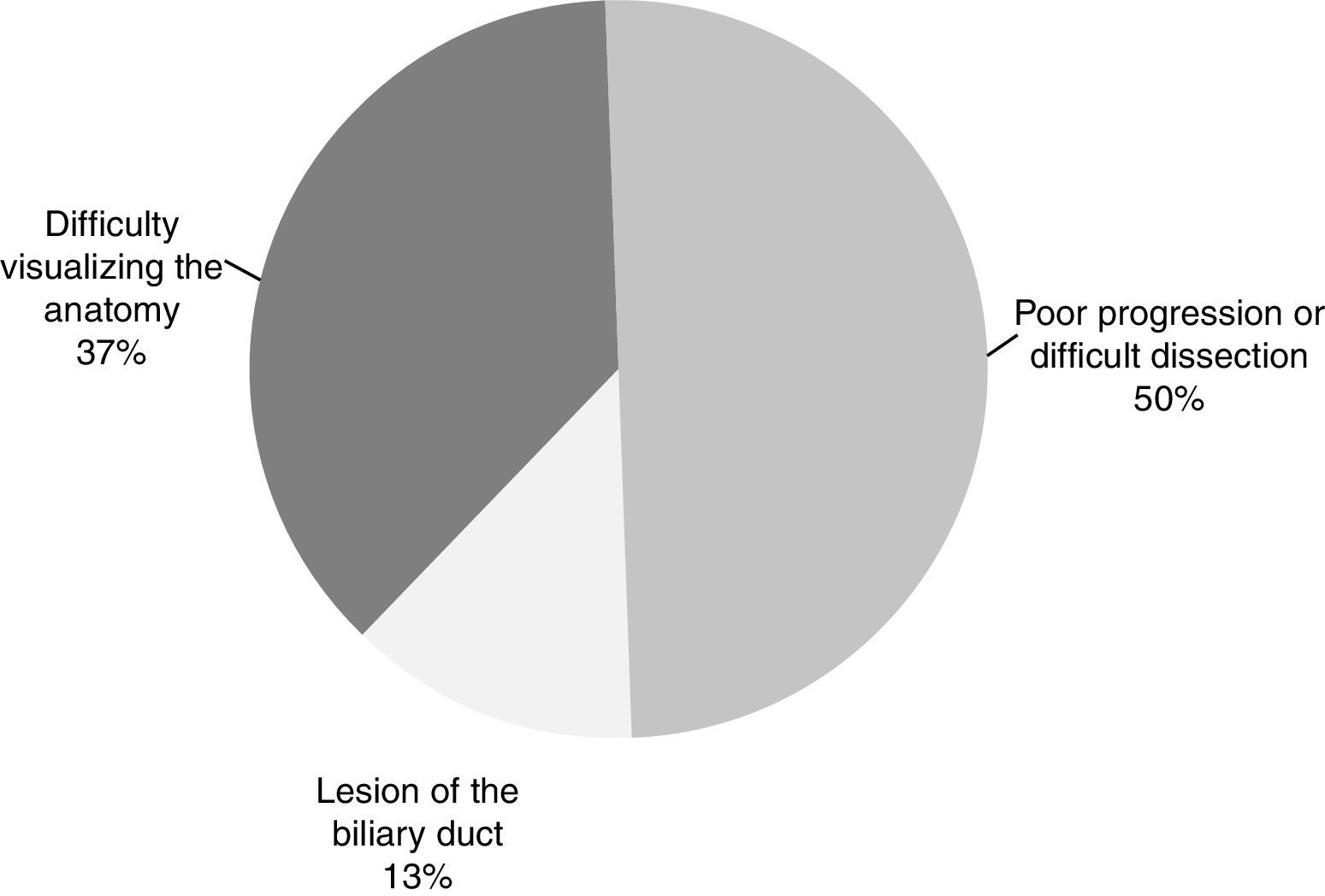
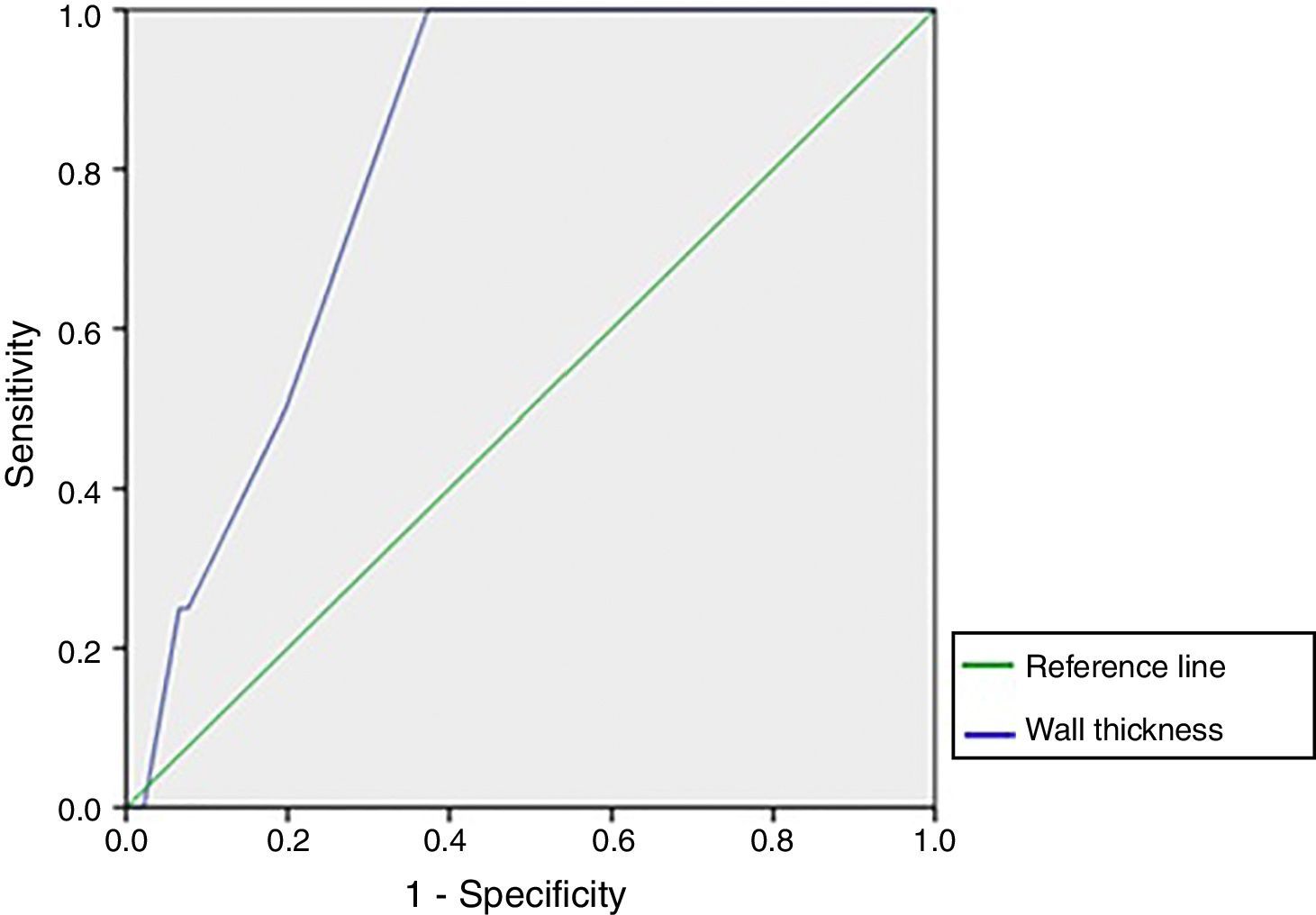
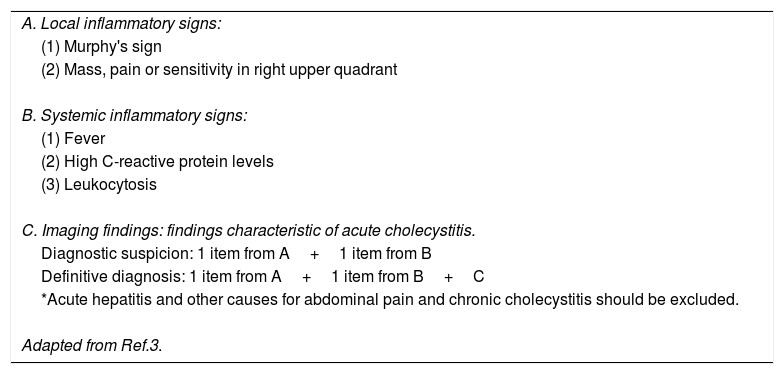
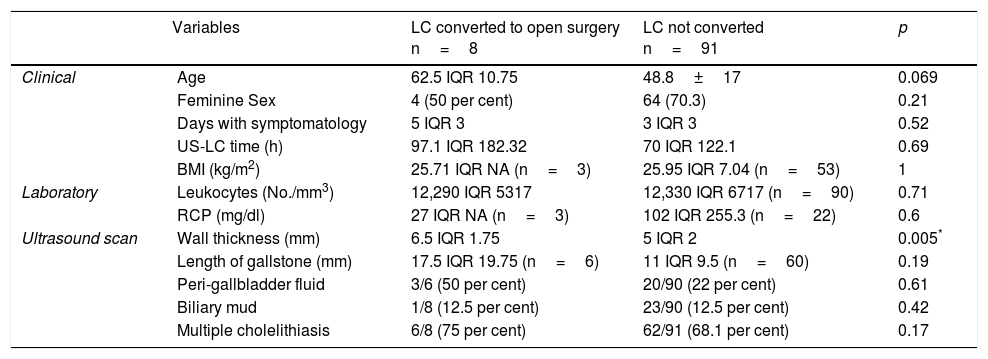
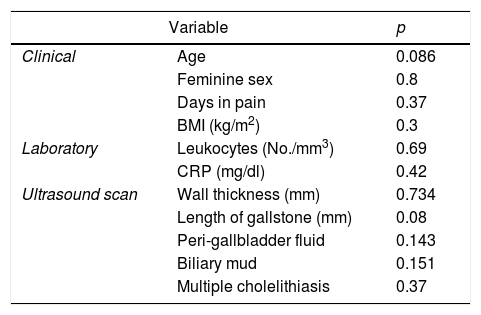
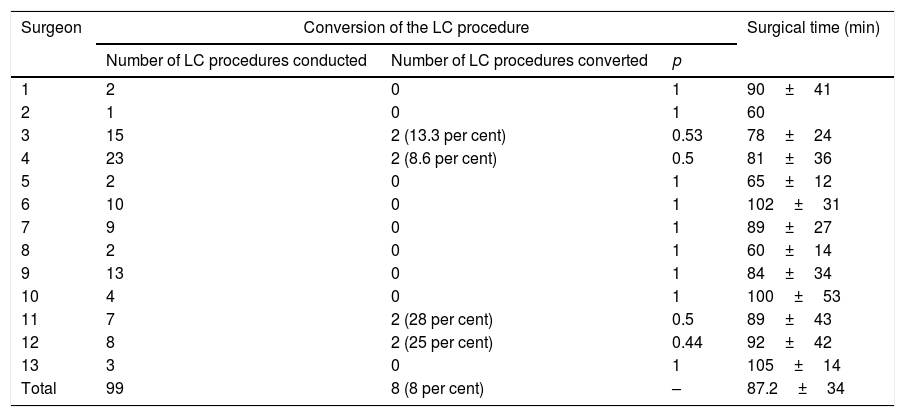
MethodWe developed a cross-sectional study that included 99 subjects older than 17 years with definitive diagnosis of AC who had undergone to LC. Preoperative variables such as clinical data, laboratory markers and ultrasound findings as wall thickness, the size of the major calculus and the presence of: perivesicular fluid, multiple cholelithiasis, biliary mud or microlithiasis were registered. We consider indirect measures of technical difficulties of LC the total surgical time and the need for conversion to open surgery. We used the square chi and Mann–Whitney U test to stablish the correlation between preoperative variables and the technical difficulties of LC. We build ROC curves of the variables with significant statistical association (p≤0.05 and 95% confidence interval) to determine the cut-off points of better sensitivity and specificity to predict conversion of LC to open surgery.
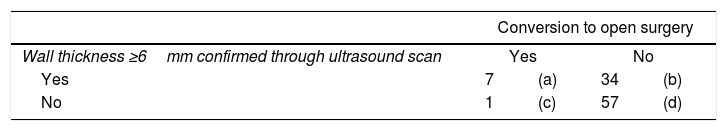
ResultsA gallbladder wall thickness ≥6mm detected by ultrasound has a sensitivity of 87.5% and a specificity of 62.6% with OR 11.71 (95%CI: 1.38–99; p=0.008) for predict conversion to open surgery. There was no relationship between surgical time and the preoperative evaluated variables.
ConclusionThe gallbladder wall thickness detected by the ultrasound is associated with the need of conversion of LC to open surgery in subjects with AC, furthermore this finding could warn the surgeon on the complexity with a particular patient.
Identificar en pacientes con colecistitis aguda (CoA) los factores preoperatorios asociados con el tiempo quirúrgico y con la conversión de colecistectomía laparoscópica (CL) a cirugía abierta.
MétodoSe realizó un estudio transversal que incluyó 99 pacientes mayores de 17 años con diagnóstico definitivo de CoA tratados con CL. Se registraron variables prequirúrgicas, como datos clínicos, valores de laboratorio y hallazgos ecográficos como el grosor de la pared de la vesícula, el volumen vesicular y la presencia de: líquido perivesicular, colelitiasis múltiple o barro biliar. Se consideraron medidas indirectas de dificultad técnica de la CL, el tiempo quirúrgico empleado y la necesidad de conversión a cirugía abierta. Se utilizaron las pruebas de ji-cuadrado o U de Mann-Whitney para establecer la relación entre las variables prequirúrgicas y aquellas indicativas de dificultad técnica. Se construyeron curvas ROC (Receiver Operating Characteristic) de las variables con asociación estadística significativa (p ≤0,05 e intervalo de confianza del 95%) para determinar los puntos de corte de mejor rendimiento para predecir la conversión de CL a cirugía abierta.
ResultadosUn grosor de la pared vesicular ≥6mm detectado por ultrasonido tiene una odds ratio de 11,71 (IC95%: 1,38-99; p=0,008), con una sensibilidad del 87,5% y una especificidad del 62,6% para predecir la conversión a cirugía abierta. No hubo relación entre el tiempo quirúrgico y las variables prequirúrgicas evaluadas.
ConclusiónEl grosor de la pared de la vesícula biliar detectado por ultrasonido se asocia con la necesidad de conversión de la CL a cirugía abierta en pacientes con CoA.
Artículo
Comprando el artículo el PDF del mismo podrá ser descargado
Precio 19,34 €
Comprar ahora