Traumatic injuries are the leading cause of death in people aged<45 years, and abdominal trauma is a source of significant morbidity and mortality and high economic costs. Imaging has a fundamental role in abdominal trauma, where CT is a fundamental tool for rapid, accurate diagnosis that will be key for patients’ clinical outcomes.
La patología traumática en general constituye la primera causa de muerte en menores de 45 años y el traumatismo abdominal en particular una fuente de importante morbimortalidad y elevados costes económicos.
La radiología tiene un papel fundamental en este proceso en el que el diagnóstico rápido y preciso con la tomografía computarizada como herramienta fundamental va a ser clave en la evolución clínica de los pacientes.
Traumatic injuries continue to be the leading cause of death in people under the age of 45.1–3 Because the effects of trauma on the body are random and it can affect different organs and systems, an overall assessment of the patient must be performed. Patients with multiple trauma require a rapid and accurate diagnosis focusing on the situations that may be imminently life-threatening.4
In this article, we focus on blunt abdominal trauma, which is much more common in our setting.1
AetiopathogenesisUp to 75% of abdominal injuries are due to road traffic accidents or falls from a height.1
Intra-abdominal injuries are the result of different, possibly co-existing, pathophysiological mechanisms, including5:
- -
Crushing: direct collision of abdominal structures against the spine or other fixed structures. Often the cause of solid visceral lesions.
- -
Compression: the sudden increase in intra-abdominal pressure can cause a rupture of hollow viscera.
- -
Deceleration: this causes shearing forces that damage the anchorage points of hollow and solid viscera, as well as vascular structures.
The Advanced Trauma Life Support guidelines (ATLS®), developed by the American College of Surgeons, are based on a primary survey (ABCDE) and a secondary survey.3,6 In the primary survey, only plain X-rays of the chest, pelvis and cervical spine are considered together with Focused Assessment with Sonography for Trauma (FAST) ultrasound, reserving computed tomography (CT) for the secondary survey in stable patients.6 However, these recommendations run counter to the current trend of incorporating CT scanners into critical care areas, and so being able to perform CT whenever the clinical situation allows.
The effectiveness of plain X-rays for detecting abdominal trauma injuries is poor. Ultrasound is an accessible, fast, non-invasive tool that can be performed at the bedside, which is why it has replaced diagnostic peritoneal lavage as technique of choice for the detection of peritoneal fluid.7,8 The most widely used protocol is FAST, which consists of examining the right flank, the left flank, the pelvis and the subxiphoid area (to rule out pericardial effusion). The extended version (E-FAST) also examines the chest for pleural effusion or pneumothorax.
According to the ATLS® guidelines, the presence of free fluid in unstable patients corresponds to intra-abdominal haemorrhage and is an indication for emergency laparotomy.6 However, there are situations in which there may be fluid but not caused by trauma, for example, in women of childbearing potential, in ascites or in patients treated with intensive fluid therapy.9 Ultrasound has low sensitivity for detecting visceral injuries and it does not identify bleeding foci. For these reasons, it would not be indicated in stable patients.
In order to overcome the limitations of ultrasound, certain centres have tried introducing contrast-enhanced ultrasound (CEUS) to assess abdominal traumatic injuries. Recent studies show a sensitivity of 79% in the detection of spleen and liver injuries, and a positive predictive value of 100%. However, these values drop sharply for the detection of retroperitoneal injuries and active bleeding foci, added to the limitations of ultrasound for assessing multisystem injuries in the context of patients with major multiple trauma. It could be a useful technique for assessing mild trauma with no suspected extra-abdominal injuries or instability criteria, for assessing the paediatric population and in the follow-up of traumatic injuries initially identified by CT.10
The limited availability, poor accessibility and the time the scans take to complete make magnetic resonance imaging an inappropriate technique for assessing patients with multiple trauma.11
The diagnosis of injuries is based almost exclusively on CT images. It is a fast, accessible technique with a sensitivity of 97% and specificity of 99% for the detection of significant abdominal injuries.2,12
ProtocolThe protocols used vary greatly. Both in view of the limited effectiveness and to avoid unnecessary radiation, performing a non-contrast phase is not recommended. Of the post-contrast phases, the venous phase is a definite requirement, in order to characterise visceral injuries and to identify any bleeding. The arterial phase is recommended to characterise bleeding, diagnose vascular injuries and plan possible intravascular treatment. If there is any injury to the urinary tract, and whenever possible, the scan should be completed by a renal elimination phase after 3−5min.13
Scanning the same anatomical region in arterial and venous phases obviously means more radiation. To avoid this, “split bolus” techniques have been proposed, in which two or three boluses of contrast are administered with pauses (serum boluses) in between, so that a dual phase (arterial and venous) or even a triple phase (arterial, venous and elimination) is obtained in a single acquisition. One of the potential drawbacks of these protocols is decreased sensitivity for detecting spleen and liver vascular injuries, and those in the neck and pelvis.14–16
Classification of traumatic injuriesSolid abdominal organs can suffer two types of injury: parenchymal and vascular.17
- 1
Parenchymal lesions:
- -
Laceration: hypodense lesions of linear morphology. The worst case is a shattered spleen. They tend to involve a capsule tear, which is why they frequently also have haemoperitoneum.
- -
Haematoma: poorly defined hypodense area. If they are peripheral and the capsule is preserved, subcapsular haematomas can form: collections with defined borders which and obtuse angles with respect to the parenchyma.
- -
Contusion: hypodense focus with poorly defined borders due to the presence of oedema or haemorrhage secondary to damage to small capillaries.
- -
Infarction: absence of enhancement due to interruption of the vascular supply.
- -
- 2
Vascular injuries:
- -
Contained vascular injury: rounded lesions that behave similarly to the vessel on which they depend, are hyperdense in the arterial phase, sometimes becoming isodense with the parenchyma in the venous phase, which is why an arterial phase is necessary for diagnosis. These are pseudoaneurysms and arteriovenous fistulas (AVF), often indistinguishable by CT, except on occasion, when a draining vein is seen with early enhancement, indicative of AVF.
- -
Non-contained vascular injury or active bleeding: accumulation of extravascular contrast with formation of a hyperdense collection in the arterial phase that increases in size and remains hyperdense in subsequent phases. Bleeding can be free into the peritoneum or exclusively intraparenchymal, which has a better prognosis. It is important to perform an arterial phase to try to identify the origin of the bleeding.
- -
- -
Haemoperitoneum: usually secondary to solid visceral injuries with capsular involvement. Blood close to the point of origin of the bleeding usually has higher densitometric values (45–70 HU), giving rise to the sentinel clot sign.18
- -
Pneumoperitoneum/pneumoretroperitoneum: common finding in open abdominal trauma. In blunt abdominal trauma it usually indicates a hollow viscus injury.
It is important to distinguish it from pseudopneumoperitoneum, in which free gas is seen between the abdominal wall and the parietal peritoneum. It is usually secondary to rib fractures, pneumothorax, pneumomediastinum or even extraperitoneal rectal injuries.19
- -
Abdominal wall injuries: an important marker of an intra-abdominal injury, as they are the consequence of high-energy impacts. Very typical is contusion of the anterior abdominal wall caused by the seat belt in road traffic accidents (seat belt sign).20
- -
Injuries to the wall are usually mild and consist of contusions/haematomas in the subcutaneous cellular tissue and small fibrillar tears or intramuscular haematomas (generally affecting the rectus abdominis). Where bleeding is detected within the rectus abdominis muscle, it will generally be dependent on the inferior epigastric artery, and if the bleeding affects the lateral wall, it corresponds to the territory of the deep circumflex iliac artery.
- -
Traumatic hernias are rare and the most common are lumbar hernias, with protrusion of abdominal structures through the inferior lumbar (Petit's) triangle. They are often underdiagnosed and in up to 25% of cases present as late complications when the hernia becomes strangulated or incarcerated.21
Highly vascular organ with a fragile capsule, which is why it is frequently injured in abdominal trauma.
The American Association for the Surgery of Trauma (AAST) classification categorises imaging findings into grades I–V from least to most severe (Fig. 1); the most severe findings (grade V) being shattered spleen or active bleeding into the peritoneal cavity.22
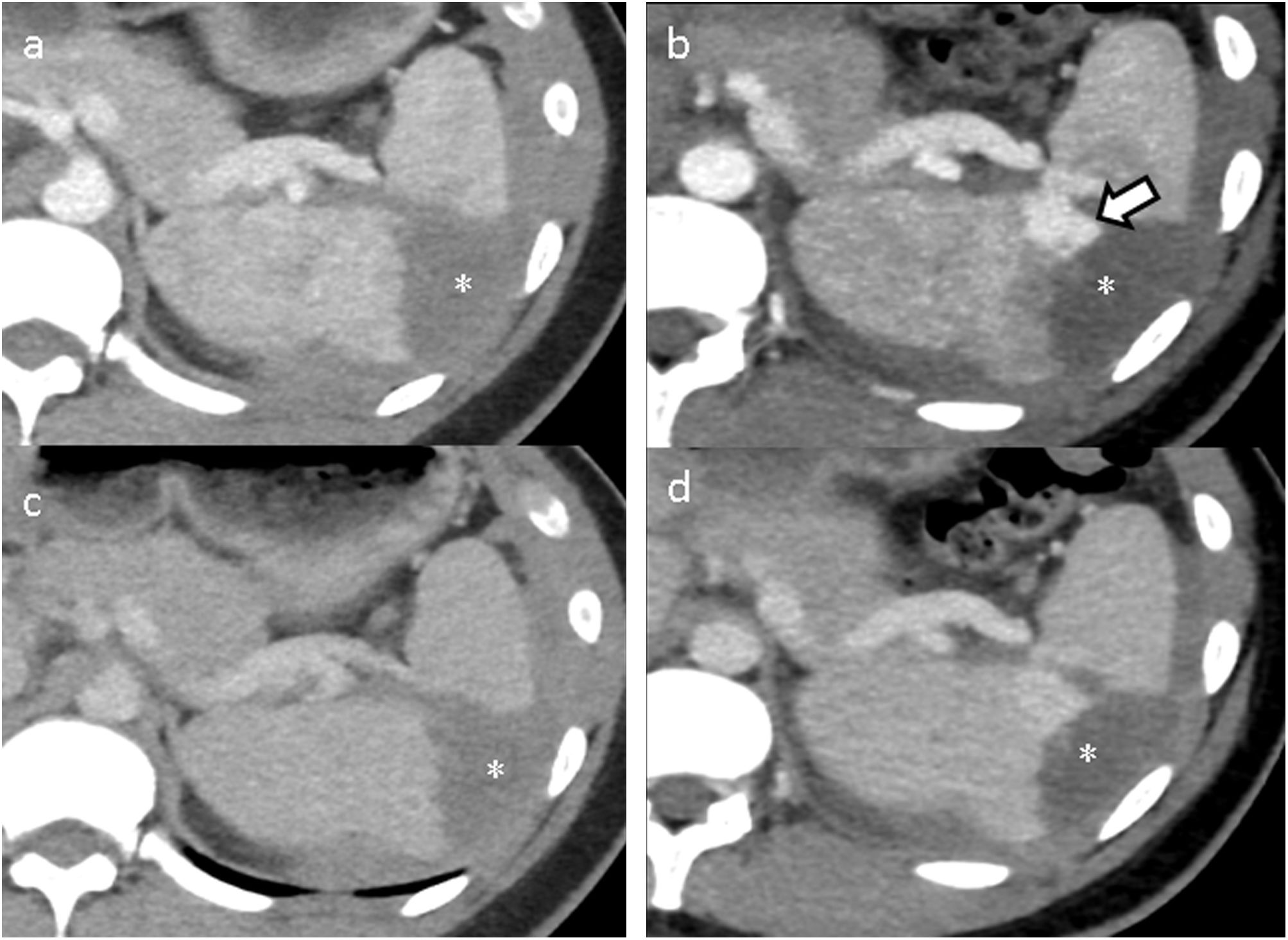
CT has a very high sensitivity for the detection of traumatic spleen injuries. Vascular injuries are much better visualised in the arterial phase, mainly helping to detect contained vascular injuries (Fig. 2).23 The venous phase facilitates not only the detection of parenchymal lesions, but also the confirmation of bleeding, by giving more time for the contrast to leak out.
CT of abdomen in arterial (a) and venous (c) phases showing a spleen haematoma (asterisk). In the follow-up CT at 48h in the arterial (b) and venous (d) phases, a newly appearing pseudoaneurysm (arrow) was identified, practically indistinguishable in venous phase (d) as the lesion was isodense with the splenic parenchyma.
The most common errors tend to be due to the analysis of the parenchyma in the arterial phase, in which the typical pattern of “striped” enhancement can simulate lacerations, and to the existence of clefts, linear and peripheral images, consequence of incomplete fusion of the splenic lobulation, which can simulate a laceration.17 Lacerations tend to be irregular, less well defined, and form more acute angles with the capsule. On occasion, splenic cysts and haemangiomas can also be indistinguishable from haematomas, in which case the assessment of associated injuries (for example, rib fractures, haemoperitoneum) may be useful.
There is no consensus on treatment, although the general trend is towards conservative management. This consists of close monitoring, follow-up imaging and angiography with embolisation, whether urgent (for active bleeding) or elective (for contained vascular lesion). Some authors recommend embolisation of all high-grade (III–V) injuries, regardless of whether or not a vascular injury is visible on CT.24 Surgery should be reserved for patients with high-grade or haemodynamically unstable injuries.25 After embolisation it is common to see intrasplenic gas; if it increases, forms a level or is associated with collections or pneumoperitoneum, abscess formation should be suspected.
Splenic trauma is a dynamic process and it is therefore advisable to perform a follow-up CT in arterial and portal phase 24−48h after the initial CT in all patients with spleen injury. This helps detect new contained vascular injuries and improves the prognosis of patients treated conservatively, reducing the risk of delayed ruptures.26,27
LiverAlong with the spleen, the liver is one of the organs most frequently affected in abdominal trauma. There are many similarities with the spleen, but also a number of differences. The liver has a dual vascular supply, which means that arterial-portal and portal-venous fistulas can develop in addition to the classic arterial-venous fistulas. In addition, the liver has a bare area not covered by peritoneum, so extraparenchymal bleeding involving this area will cause retroperitoneal haematomas without haemoperitoneum, making it undetectable by FAST ultrasound.13 Lastly, the gallbladder and bile duct may be affected, usually in the case of high-grade lesions. Gallbladder injuries are difficult to identify on CT, where the signs would be a thickened, poorly defined wall and perivesicular fluid. It is unlikely we would be able to see a gallbladder wall defect. Bile duct injuries will lead to free fluid indistinguishable from haemoperitoneum, and some authors recommend scintigraphy or MRI with liver-specific contrast for diagnosis, with the MRI option being the most widely used in our setting.16,28,29
Parenchymal injuries must be assessed over parenchyma with homogeneous enhancement in a portal venous phase. As in the spleen, lacerations and haematomas may be seen. Lacerations are hypodense images with a more linear or branched pattern, while haematomas are less well-defined hypodense areas and may be subcapsular. Vascular injuries may also be found, either contained (pseudoaneurysms and fistulas, arterial-venous, arterial-portal or portal-venous) or not contained (active bleeding).30
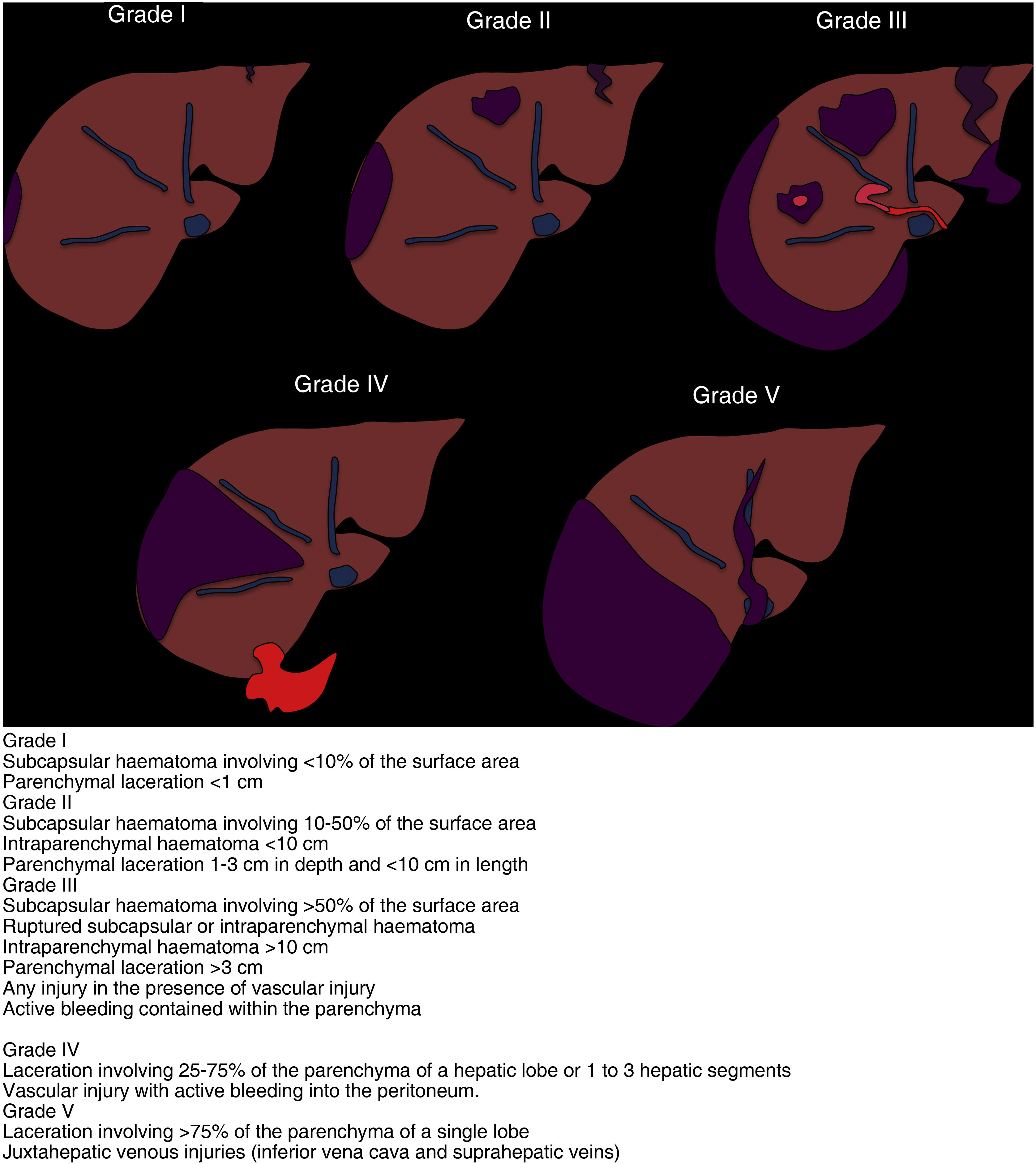
As with the spleen, the AAST published an update to the scoring scale in 2018 (Fig. 3) to include vascular injuries. They are divided into five grades, from minor to major severity, with grade V consisting of lacerations involving more than 75% of the parenchyma and injury to juxtahepatic veins (inferior vena cava and suprahepatic veins).22
On occasion, there may be uncertainty about the diagnosis in patients with hepatic steatosis, and areas of focal steatosis should not be confused with lacerations or haematomas. We should keep in mind the typical areas of fatty deposits in the perivesicular area and surrounding the falciform ligament. If diffuse periportal hypodensity is observed, it may indicate periportal oedema, but if it is focal, it may be related to a haematoma that crosses through the periportal space.31
The treatment is conservative whenever the patient's situation allows, and injuries of a vascular nature will be treated by embolisation. Routine follow-up imaging is not recommended unless clinical or laboratory tests suggest a complication.17
Bowel and mesenteryTraumatic bowel and mesenteric injury is more common in open trauma. In blunt trauma, it has classically been associated with abdominal wall injury and Chance fracture of vertebrae from seat belts, and is a result of high-energy mechanisms.
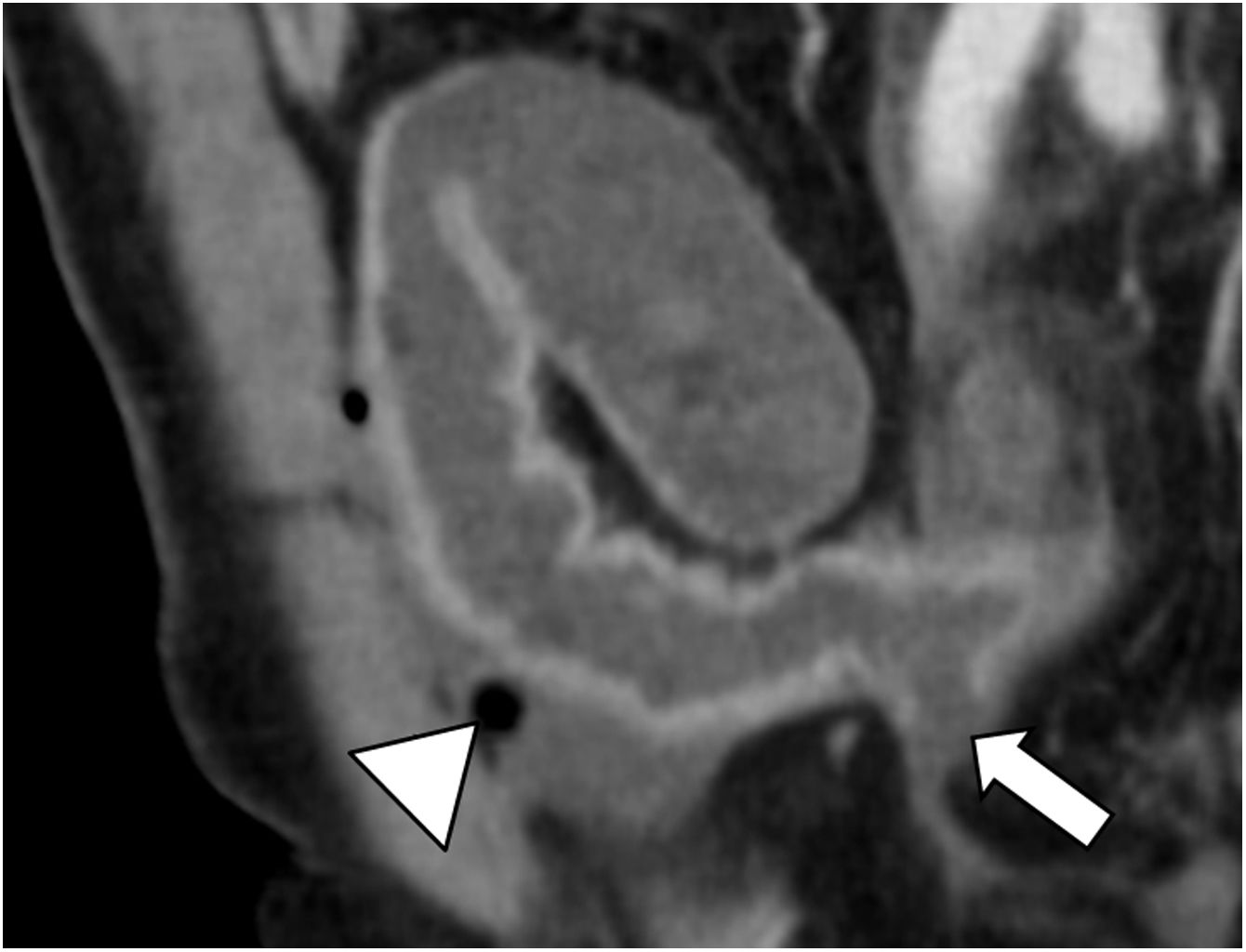
The most specific radiological findings are discontinuity of the bowel wall, the extravasation of enteric content and pneumoperitoneum (important to distinguish it from pseudopneumoperitoneum). Unfortunately, these are not very sensitive findings as it is generally not possible to visualise the bowel wall defect and with the majority of perforations there is no pneumoperitoneum. Both wall thickening and enhancement abnormalities are more sensitive findings. There may be loops with increased enhancement due to contusion or as a compensatory phenomenon due to ischaemia secondary to a mesenteric vascular injury (Fig. 4).
Oblique reconstruction of CT of abdomen-pelvis in venous phase after intravenous contrast administration. Image shows perforation (arrow) and pneumoperitoneum (arrowhead) as specific signs of traumatic bowel injury. A slight thickening and more diffuse mural hyperuptake can also be seen as a more sensitive sign of injury.
If intestinal involvement is diffuse with mural enhancement and mucosal thickening in a patient with hypotension, shock bowel should be considered rather than direct traumatic involvement.13,32,33
The findings in duodenal injury are similar to those described for bowel injury, but there are certain distinctions because of its anatomical relationships. It is important to remember that the first portion is the only part that is intraperitoneal, while the second contains the ampulla of Vater, so its involvement may mean a biliary injury. The presence of a submucosal haematoma is typical; this can even make gastric emptying difficult and is often associated with a pancreatic injury.34,35
The most specific findings of mesenteric injury are haematoma and vascular injury, which may result in active bleeding, pseudoaneurysm, occlusion or intimal injury. Other less specific findings are increased density of the mesentery, fat striation and the presence of peritoneal fluid.36
Treatment of these lesions is usually surgical due to the risk of peritonitis and sepsis. Some small mesenteric haematomas and focal thickening not suspected of being at risk of perforation can be treated conservatively, but with close monitoring.37
PancreasInjury to the pancreas is generally a result of direct trauma against a steering wheel or handlebars. The lesions become more evident in successive imaging tests where the contusions will show up as oedematous areas. Different injuries may involve contusions (hypodense areas), lacerations (linear hypodensities) or transection (full thickness laceration).13,38
Urinary systemThe kidneys are well protected in the retroperitoneum immersed in the fat inside the renal fascia, with the renal pelvis and the vascular pedicle as the only anchorage points. This makes them particularly sensitive to acceleration/deceleration forces, which cause injuries at the ureteropelvic junction or intimal injuries in the arteries or veins, which can go on to cause thrombosis of the vessel.39
The only sign of a possible urinary injury is haematuria and the severity is not dictated by the amount of blood; in fact, in some of the most severe injuries (pedicle injury or ureteropelvic junction avulsion) there may not be haematuria. There are significant limitations with ultrasound as, because the kidneys are retroperitoneal, patients will not have free intraperitoneal fluid, and the sensitivity of CEUS for detecting urinary tract injuries is also low.40 The technique of choice is therefore CT in arterial and portal phases, performing an excretory phase after 5−10min if urinary tract injury is suspected. Most injuries to the urinary tract occur at the level of the kidneys due to lacerations involving the collecting system, but it is not uncommon for the ureteropelvic junction to be affected. In such cases, it is important to identify whether the injury is partial, in which case dye can be seen in the ureter distal to the injury, or complete, where there is no dye in the distal ureter (Fig. 5).13,17,39
Coronal reconstruction in the elimination phase showing extravasation of contrast in both renal pelvises suggestive of bilateral ureteropelvic avulsion. The presence of staining in the left distal ureter (arrow) would prompt endourological treatment to be considered, as it would indicate a partial injury, while the right injury probably requires a surgical approach as it is a complete injury.
As with the classifications of liver and spleen injuries, the latest update of the AAST severity scale includes vascular injuries (Fig. 6). The most severe injuries, grade V, are laceration of the vascular hilum, shattered kidney or devascularisation with bleeding.22
Treatment is generally conservative, except in complete injury of the ureteropelvic junction, when surgery will be required. Barring clinical deterioration, routine follow-up imaging of kidney injuries is not generally recommended.39,41
Bladder rupture is usually secondary to complex fractures of the pelvic ring and is generally extraperitoneal (90%). Treatment of these ruptures is conservative, unlike intraperitoneal ruptures, which will generally require surgical repair. For accurate diagnosis, a CT cystogram will very often be necessary with retrograde distension of the bladder by injecting iodinated contrast diluted to 10% through a catheter.13
Conclusions- -
The widespread use of CT and the implementation of new protocols have made it possible for patients with multiple trauma to be managed increasingly conservatively.
- -
This is feasible largely thanks to the endovascular treatment of vascular lesions.
- -
Abdominal trauma will have general findings along with certain features particular to each organ. We need to be familiar with these in order to alert the surgeon to the minority of injuries that are going to require urgent surgical management.
- 1
Responsible for the integrity of the study: GA and JC.
- 2
Study conception: GA and JC.
- 3
Study design: JC and GA.
- 4
Data collection: GA and JC.
- 5
Data analysis and interpretation: GA and JC.
- 6
Statistical processing: not applicable.
- 7
Literature search: JC and GA.
- 8
Drafting of the article: JC and GA.
- 9
Critical review of the manuscript with intellectually relevant contributions: JC, GA, VG, AU and PR.
- 10
Approval of the final version: JC, GA, VG, AU, PR and JC.
The authors declare that they have no conflicts of interest.