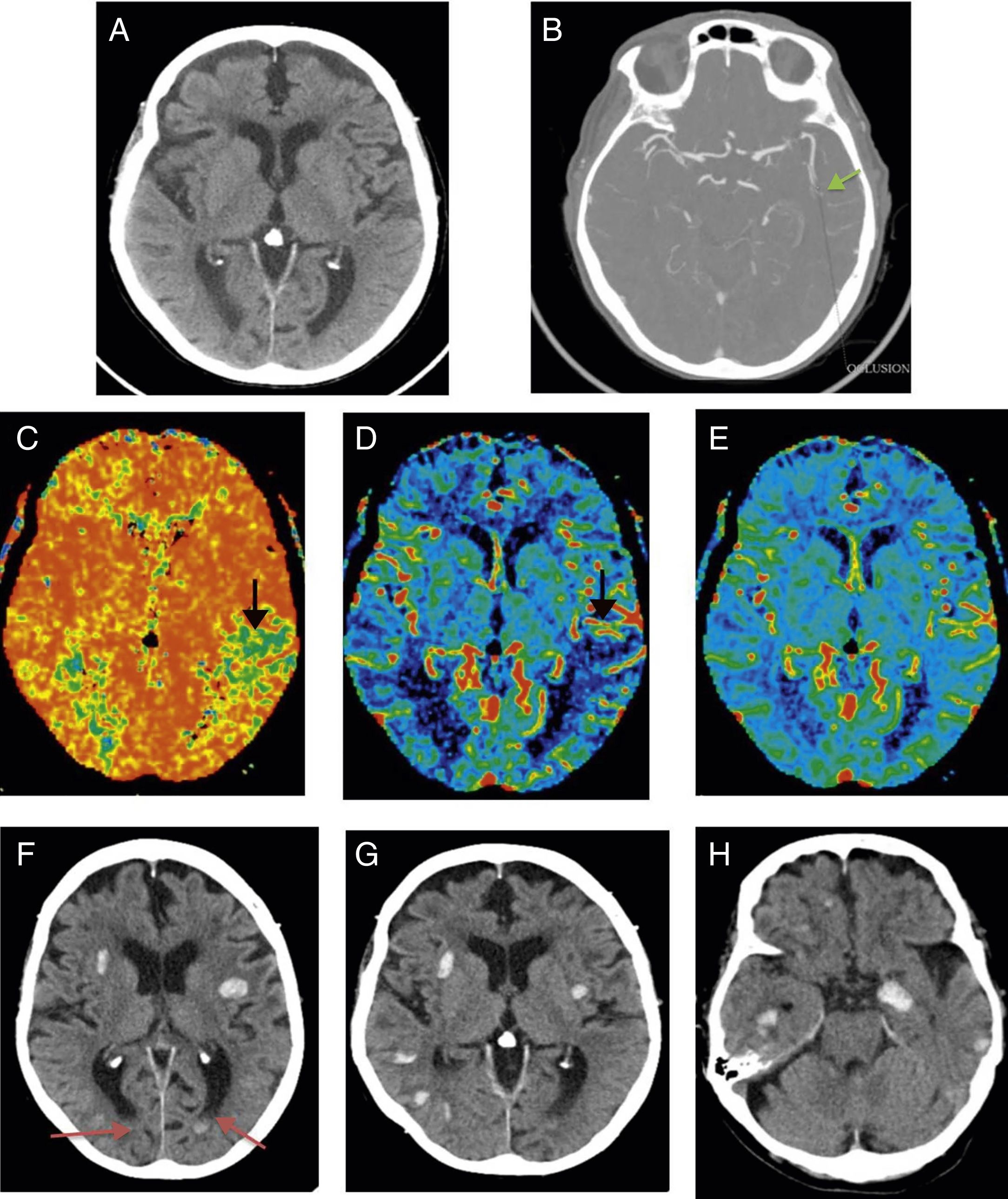
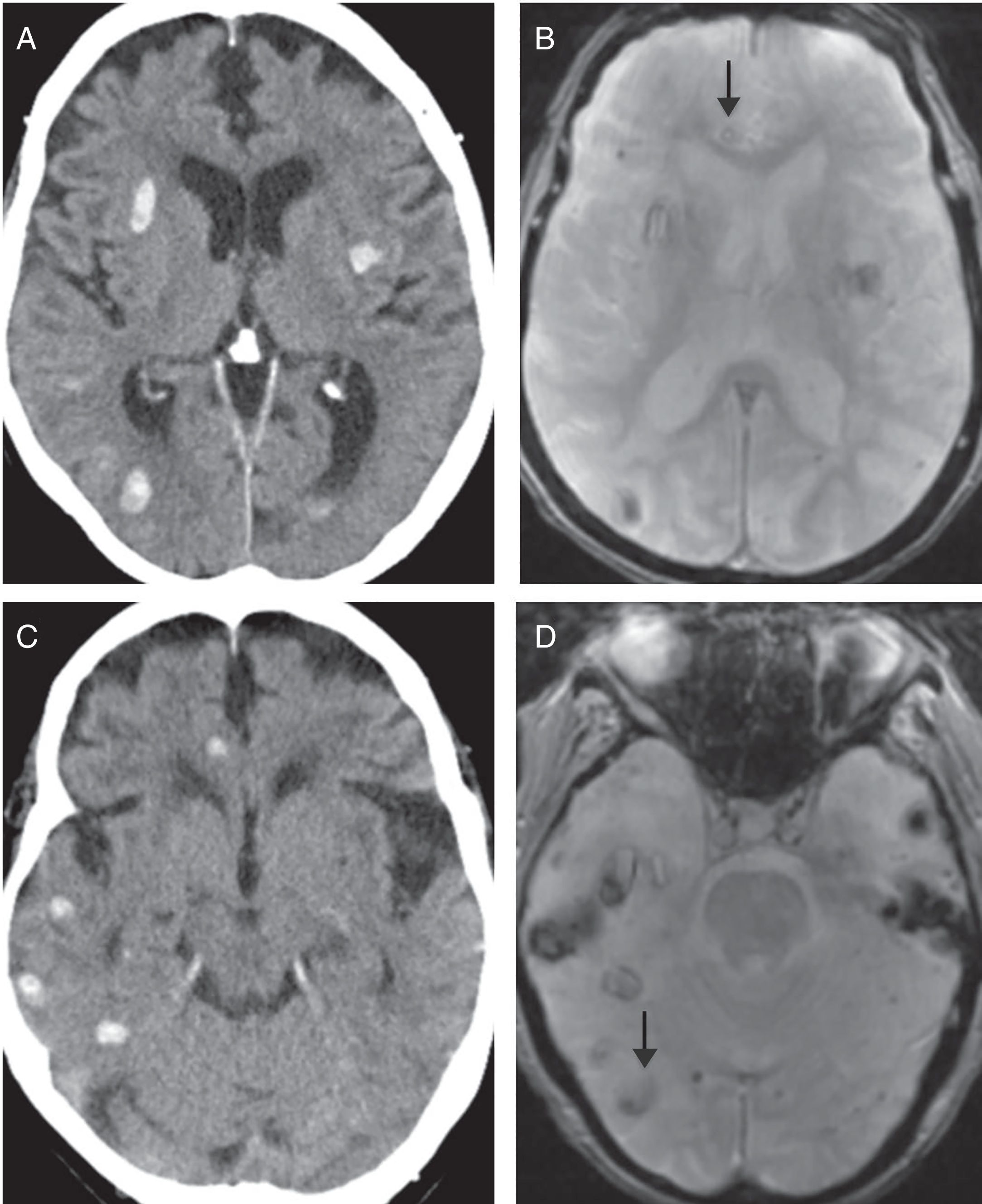
We present the case of a 90-year-old woman with a history of left carotid transient ischaemic attack and mild aortic stenosis. She attended the emergency department with motor aphasia of unknown onset. A National Institutes of Health stroke scale (NIHSS) score of 5 was obtained on physical examination. The stroke code was activated and brain computed tomography (CT), cerebral perfusion CT and CT angiography of the supra-aortic arteries and circle of Willis were performed, which revealed a baseline Alberta Stroke Program Early CT score (ASPECTS) of 10, an area of ischaemic penumbra in the territory of the left middle cerebral artery and a thrombus in the ipsilateral distal M2 segment (Fig. 1A–E). Despite the patient's advanced age, and given her good quality of life prior to the imaging findings, fibrinolytic therapy was initiated. Twenty-four hours after treatment, the patients neurological status had deteriorated. A follow-up brain CT scan was requested, which showed multiple foci of lobar and diffuse intraparenchymal haemorrhage (Fig. 1F–H). The distribution of haemorrhagic foci distant from the territory affected by the penumbra area ruled out haemorrhagic transformation. Suspecting amyloid angiopathy (AA), a magnetic resonance imaging (MRI) scan was requested as a complementary test. The MRI, based on the Boston criteria, supported the diagnosis of “probable” AA by showing multiple foci of old bleeding in the T2 gradient echo sequence (Fig. 2). Mixed dysphasia persisted at discharge.
(A–E) Pretreatment studies. Computed tomography (CT) of the brain without contrast (A), CT angiography of circle of Willis (B) and cerebral perfusion study (C–E) performed due to suspicion of ischaemic stroke. (A) The baseline CT shows no signs of acute ischaemia (ASPECTS 10). (B) In the CT angiography of the circle of Willis, an obstruction is observed in the left M2 segment, suggestive of a thrombus. (C) Increased mean transit time (arrow) visible on perfusion maps. (D) Decreased blood flow (arrow). (E) Normal volume, no change from perfusion study. The aforementioned abnormalities are located in the left parietal region, left middle cerebral artery territory, and are suggestive of penumbra. (F–H) Brain CT without contrast, axial slices, performed 24h after the start of fibrinolytic treatment. Multiple foci of diffuse cortical, lobar, and predominantly supratentorial bilateral bleeds can be seen remote from the area of ischaemia. The deep grey nuclei are spared. The radiological findings described are suggestive of amyloid angiopathy. Blood levels in left occipital ventricular horns (arrows in panel F).
Comparative study of magnetic resonance imaging (MRI) of the brain (gradient echo sequence) and computed tomography (CT) of the brain without intravenous contrast. Due to the different settings and the different slice thickness used in the CT and MRI studies (the orbitomeatal line is used in CT and the subcallosal line in MRI), the topography of the images obtained does not completely match. The images can be compared by taking as a reference the frontal ventricular horns in (A), (B) and the posterior fossa in (C) and (D). The arrows indicate old haemorrhage foci visible in gradient sequence MRI, but not in CT. These findings support the diagnosis of amyloid angiopathy according to the Boston criteria.
Haemorrhagic transformation of cerebral ischaemia is a common complication after fibrinolytic treatment, and occurs in 5.8%1 of cases. The main risk factors are advanced age, high blood pressure and low body weight. However, a less discussed complication that increases morbidity in these patients is remote intracerebral haemorrhage.2 This type of complication occurs in 1.3–3.7% of cases.3 Studies suggest two possible associations that could explain the underlying cause of this type of bleeding, according to location. The first is the association between deep haemorrhage and arterial hypertension, and the second between lobar bleeding and previous microbleeds that would act as markers of underlying small vessel pathology (AA).3
AA is caused by the accumulation of β-amyloid protein in small and medium vessels, giving rise to greater vascular fragility. Ageing is the main risk factor, and AA is more common in the elderly,4 in whom the incidence of cerebral ischaemia is also higher. The main radiological manifestation of AA according to the Boston criteria is the presence of acute/chronic cortical and/or corticosubcortical haemorrhages.4 The differential diagnosis must take into account other pathologies that can cause cerebral bleeding, such as hypertension, multiple cavernomatous malformations and previous brain injury. Diagnosis of exclusion is therefore indicated. It is important to note that the characteristic distribution with respect to deep grey nuclei and the brainstem can distinguish AA from haemorrhage secondary to hypertension.4
As already mentioned, studies have suggested a possible association between amyloid angiopathy and post-treatment remote intracerebral haemorrhage.2,3 Because microbleeds, visible on MRI, can act as concomitant AA markers, the performance of a brain MRI before the start of treatment would predict the risk of post-treatment bleeding5 and would facilitate selection of candidates for fibrinolytic treatment. However, there is still insufficient evidence to support this hypothesis and justify it as a contraindication for treating a serious and prevalent condition such as ischaemic stroke.3
This is why it is so important to continue to design studies to determine the usefulness of MRI in assessing the association between prior microbleeds, post-fibrinolysis bleeding and patient outcomes.
Please cite this article as: Sigüenza González R, Gómez San Martín E. Angiopatía amiloide como causa de “hemorragia intracraneal remota” en paciente tratado mediante fibrinólisis. Radiología. 2019;61:266–268.