The use of general anesthesia in infants involves both short-term and long-term risks. The aim of this study is to evaluate the efficacy of brain MRI without anesthesia in infants younger than 3-month-old immobilized with a pillow.
Patients and methodsThis prospective case-control study was done in 2019. Cases were stable patients less than 3 months old who did not require ventilatory support for whom brain MRI was indicated. Patients were fed so they would fall asleep and placed in the scanner with an immobilizing pillow. Controls were clinically unstable patients matched for age and sex referred for brain MRI under general anesthesia. Three pediatric radiologists evaluated the success of the MRI study (whether it answered the clinical question), recorded whether it was necessary to repeat the study, and rated the presence of motion artifacts on a scale ranging from 1 to 4.
ResultsA total of 47 cases were included (28 boys and 19 girls; mean age, 31 days). Of these, 42 (89%) MRI studies were considered successful. The proportion of successful MRI studies was lower in outpatients than in inpatients (p = 0.02). The quality of MRI in cases was considered optimal in 60% and suboptimal (motion artifacts in one or two sequences) in 30%. No safety issues related with the technique were detected. The mean duration of the studies was 16.6 min (range, 6–30 min). All of the MRI studies in controls were considered successful; quality was considered optimal in 89% and suboptimal in 11%. In the first year in which we used this technique, we avoided the use of general anesthesia in 47 MRI studies in 42 newborns.
ConclusionBrain MRI using the feed and sleep technique in infants younger than 3-month-old immobilized with a pillow can be done safely and efficaciously without general anesthesia.
El uso de anestesia general en niños pequeños conlleva riesgos, a corto y largo plazo. El objetivo de este estudio fue evaluar la eficacia de la técnica de resonancia magnética (RM) cerebral sin anestesia mediante fijación con colchón en niños menores de 3 meses.
Pacientes y métodosEstudio prospectivo de casos y controles realizado en el año 2019. Los casos fueron pacientes menores de 3 meses con indicación de RM craneal, estables y sin soporte ventilatorio; las resonancias se realizaron usando la técnica de dar de comer y dormir y un colchón inmovilizador. Los controles fueron pacientes de la misma edad y sexo, inestables clínicamente, derivados para realizar RM craneal con anestesia general. Tres radiólogos pediátricos evaluaron el éxito de la RM (si respondía a la pregunta clínica), si era necesario repetirla y calificaron la presencia de artefactos de movimiento en una escala del 1 al 4.
Resultados47 casos fueron incluidos en este estudio (28 niños, 19 niñas; media: 31 días de vida), de los cuales (89%) 42 RM fueron llevadas a cabo de manera exitosa. Los estudios realizados de manera ambulatoria se asociaron a mayor posibilidad de fallo de la técnica que los realizados a ingresados (valor de p 0,02). El 60% de las RM de los casos realizados tuvieron calidad óptima y el 30%, subóptima (artefacto de movimiento en una o dos secuencias). No se detectaron problemas de seguridad con esta técnica. La media de duración de los estudios fue de 16,6 minutos (rango 6-30 minutos). El 100% de las RM de los controles bajo anestesia general se llevaron a cabo con éxito, con una calidad óptima en el 89% y subóptima en el 11% restante. En el primer año de experiencia con esta técnica, de 47 RM realizadas, se evitó el uso de anestesia general a 42 recién nacidos.
ConclusiónLa técnica de dar de comer y dormir y fijación con colchón neumático para realizar RM sin anestesia puede realizarse de forma eficaz y segura en niños menores de 3 meses.
Magnetic resonance imaging (MRI) of the head is the most sensitive imaging technique for detecting ischaemia, haemorrhage and central nervous system malformations in children under one year of age.1 MRI requires the patient to be immobile for a period of 15–45 min; therefore, it has traditionally been performed with general anaesthesia. The use of general anaesthesia is associated with immediate risks due to possible airway depression or anaphylaxis,2,3 and in the first few years of life it has also been linked to higher rates of developmental delays, learning difficulties and attention disorders.4,5 This relationship between neurotoxicity and general anaesthesia in small children is the subject of great debate.6–9 However, according to the “as low as reasonably achievable” (ALARA) principle, there is a general consensus that it is advisable to make every effort to avoid the use of general anaesthesia in children under 3 years of age.6–9 Several studies have shown the usefulness of the technique of “feed and sleep” and/or immobilisation with an air mattress to reduce numbers of MRIs requiring general anaesthesia.10–14 The objective of this study was to evaluate the efficacy and safety of this technique for performing a head MRI in children under 3 months of age at our centre and to determine the factors associated with the technique’s failure.
Patients and methodsThis was a prospective case/control study conducted in 2019. It did not require the approval of an ethics committee or informed consent from the patients’ parents or legal guardians as the studies were necessary for the clinical management of the patients. A case/control design was used to confirm that the quality of the technique of the studies included as cases was suitable compared to controls of the same age performed with general anaesthesia. The patients enrolled as cases in this study were referred to the paediatric radiology unit for an MRI of the head. They were clinically stable with no airway problems. The order for these MRI studies indicated a wish that they be performed without anaesthesia, using the “mattress” method. The controls were clinically stable patients of a similar age and sex for whom a head MRI under general anaesthesia was ordered. The neonatologists independently determined the indication for MRI and whether the patients required general anaesthesia (controls) or did not require general anaesthesia (cases) for the MRIs depending on the patients' clinical condition.
The technique of “feed and sleep” and immobilisation with an air mattress required the patient to fast for approximately 2–3 h before the MRI. Nurses and radiology technicians with experience with paediatric patients performed all the procedures. A physician (neonatologist or paediatrics resident) and a neonatology nurse were also present when the patients were admitted to the neonatology unit or neonatal intensive care unit. Feeding was in the neonatology department for inpatients and in the radiology department for outpatients. Light and noise were minimised in the preparation room and in the MRI room. Following feeding, the patients were given earplugs (prepared by our nursing staff with cotton), MRI helmets and a sleeping mask like those used in light therapy to isolate them acoustically and visually. Dummies were given to infants who wanted them and which calmed them.
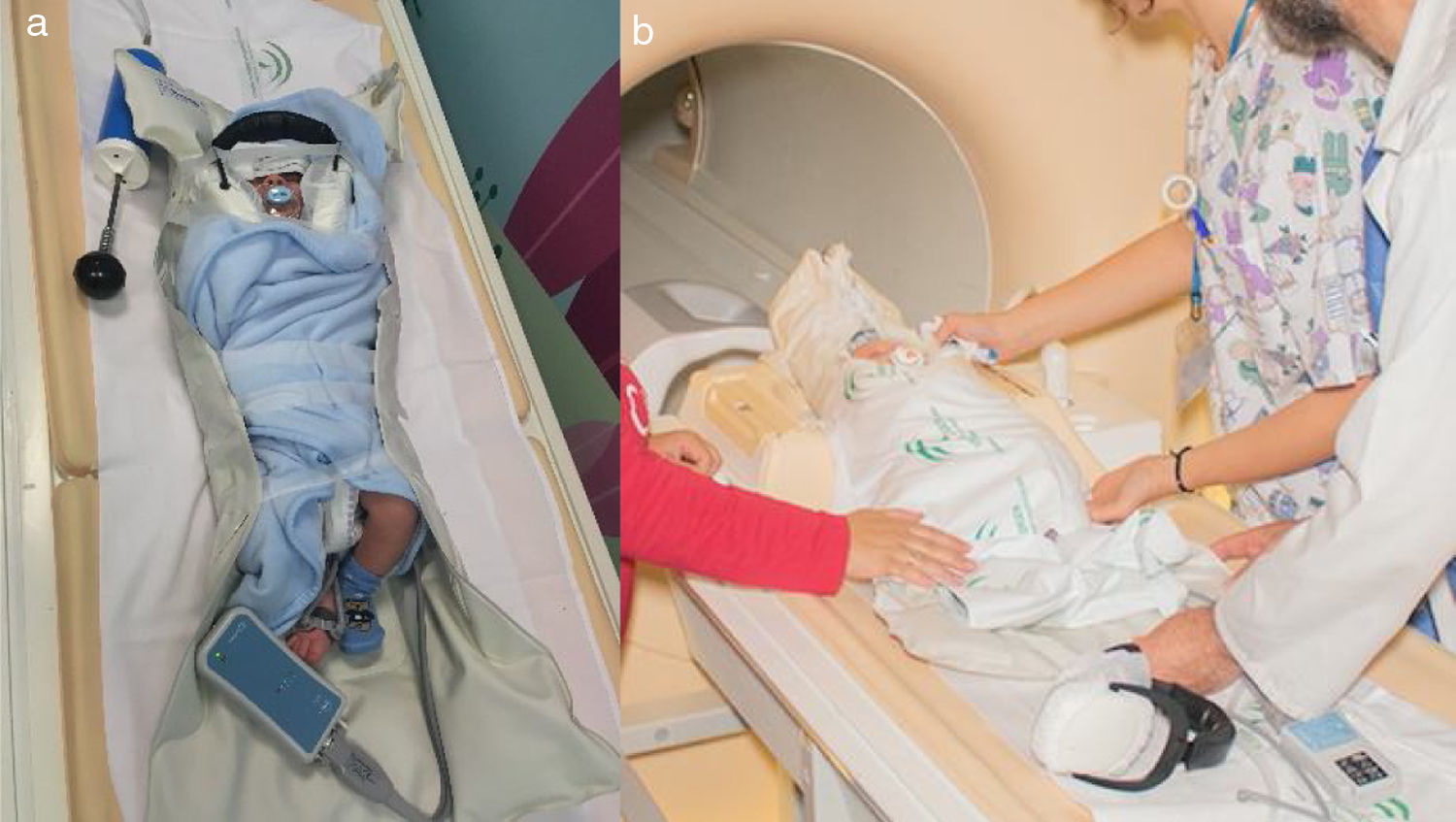
Heart rate and oxygen saturation were monitored throughout the study with an MRI-compatible pulse oximeter placed on the child's foot. Diaphragm movement was also monitored with an MRI-compatible detector. Finally, the infant was wrapped in a blanket and placed on the mattress (Vakuum-Kissen, Schmidt, Garbsen, Germany) and a suction system was connected to a device on one side of the mattress to remove the air from the mattress (Figure 1a). After the infants had fed, the parents/nursing staff held them in their arms for 10–15 min in a dark room. Subsequently, the patient was taken to the MRI room and placed on the MRI table with their head inside the coil (Figure 1b). The parents could accompany the children in the MRI room if they wished.
Two newborns in whom the technique of “feed and sleep” and immobilisation with an air mattress was used. Image 1 shows the infant wrapped in a blanket in the immobilising mattress. The mechanism for removing the air from the inside of the mattress is seen in the upper right-hand corner. The pulse oximeter is beside the infant’s right foot. Eye protection isolating the infant from visual stimuli. Image 1b shows another newborn being placed on the magnetic resonance imaging table with their head inside the head coil.
When the study ended, air was allowed to re-enter the mattress, which lost its rigidity, and the child was transferred to the neonatology floor or remained in the radiology unit until their first feeding. Contraindications for this technique were clinical instability, feeding problems or risk of respiratory compromise.
All the studies were conducted with a 1.5-Tesla MRI scanner (Philips Ingenia, Netherlands). The sequences used were axial diffusion (b0 and b1000 values), axial T2-weighted fast field echo (FFE) sequences, sagittal T1-weighted 3D sequences, axial T2-weighted sequences and coronal T2-weighted sequences, in that order. Some additional sequences depending on the patient’ disease included axial T2-weighted FLAIR sequences, time-of-flight angiographies without contrast, sagittal T2-weighted 3D sequences and T1-weighted 3D sequences following administration of contrast. Controls were performed under the supervision of an anaesthetist who used inhaled sevoflurane, administered through a mask, with no need for intubation.
Imaging findings and demographics, including sex, age, indication for the study, number of sequences, duration of the study and incidents during the study were reviewed. Three paediatric radiologists with 7, 12 and 15 years of experience in interpreting paediatric head MRIs independently determined whether the MRI answered the clinical question (success of the test) and whether the study needed to be repeated. They rated the corresponding imaging quality on a scale of 1–4 (optimal, suboptimal, poor or very poor). The optimal quality studies showed no motion artefacts; those of suboptimal quality showed motion artefacts on 1–2 sequences; those of poor quality showed motion artefacts in almost all sequences, and those of very poor quality showed motion artefacts rendering the study impossible to assess. The characteristics of the failed studies were compared to those of the successful studies to identify predictive factors of the technique’s failure.
All the groups of paired data were analysed using Student’s dependent or independent paired t test, as appropriate. Fisher’s exact test was used to compare nominal variables between the group in which the technique succeeded and the group in which it failed. Prism 8 (GraphPad Software, Inc., La Jolla, CA, United States) was used for statistical analysis. A p value less than 0.05 was considered statistically significant.
ResultsForty-seven patients whose MRIs were performed with the “feed and sleep” and air mattress technique were enrolled in this study (19 girls; 28 boys; median age 21 days; interquartile range 10–45 days). Thirteen patients were premature and thirty-four patients were full-term. The indications for the case and control studies are included in Table 1. Thirty-eight patients had been admitted to the neonatology department at the time of the study. Forty-seven patients whose MRIs were performed with general anaesthesia were used as controls (19 girls; 28 boys; median age 21 days; interquartile range 11–44 days). Seven controls were premature and thirty-nine controls had been admitted to the neonatology department on the day of the study.
Clinical characteristics of 47 cases who underwent magnetic resonance imaging (MRI) of the head with the technique of “feed and sleep” and immobilisation with an air mattress and 47 controls who underwent MRI of the head under general anaesthesia.
| Characteristics | Cases (n = 47) | Controls (n = 47) |
|---|---|---|
| Girls/boys | 19 (40%)/28 (60%) | 19 (40%)/28 (60%) |
| Age (days) | Median: 21 | Median: 21 |
| Interquartile range: 10–45 | Interquartile range: 11–44 | |
| Gestational age | <37 weeks, n = 13 | <37 weeks, n = 7 |
| ≥37 weeks, n = 34 | ≥37 weeks, n = 40 | |
| Inpatient | N = 38 | N = 39 |
| Outpatient | N = 9 | N = 8 |
| Indications | Asphyxia, n = 20 | Asphyxia, n = 14 |
| Intracranial bleeding, n = 10 | Intracranial bleeding, n = 4 | |
| Seizures, n = 5 | Seizures, n = 6 | |
| Perinatal infection, n = 3 | Perinatal infection, n = 3 | |
| Hypotonia, n = 2 | Hydrocephaly, n = 6 | |
| Hypertonia/hyperreflexia, n = 2 | Post-cardiac surgery, n = 4 | |
| Intracranial cyst, n = 1 | Intracranial cyst, n = 2 | |
| Hypoglycaemia, n = 1 | Decreased consciousness, n = 2 | |
| Dehydration, n = 1 | Polymalformative syndrome, n = 2 | |
| Apnoea, n = 1 | Horner syndrome, n = 1 | |
| Subgaleal haematoma, n = 1 | Spots on the scalp, n = 1 | |
| Intracranial tumour, n = 1 |
Table 2 summarises the independent evaluation of the quality of the case and control MRIs by three paediatric radiologists. In the case group, 42 (89%) MRIs using the technique of “feed and sleep” and immobilisation with an air mattress were performed successfully, answering the clinical question. Three MRIs could not be performed and two MRIs were performed but were not of a sufficient quality for diagnosis. These 5 MRIs had to be repeated with general anaesthesia. Table 3 compares the studies that were successful using this technique and the studies that failed. Of the 5 cases that failed, four were performed on an outpatient basis, and there was a statistically significant link between the test having been done on an outpatient basis and its failure (p value 0.02). The patients in whom the technique failed had an older mean age than those in whom it succeeded (28.2 versus 59.8 days old) without achieving statistical significance (p value 0.20).
Evaluation of magnetic resonance imaging (MRI) studies of the head for the 47 cases and 47 controls by three paediatric radiologists with 7, 12 and 15 years of experience in interpreting MRIs of the head in children.
| Cases n = 47 | Controls n = 47 |
|---|---|
| Does the MRI answer the clinical question? | |
| Yes, n = 42 | Yes, n = 47 |
| No, n = 2 | No, n = 0 |
| Not performed, n = 3 | |
| Does the MRI need to be repeated? | |
| Yes, n = 5 | Yes, n = 0 |
| No, n = 42 | No, n = 47 |
| MRI quality | |
| Optimal, n = 28 | Optimal, n = 42 |
| Suboptimal, n = 14 | Suboptimal, n = 5 |
| Poor, n = 1 | Poor, n = 0 |
| Very poor, n = 1 | Very poor, n = 0 |
| Not performed, n = 3 | |
Optimal: no motion artefacts; suboptimal: artefacts on 1–2 sequences; poor: artefacts on almost all sequences; very poor: study impossible to assess; not performed: the patient did not fall asleep and the test was not performed.
Comparison between the cases in which the technique of “feed and sleep” and immobilisation with an air mattress succeeded and the cases in which it failed.
| Successful MRI with mattress N = 42 | Failed MRI with mattress N = 5 | p Value | |
|---|---|---|---|
| Age (days) | 28.2 | 59.8 | 0.20 |
| Boys/girls | 26/16 | 2/3 | 0.43 |
| Inpatient/outpatient | 37/5 | 1/4 | 0.02 |
| Premature/full-term | 12/30 | 1/4 | 0.70 |
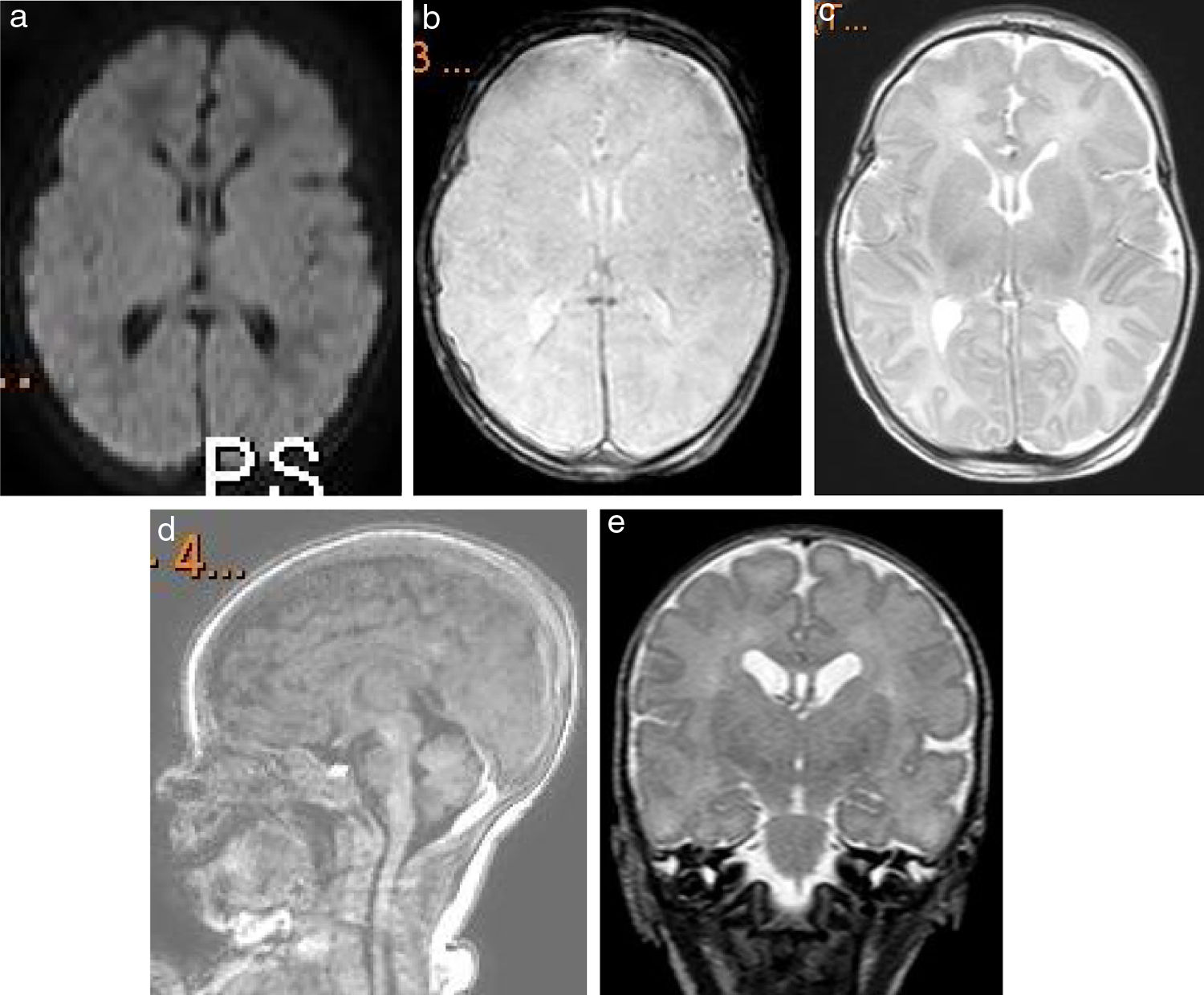
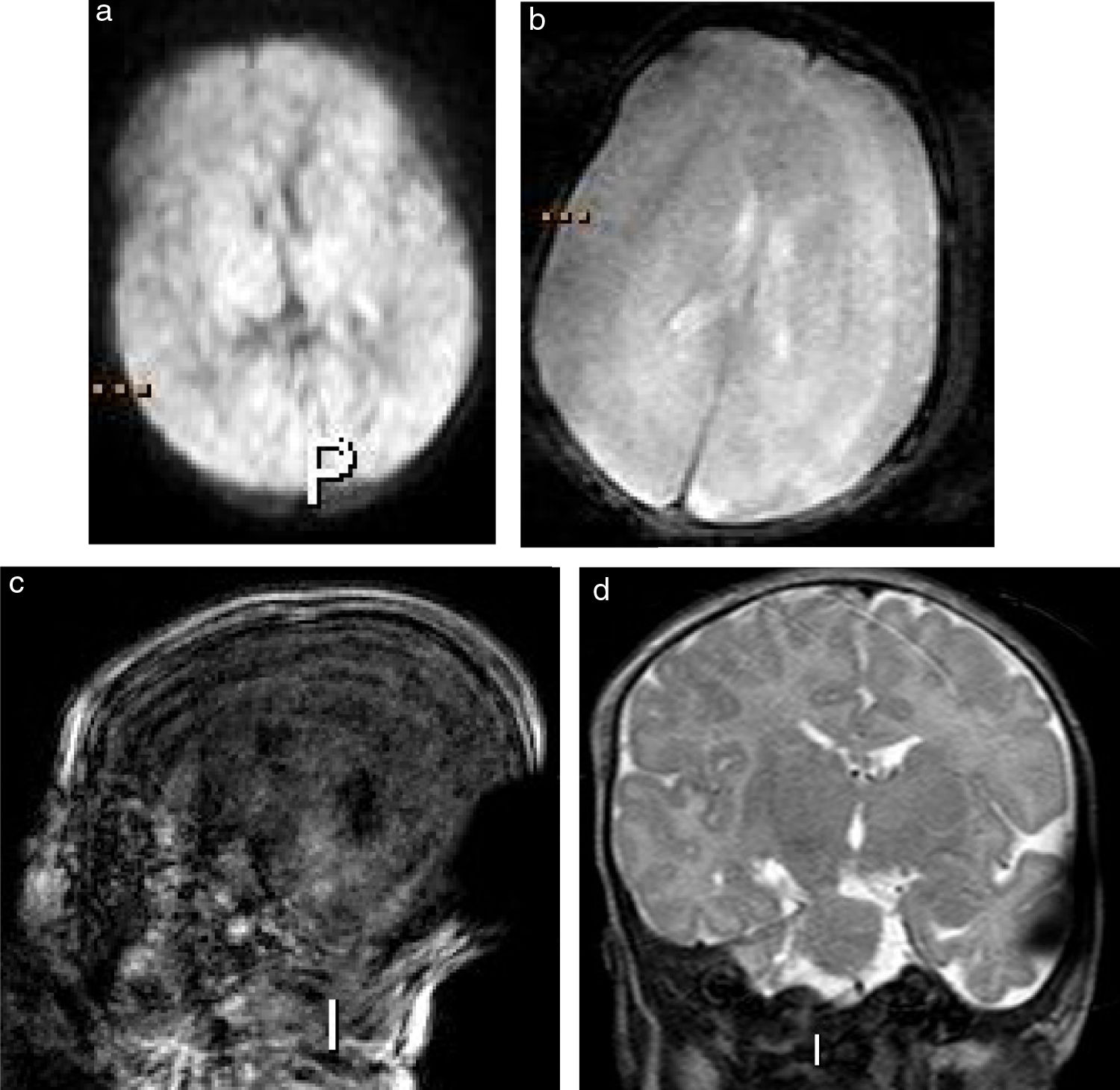
Among all the cases, 60% were of optimal quality, without any motion artefacts; 30% were of suboptimal quality, with motion artefacts on 1–2 sequences; 6% could not be performed; and 4% showed motion artefacts on multiple sequences rendering them impossible to assess. Examples of optimal quality and very poor-quality MRIs are shown in Figs. 2 and 3, respectively. In 10 (21%) studies, at least one sequence had to be repeated due to motion artefacts. In the rest, the child moved, preventing the continuation of the study. The mean duration of the MRIs (from the first sequence to the last) was 16.6 min (range 6–34 min).
Images from axial diffusion (a), axial gradient echo (b), axial T2-weighted (c), sagittal T1-weighted 3D (d) and coronal T2-weighted magnetic resonance imaging sequences (e) in a 7-day-old girl admitted to the neonatology floor due to suspected perinatal asphyxia. This study was performed with the technique of “feed and sleep” and immobilisation with an air mattress and evaluated by three reviewers to be of an optimal quality.
Images from axial diffusion (a), gradient echo (b), sagittal T1-weighted 3D (c) and coronal T2-weighted magnetic resonance imaging sequences in a full-term 14-day-old boy due to suspected perinatal asphyxia. This study was conducted on an outpatient basis with the technique of “feed and sleep” and immobilisation with an air mattress. The three reviewers deemed it of a very low quality, with motion artefacts on all sequences, and suggested that it be repeated with general anaesthesia.
Among the controls which were performed with general anaesthesia, 100% were of diagnostic quality, with no need to repeat any study. Of these cases, 89% were of an optimal quality, whereas 11% were suboptimal with motion artefacts in 1–2 sequences (the radiologist in charge decided not to repeat them, given that the study overall presented good quality and reducing anaesthesia time was prioritised). In 3 (6%) studies, at least one sequence had to be repeated due to motion artefacts. The mean duration of the MRI studies was 19.7 min (range 11–44 min). The mean duration of the MRI studies of the controls (19.7 min) was longer than that of the cases (16.6 min) (p value 0.03). This difference was due to the 3D isovolumetric sequences used in the controls but not the cases in order to shorten the duration of the studies (2D sequences were used), as well as the post-contrast 3D isovolumetric sequences used in 3 controls (2 due to suspicion of active intracranial infection and 1 to characterise a tumour), which had an approximate duration of 3–4 min.
There was no disagreement among the three radiologists as to which studies needed to be repeated. There were 5 disagreements between the evaluators in classifying cases as optimal or suboptimal quality; these cases were re-evaluated and a consensus was reached. No complications associated with immobilisation techniques or general anaesthesia were observed in any of the studies.
In the first year of experience with this technique, the use of general anaesthesia was avoided in 42 newborns out of 47 MRIs performed.
DiscussionBrain MRI is a technique widely used in children in the first year of life and is traditionally performed with general anaesthesia. In the last decade, centres have started using alternatives to general anaesthesia to perform these studies.
General anaesthesia carries a risk of possible cardiorespiratory arrest that is three times higher in children than in adults, with an incidence of 1.4 arrests per 10,000 anaesthetised patients, more than half of which occur in children under one year of age.15,16 This, and the possible long-term side effects reported, such as learning and attention disorders,4,5 have led many centres to seek alternatives to general anaesthesia for performing studies in infants. Our study and others10–12,14 have shown that MRI may be performed in infants with no need for general anaesthesia.
At our hospital, using the technique of “feed and sleep” and immobilisation with air mattress we have managed to reduce the number of cases of anaesthesia in this population, with a success rate of 89%. This is similar to that reported in prior studies with a success rate of 90%–100% using the technique of “feed and sleep” and immobilisation with air mattress.11–14
Our study showed that children who underwent the study on an outpatient basis presented a greater likelihood of not completing it satisfactorily, a finding not reported in previous studies. In our experience, this may have been due to the fact that many children who came from home arrived asleep and grew more irritable when they were changed and immobilised in the mattress. The children in whom the study failed also had an older mean age than those in whom it succeeded, without attaining statistical significance. Prematurity was not shown to be a factor associated with the technique's failure, in contrast to a study by Antonov et al.14
Our study enrolled infants under 3 months of age referred for a wide variety of diseases who were either inpatients or outpatients. Other studies have enrolled infants up to 6 months of age11 and studied other anatomical regions such as the spine, cardiovascular system and genitourinary tract.11,13 Our short-term goal is to use this technique to study other organs and systems, extend its use up to 6 months of age and re-evaluate the results. Two other advantages of the use of this technique are a shortened waiting list for MRIs with general anaesthesia and the lower cost of this technique as it excludes anaesthesia and associated staff costs. However, the use of this technique may also increase costs in some patients, if they must be seen again to perform the study with anaesthesia.
This study has some limitations, as it was conducted at a single centre and some procedures were performed by radiology technicians and nurses with less paediatric experience during a holiday period. These questions might have increased numbers of technique failures and motion artefacts in the final analysis. It should be noted that although the staff were less experienced, the results of this technique were good. Our study only measured the time period between the first and the second sequence; it did not measure the actual time for each study from the patient’s arrival on the unit to their departure from the unit. The protocols used with the mattress technique were shorter than the studies performed with general anaesthesia, which might have slightly biased the results. The patients considered controls were slightly different from the cases in that they were not only clinically unstable but also had more serious conditions requiring longer or more complex MRI studies. Another limitation of the study is that we did not perform more complex sequences such as tractography or spectroscopy to assess whether they may be used with this technique.
ConclusionThe technique of “feed and sleep” and immobilisation with an air mattress is feasible and safe for performing MRIs of the head in children under 3 months of age. The systematic use of this technique by staff who have experience with paediatric patients is useful for preventing the need for general anaesthesia.
AuthorshipEach one of this article’s authors made a substantial contribution to the study concept and design, data acquisition or data analysis and interpretation. They all contributed to the drafting of the article or to the critical review of its intellectual contents. They all approved the definitive version of the article.
Conflicts of interestThe authors declare that they have no conflicts of interest.