Traumatic and especially inflammatory-infectious dental lesions are very prevalent in our context. Inflammatory-infectious disease is usually discovered incidentally on imaging studies that include the orofacial region. Moreover, these conditions can result in potentially severe complications, so early diagnosis and treatment are important. Multidetector computed tomography offers good diagnostic performance for dental lesions, although the radiological findings can be subtle and can go undetected if the radiologist is not familiar with them. Likewise, invasive dental procedures are becoming increasingly common, and these can also result in complications. On the other hand, in daily practice a variety of radiolucent mandibular lesions or developmental anomalies can lead to erroneous interpretations. For these reasons, radiologists should be familiar with possible findings related with dental conditions.
La patología dentaria traumática y en especial la inflamatorio-infecciosa son muy prevalentes en nuestro medio. Esta última suele encontrarse de forma incidental en muchos de los estudios radiológicos que incluyen la región orofacial. Además, es una potencial causa de complicaciones graves, lo que hace que su diagnóstico y tratamiento precoz sean importantes. La tomografía computarizada multidetector ofrece un buen rendimiento diagnóstico en la patología dentaria, aunque sus manifestaciones radiológicas pueden ser sutiles y si no se conocen, pasar desapercibidas. Asimismo, son cada vez más frecuentes los procedimientos dentales invasivos, no exentos de complicaciones. Por otra parte, en la práctica diaria pueden encontrarse variedad de lesiones mandibulares radiolucentes o anomalías del desarrollo que pueden llevar a interpretaciones erróneas. Por todo ello, es recomendable que el radiólogo esté familiarizado con los posibles hallazgos en la patología dentaria.
Dental disease and the associated complications are a common cause of medical consultation1. It is estimated that more than half of adults over the age of 30 have some type of dental infection2. Therefore, dental abnormalities are a very common incidental finding in multidetector computed tomography (MDCT) scans performed daily for other reasons3,4.
Without treatment, they can cause serious complications (including deep neck infections) which can even be life-threatening5,6. In such cases, identification of the source of infection is essential in establishing a definitive aetiological treatment1.
Moreover, in studies that include the orofacial region, the radiologist may encounter abnormalities in tooth development or radiolucent lesions of the mandible, some associated with the tooth, which, due to their great variety, can be a challenge to diagnose7.
This article sets out to review the anatomy and discuss the most prevalent types of dental disease in our setting, particularly traumatic and inflammatory-infectious disorders. We also address the technique and the potential complications of different dental procedures, whether performed for therapeutic or aesthetic reasons, as aesthetic procedures are becoming increasingly more common1.
TechniqueThe imaging technique of choice is MDCT with helical acquisition. Its high spatial resolution (the thinnest possible slice thickness is recommended) and the ability to perform reconstructions in the three spatial planes (axial, coronal and sagittal) make it easier to detect subtle lesions1.
The use of intravenous iodinated contrast is not usually necessary, except in cases of suspected infectious complications1.
AnatomyThe tooth is anatomically composed of two clearly differentiated parts: the crown and the root1 (Fig. 1A). The crown is the visible part of the tooth in the mouth and is composed of different tissues1. The innermost part is the pulp, which is radiolucent and contains the neurovascular structures that support the tooth. The pulp is surrounded and protected by two mineralised layers: the outer layer, the enamel, which is harder and more radiopaque; and the inner layer, the dentin, which is less hard and less dense1.
A) Normal anatomy of the tooth. B) Numbering of adult teeth according to the World Dental Federation System classification. C) Numbering of deciduous teeth according to the World Dental Federation System classification. ©Radiology Department, Hospital Universitario de Basurto, Bilbao, Spain.
The root, surrounded by alveolar bone, is formed by the caudal extension of the pulp and dentin1. The most distal end of the root is known as the apex, where we have the openings of the root canals which allow the neurovascular structures to pass into the tooth. The root is surrounded by another mineralised layer called cementum, which has a density similar to dentin and is therefore difficult to identify by MDCT3.
Each tooth is housed in a bone hole, called the alveolar process, to which it is attached through the periodontal ligaments3. Radiologically, these ligaments form a very thin low-density layer of between the root and the lamina dura of the alveolar bone, called the periodontal space4.
Humans have two types of teeth during our lives4:
- •
At the age of six months we begin to form a first set of 20 temporary teeth, which we gradually lose until they disappear around the age of 122.
- •
Around the age of seven, a second, permanent set of 32 teeth begins to emerge, which makes up the secondary or adult dentition1,2.
The most widely used classification worldwide for the numbering of teeth is that published by the World Dental Federation System1 (Fig. 1 B). This classification assigns two numbers to each tooth:
- •
The first number indicates the quadrant the tooth is in. In the permanent teeth: 1 - upper right quadrant; 2 - upper left quadrant; 3 - lower left quadrant; 4 - lower right quadrant. In primary teeth: 5 - upper right quadrant; 6 - upper left quadrant; 7 - lower left quadrant; 8 - lower right quadrant1.
- •
The second number (1–5 in the primary teeth and 1–8 in the permanent) determines the exact position of the tooth within the quadrant, from medial to lateral1.
This is usually related to trauma to the craniofacial region, which is very prevalent in our setting4. An estimated one third of all individuals will experience some type of traumatic dental injury in their lifetime1.
FractureFracture is the most common type of injury in permanent teeth1. It is defined as a break in continuity in any of the tissues of the tooth, affecting the crown or the root1. Extension of the fracture through the pulp is associated with a worse prognosis due to the risk of neurovascular structure involvement and devitalisation of the tooth2 (Fig. 2A–D).
Multidetector computed tomography of the orofacial region in sagittal (A), coronal (B and C) and axial (D) planes. Non-displaced dentoalveolar fracture, which crosses the dental pulp at the level of the root (A and B). Tooth fracture through the pulp. The free fragment is in the patient's mouth (C and D). ©Radiology Department, Hospital Universitario de Basurto, Bilbao, Spain.
When accompanied by fractures in the alveolar bone, they are called dentoalveolar fractures and are more likely to be associated with tooth instability through damage to the periodontal ligament structures4 (Fig. 2A and B).
DislocationThis is the most common type of injury in the primary teeth4. It is caused by injury to the periodontal ligaments; in adults it is therefore usually accompanied by alveolar fracture4. Dislocations include various types of injuries1:
- •
Extrusive luxation: increase in the periodontal ligament space, almost always in the apical region, with the tooth maintaining its location within the corresponding alveolar process1 (Fig. 3A–C).
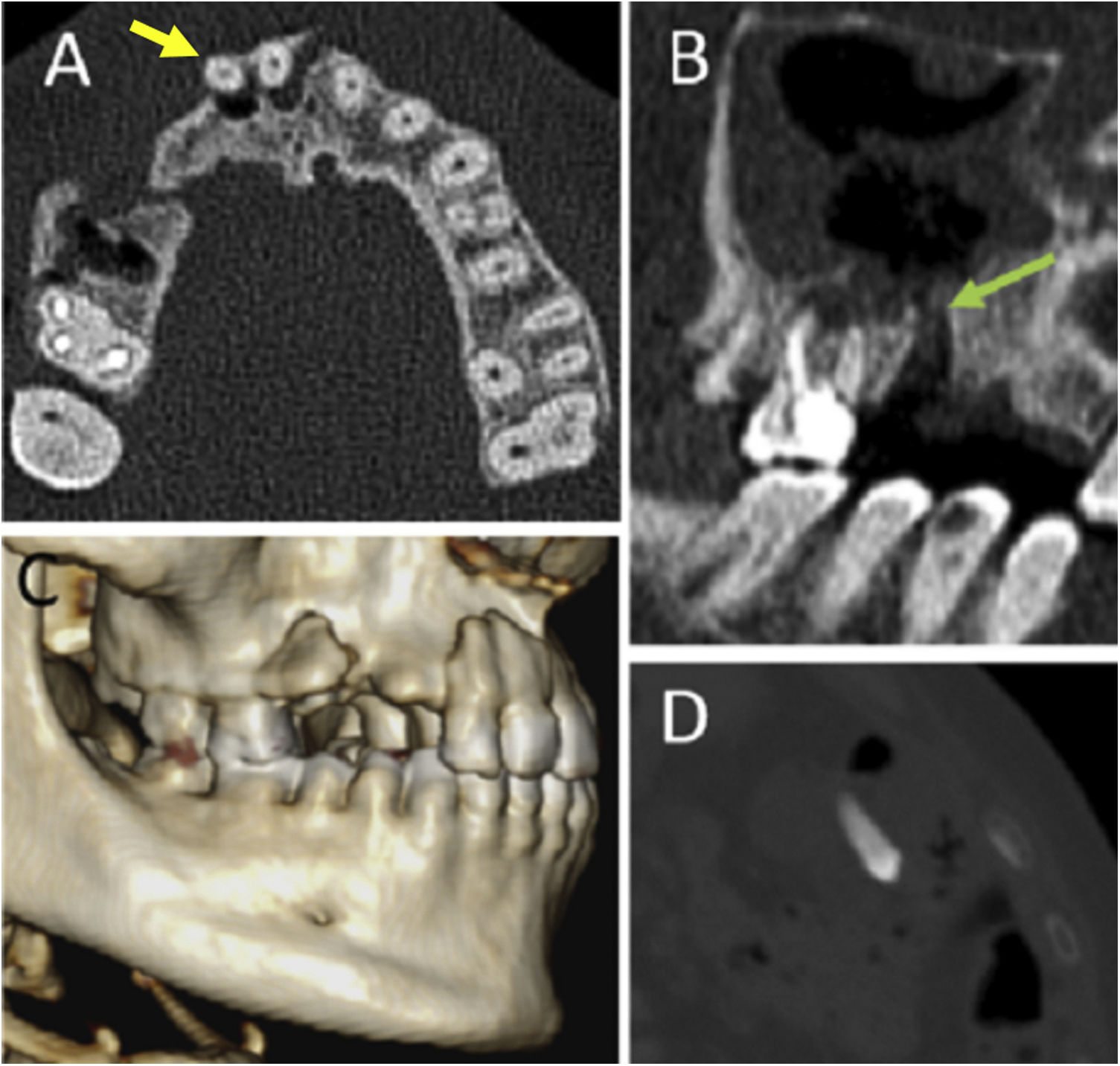
Figure 3.Multidetector computed tomography (MDCT) of the orofacial region in axial (A) and sagittal (B) planes and 3D reconstruction (C). Complex fracture on the right side of the maxillary bone, with extrusive dislocation towards the vestibule of teeth 11 and 12 (yellow arrow in A) and absence of teeth 13, 14 and 15. Partial occupation of the right maxillary sinus with a bone defect due to a floor fracture which has caused an oroantral fistula (green arrow in B). Abdominal MDCT in axial plane and bone window (D): a complete tooth can be seen inside the patient's transverse colon (magnified image of this area).©Radiology Department, Hospital Universitario de Basurto, Bilbao, Spain.
(0.18MB). - •
Intrusive luxation: reduction or disappearance of the periodontal ligament space due to impaction of the tooth in its alveolar socket2.
- •
Lateral luxation: asymmetrical increase in the periodontal space with greater involvement of one side or the other. It is nearly always accompanied by alveolar fracture1.
Avulsion: absence of the tooth in its corresponding alveolar socket2 (Fig. 3A and C).
After a tooth fracture or avulsion, possible aspiration or swallowing of broken fragments or teeth should always be ruled out (Fig. 3D).
Inflammatory/infectious diseaseThe main causes of inflammatory-infectious dental diseases are poor oral hygiene and dental procedures1. The disease process can originate in the tooth itself or in the adjacent soft tissues5:
- •
Endodontal infections: they start as dental caries, in which the infection destroys the enamel. It then penetrates the dentin and eventually reaches the pulp. From there, the infection will spread directly to the dental apex through the root canal. On MDCT they are seen as hypodense lesions due to the demineralisation of enamel and dentin1 (Fig. 4A and B).
Figure 4.Multidetector computed tomography of the orofacial region in axial (A and C), sagittal (B) and coronal (D) planes. Areas of dentin demineralisation in relation to dental caries (yellow arrows in A and B). Radiolucent periapical halo in relation to periradicular disease changes (green arrows in C and D). ©Radiology Department, Hospital Universitario de Basurto, Bilbao, Spain.
(0.12MB). - •
Periodontal infections: they begin as an infection of the gingiva or gingival mucosa (gingivitis), which later penetrates the periodontal space4. From there, through the periodontal ligaments, the infection can spread caudally to the apex2. On MDCT they can be seen as a hypodense halo which begins around the root bifurcation4.
- •
Pericoronitis: it is a particular case of periodontal infection4. It is usually caused by impaction of food around the mandibular third molars when they have not yet erupted4. It is seen on MDCT as a radiolucent halo around the crown of the unerupted tooth4.
When the infection spreads to the dental apices, what is known as periapical disease occurs. This term covers a spectrum of diseases that occur around the apex of the tooth, including periapical abscess, periapical granuloma and periapical cyst3.
Osteolysis derived from the inflammatory changes initially manifests on MDCT as a widening of the periapical space, with a fine radiolucent halo surrounding the root and apex3 (Fig. 4C and D).
Periapical abscesses occur in infections that the immune system is unable to control. They are usually accompanied by fever, pain and local inflammatory signs. Radiologically, they manifest as periapical lytic lesions with signs of activity in the form of poorly defined borders and associated acute osteomyelitis changes3.
In cases of locally persistent latent infection periapical granulomas (encapsulated granulation tissue) or, alternatively, periapical cysts (due to the proliferation of secretory epithelial cells) may develop over time4. The cyst is usually larger, grows over time and has more clearly defined borders than the granuloma, although radiologically they may be indistinguishable2,3.
The rate of complications associated with periapical infections is generally higher than that of other types of dental infection5. Other factors which also influence the risk of complications are the duration of the infection (prior to the initiation of antibiotic treatment) and the tooth affected3.
Treated early, most infections tend to be limited to the tooth3. However, if left untreated, the infection can penetrate the adjacent alveolar bone and even spread to other neighbouring anatomical areas, leading to potentially serious infectious conditions5. In such cases, MDCT is an essential tool which makes it possible to delimit the extent of the infection, detect possible complications and identify the dental origin of the condition in order to establish a definitive aetiological treatment1.
ComplicationsOdontogenic sinusitisPeriapical infections and dental procedures on the upper dental arch (particularly at the level of the second molars) are a common cause of maxillary sinusitis1,3.
Imaging findings do not differ from sinusitis by other causes3. We should suspect dental origin in cases of unilateral maxillary sinusitis (up to 70% are estimated to be of odontogenic origin), especially if there are also radiological manifestations of periapical disease in the underlying teeth1,3.
Definitive imaging diagnosis requires the identification of an oroantral fistula, visible on MDCT as a bony interruption in the floor of the maxillary sinus1 (Fig. 5A–C). The adjacent soft tissues tend to occlude the bone defect, so the diagnostic sensitivity to see the communication improves if we perform a series with air retention in the mouth1.
Multidetector computed tomography of the orofacial region in coronal (A and C) and sagittal (B) planes. Radiolucent halo of periapical disease around tooth 26, with a bone defect suggestive of an oroantral fistula in the floor of the left maxillary sinus (yellow arrow in A), which is partially occupied. Absence of extracted tooth 15, with a bone defect suggestive of an oroantral fistula in the floor of the right maxillary sinus (green arrow in B and C), which shows mucosal thickening with an inflammatory appearance. ©Radiology Department, Hospital Universitario de Basurto, Bilbao, Spain.
The aetiological diagnosis is important, as it has a bearing on treatment1. Sinusitis of odontogenic origin is usually associated with a higher rate of anaerobic infection1. Moreover, depending on the size of the socket, it may not resolve spontaneously and may require surgical repair1.
Odontogenic mandibular osteomyelitisInfectious dental disease is a common cause and we should always rule it out in cases of osteomyelitis, particularly of the jaw3. It occurs when the periodontal infection manages to penetrate the underlying alveolar bone1.
The radiological manifestations of odontogenic osteomyelitis are the same as for osteomyelitis by other causes. The radiological findings vary according to the stage of the disease1. In acute phases, bone involvement is predominantly lytic1. Later, bone involvement becomes mixed, with the development of areas of reactive sclerosis in the trabecular bone. Reactive periosteal thickening and cortical fragmentation may also be seen. Possible complications include the formation of bone sequestrations (devitalised and infected cortical fragments that perpetuate the infection) and fistulisation to adjacent soft tissues, which can lead to recurrent abscesses1,6.
Deep neck infectionsOdontogenic infections are associated with a large proportion of deep neck infections in adults as a result of spread from adjacent tissues3. The initial route of spread to the deep neck spaces varies according to the location of the affected tooth5:
- •
In the mandibular dental arch, the apices of the second and third molars are below the insertion of the mylohyoid muscle, whereby the infection usually spreads directly into the submandibular space5.
- •
The rest of the teeth in the lower arch have their apices above the insertion of the mylohyoid, hence spread will be to the sublingual space5.
- •
In the upper dental arch, infection of the molars can spread to the masticator space, and from there following the mandibular branch of the trigeminal nerve to the intracranial compartment5.
Any infection with involvement of deep neck spaces can become potentially life-threatening. MDCT is very useful for detecting complications, including abscess formation, airway stenosis, thrombosis of vascular structures and spread to the mediastinum1,6.
Mediastinal spread is usually through the retropharyngeal space, although it can also be through the carotid space. It is a very serious complication with a very high mortality rate (15%–40%) which requires immediate aggressive treatment. The initial imaging findings can be subtle (for example, slight increase in mediastinal fat density, small flecks of fluid) and may easily go unnoticed6.
Ludwig anginaThis is an unusual type of neck infection. It is a rapidly progressive cellulitis of the floor of the mouth due to spread of the infection to the sublingual and submandibular spaces5.
It is estimated that more than 90% of cases have an odontogenic origin3. The infection can be located in any lower tooth, although it tends to be more common in the second or third molars1. It occurs more frequently in diabetic and immunosuppressed patients1.
Involvement is usually bilateral and rapidly progressive, with severe oedema that displaces the tongue posteriorly and obstructs the airway6. It can lead to serious, life-threatening conditions which require immediate action. Diagnosis is usually clinical, although MDCT plays a fundamental role in assessing the airway, detecting collections or gas bubbles and identifying the responsible tooth1.
Orbital cellulitisIntraorbital spread of infection is a rare but serious complication. Early diagnosis is essential to avoid severe complications such as vision loss3.
It can originate in several ways, the most common one being direct spread from a maxillary sinusitis3. Another possible route of spread is the extension of facial cellulitis through the subcutaneous cellular tissue until it reaches the periorbital region, where it can invade the postseptal or intraorbital compartment3.
Intracranial complicationsThese are rare and are associated with a poor prognosis3.
Orbital cellulitis can give rise to septic thrombosis of the ophthalmic vein, which spreads to the cavernous sinus. Radiologically, it presents as an increase in the lumen of the venous structures, with hypodense content and absence of contrast uptake3.
Other possible complications due to direct spread are epidural abscesses, subdural empyemas, meningitis and even intraparenchymal abscesses3.
Dental proceduresDental procedures are becoming more common and are not devoid of complications2. Correlation between the procedure carried out and the time interval until when the imaging test was performed is important2.
Dental fillingThis is the treatment used in caries limited to enamel and dentin, with preservation of the pulp and the neurovascular tissue of the tooth2. It consists of debriding the infected tissue with subsequent restoration of the tooth using metal or resin amalgams (amalgams have less artefact in MDCT studies)2 (Fig. 6A and B).
Multidetector computed tomography of the orofacial region in axial (A, D and E) and sagittal (B and C) planes. Post-filling changes in the crown of several teeth in the upper arch (blue arrows in A and B). Roots of teeth with normal endodontics (yellow arrows in C, D and E) and with periradicular radiolucent halo (green arrows in D and E). ©Radiology Department, Hospital Universitario de Basurto, Bilbao, Spain.
Used for the treatment of caries with spread to the pulp2. It consists of the removal of the devitalised pulp, with subsequent filling and sealing of the pulp cavity using an inert, bacteriostatic material with high-density on MDCT2. Apart from that, the tooth maintains its shape (Fig. 6C).
As in all other invasive dental procedures, the most common complication is infection, visible in the form of a periradicular radiolucent halo4. However, this finding is nonspecific and may also be secondary to sequelae of a periapical infection prior to the procedure or to a foreign body reaction that generates periradicular osteolysis, which is radiologically indistinguishable from infection. The differential diagnosis is therefore clinical (Fig. 6D and E).
Tooth extractionTooth extraction may be performed on teeth devitalised due to advanced infection or on healthy teeth for aesthetic reasons. The latter is particularly common in third molars which are impacted during eruption1.
In the initial days post-extraction, the corresponding alveolar process usually presents fluid content (sometimes blood-stained) and isolated gas bubbles related to the procedure1. Over time, the cavity left by the extraction is remodelled and may even disappear4.
The main complication associated with extraction is infection. This tends to occur around three or four days after the procedure, with increased pain and local inflammatory signs1. MDCT helps to determine the extent of the infection and detect other complications1.
Possible non-infectious complications include bleeding, subcutaneous emphysema (sometimes associated with pneumothorax or pneumomediastinum), incomplete removal and bone fractures. A further complication in the case of fractures is the possible formation of oroantral fistulae in the maxillary sinus floor1,2,4.
Dental implantsMetallic dental implants are an increasingly used option in patients with tooth loss, either for aesthetic purposes or to recover functionality1.
The most common complication is peri-implant osteolysis or peri-implantitis, which appears on MDCT as a radiolucent halo around the prosthesis. It may be secondary to infection or be an inflammatory reaction to a foreign body. Imaging findings are nonspecific and the differential diagnosis is clinical. In any event, without treatment, the process results in the loosening and possible movement of the implant1.
Another important complication to be taken into account is injury to adjacent anatomical structures during placement of the prosthesis, including the mandibular canal or the maxillary sinus floor 1 (Fig. 7A). To avoid that, prior cement grafts can be performed in patients with insufficient bone volume1. On MDCT, they appear as irregular masses with a density similar to bone and should not be confused with osteoma-type bone lesions1. If the prior use of cement is required, the fact that it can become fragmented and move must be taken into account. If this occurs, it is important to recognise the fragments as such, especially within the maxillary sinus, where they can lead to a misdiagnosis of fungal sinusitis1 (Fig. 7B and C).
Multidetector computed tomography of the orofacial region in sagittal (A and B), and axial (C) planes. Implant malposition with injury to the maxillary sinus floor, which is almost completely occupied (A). Aseptic loosening of a dental implant in the upper left dental arch. Migration of the implant to the maxillary sinus (yellow arrow in C) and presence of cement fragments (green arrows in B and C) inside the maxillary sinuses can be seen. ©Radiology Department, Hospital Universitario de Basurto, Bilbao, Spain.
Not all radiolucent images of the mandible are associated with periapical infections. This group covers a wide spectrum of lesions, both odontogenic and non-odontogenic, and the degree of aggressiveness is highly variable7,8. They can be found incidentally in asymptomatic patients and being familiar with such lesions and their signs is essential for correct interpretation of the findings7.
Our focus here is solely on radiolucent (or mixed) lesions of odontogenic origin. They generally tend to be benign cystic lesions with no or sluggish growth, although some may also show locally aggressive behaviour9. Radiological findings may overlap and a definitive imaging diagnosis is not always possible9.
Radicular or periapical cystThey are the most common odontogenic cystic lesions8. They develop as a result of chronic periapical infections; hence they are located in close contact with the dental apex7 (Fig. 8A).
Multidetector computed tomography of the orofacial region in sagittal (A, C, E and F), axial (B) and oblique sagittal (D) planes. A) Periapical cyst: periapical lytic lesion in a tooth with a small caries in its anterior margin. B) Nasopalatine cyst: maxillary lytic lesion centred on the midline in slight contact with the root of a tooth in the upper left quadrant. C) Dentigerous cyst: pericoronal lytic lesion around an unerupted third molar. D) Dentigerous cyst: pericoronal lytic lesion in a tooth in the upper arch. E) Keratocyst: expansile lytic lesion in the posterior part of the mandibular body, in contact with the root of several teeth in the lower arch, with marked thinning of the inferior cortical bone. F) Ameloblastoma: multilocular lytic lesion in the posterior part of the mandibular body, slightly expansive. ©Radiology Department, Hospital Universitario de Basurto, Bilbao, Spain.
Curettage of these lesions is necessary during tooth extraction, as otherwise they can persist, leading to so-called residual cysts7.
An important differential diagnosis of maxillary periapical cysts is nasopalatine cyst (Fig. 8B), a benign cystic lesion centred on the nasopalatine duct in the midline of the maxillary bone. Although not of dental origin, it may have contact through proximity with the roots of the teeth in the upper arch. The fact that the location is specific is helpful in making the distinction3.
Dentigerous or follicular cystIt is the second most common type of cyst7. They are developmental lesions, most often associated with mandibular third molars which have not yet erupted or are impacted7. They form around the crown of the tooth, are usually unilocular and can become expansile, albeit without causing destruction of cortical bone8 (Fig. 8C and D).
Primordial cystThese are cystic lesions which replace a tooth which should have formed, but is missing due to cystic degeneration during odontogenesis8.
Odontogenic keratocystIt is a benign cystic neoplasm arising from the dental lamina7. They can appear surrounding any part of the tooth, either the root or the crown. They are more common in the ramus or posterior part of the mandibular body, sometimes associated with a tooth that has not yet erupted7,9. They are well-defined lesions and may be unilocular or multilocular, with small satellite cystic lesions around the larger one, which usually has dense keratin content within7,9. Their appearance is typically expansile and may include areas of cortical interruption and resorption of adjacent tooth roots (Fig. 8E). The definitive diagnosis is usually histological, and surgery is the treatment of choice, with high rates of local recurrence8,9. In multiple lesions, Gorlin-Goltz syndrome should always be considered8.
AmeloblastomaThis is a neoplasm arising from the remnants of the dental lamina7. Ameloblastomas are most common in the ramus or posterior part of the mandibular body, sometimes associated with unerupted third molars8. They may be unilocular or multilocular, with well-defined borders, occasionally with a soft tissue component associated with cystic areas8. They are typically expansile lesions which can be locally aggressive, with erosion of dental roots, cortical bone destruction and extraosseous spread8 (Fig. 8F). Histological examination is essential to confirm diagnosis and determine the degree of malignancy8.
Periapical cemento-osseous dysplasiaOf unknown aetiology, it typically occurs in asymptomatic women aged 40 to 507. It is a disease of the spectrum of benign fibro-osseous lesions and originates in the periodontal ligament9. Despite not strictly having a dental origin, the lesions develop in very close contact with the teeth. An increase in the production of connective tissue occurs around the root of one or more generally healthy teeth. This causes generally well-defined, characteristically periapical radiolucent lesions which calcify over time and become mixed7 (Fig. 9A and B). In the florid variant of the disease, the lesions tend to be larger and multiple, even affecting all the mandibular and maxillary roots9.
Multidetector computed tomography of the orofacial region with curved reconstruction (A) and in sagittal plane (B). Typical periradicular lesions in a patient with periapical cemento-osseous dysplasia. Multiple mixed lytic and sclerotic lesions can be seen surrounding the root of numerous teeth of both the upper and lower dental arches. ©Radiology Department, Hospital Universitario de Basurto, Bilbao, Spain.
These abnormalities can cause aesthetic or mechanical problems in the eruption of the tooth, in which case extraction might be necessary. In other cases, they are discovered incidentally in asymptomatic patients10,11:
- •
Total or partial tooth agenesis: due to degeneration of the dental follicle prior to odontogenesis. It may give rise to a residual or primordial cyst7.
- •
Enclosed tooth (Fig. 10A–D): located partially or totally inside the bone10.
Figure 10.Multidetector computed tomography of the orofacial region in coronal (A and D), axial (B) and sagittal (C) planes. A) Supernumerary tooth completely enclosed in the mandibular symphysis. B) Supernumerary teeth completely enclosed in the maxillary bone. C) Unerupted, impacted third molar. D) Inverted, dysmorphic supernumerary tooth, enclosed in the maxilla, showing incipient eruption into the maxillary sinus. ©Radiology Department, Hospital Universitario de Basurto, Bilbao, Spain.
(0.12MB). - •
Impacted tooth (Fig. 10C): blocked within the bone due to mechanical problems11.
- •
Supernumerary tooth (Fig. 10A, B and D): usually single, most often in the midline of the maxilla (in this location it is called mesiodens)2,11. They can be eumorphic or dysmorphic10. They do not usually erupt, but they can cause mechanical problems for the eruption of the rest of the teeth10,11. The other anatomical variants are more common in these supernumerary teeth10.
- •
Dysmorphic tooth (Fig. 10D): tooth with abnormal size or shape10,11.
- •
Ectopic tooth (Fig. 10B and D): in a position removed from its theoretical physiological location10.
- •
Inverted tooth (Fig. 10C): can even erupt into the nasal cavity10.
Inflammatory-infectious dental disease, radiolucent mandibular lesions and an ever-increasing growth in the number of dental procedures can be challenging for the radiologist in diagnostic terms, due both to their often subtle presentation and the risk of serious secondary complications. Radiologists should therefore make themselves familiar with the possible findings in dental disease.
Authorship- 1
Responsible for study integrity: JJGM, LAM and RFP
- 2
Study conception: MSA, JJGM, LAM and RFP.
- 3
Study design: MSA, JJGM and LAM.
- 4
Data collection: MSA, JJGM and LAM.
- 5
Data analysis and interpretation: N/A.
- 6
Statistical processing: N/A.
- 7
Literature search: MSA, JJGM, LAM and RFP.
- 8
Drafting of the article: MSA.
- 9
Critical review of the manuscript with intellectually relevant contributions: JJGM, LAM and RFP.
- 10
Approval of the final version: MSA, JJGM, LAM and RFP.
The authors declare that they have no conflicts of interest.