The ultrasonographic diagnosis of pneumothorax is based on the analysis of artifacts. It is possible to confirm or rule out pneumothorax by combining the following signs: lung sliding, the A and B lines, and the lung point. One fundamental advantage of lung ultrasonography is its easy access in any critical situation, especially in patients in the intensive care unit. For this reason, chest ultrasonography can be used as an alternative to plain-film X-rays and computed tomography in critical patients and in patients with normal plain films in whom pneumothorax is strongly suspected, as well as to evaluate the extent of the pneumothorax and monitor its evolution.
El diagnóstico ecográfico del neumotórax se basa en el análisis de artefactos. Combinando los siguientes signos: el deslizamiento pulmonar, las líneas A y B, y el punto pulmonar, es posible diagnosticar o descartar de forma segura la presencia de un neumotórax. Una ventaja fundamental de la ecografía pulmonar es su fácil acceso en cualquier situación crítica, especialmente en pacientes en la UCI. Por ello, la ecografía torácica podría utilizarse como alternativa a la radiografía simple y la TC en el paciente crítico, en pacientes con alta sospecha de neumotórax y radiografía normal, y para valorar la extensión del neumotórax y monitorizar su evolución.
The utility of a simple thoracic X-ray and CT in the study of pneumothorax is very well defined but in some cases–especially in patients in a critical condition thoracic X-rays are hard to interpret and in many occasions these patients cannot go to the CT room. It is under these circumstances that the thoracic ultrasound is a useful alternative.1 Also it is an accessible cheap and innocuous technique.
Several studies have proven that in order to diagnose pneumothorax the pulmonary ultrasound of the bedhead of patients is as efficient or even more efficient than the conventional X-ray performed when the patient is in the supine position.1–3 Gas molecules produced in the lung cause some sort of dispersion in the sound waves emitted by the transducer in infinite directions which in turn makes the formation of diagnostic images just impossible. However they cause a series of artifacts whose analysis we can use to confirm or discard pneumothorax. As a matter of fact evaluating one pneumothorax through an ultrasound is nothing but a study of artifacts.
Our goal is to describe the main ultrasound signs of pneumothorax, consider its practical clinical applications and recognize the possible limitations of this modality.
Technical issuesOne high frequency lineal probe (5–12MHz) of one conventional ultrasound scanner is enough for the analysis of pleural line–which is superficial. The lower-frequency convex sound waves (2–5MHz) will be used to evaluate the subjacent pulmonary artifacts toward the pleural line. Pulmonary patterns are dynamic so the retrospective analysis of static images is not adequate. This is why the main signs are shown in video.
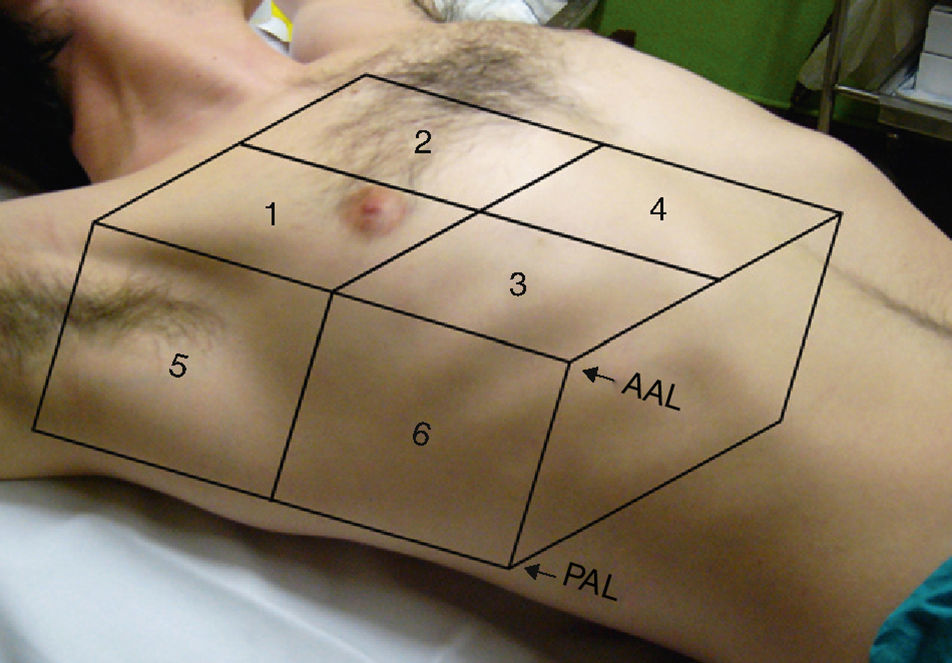
The patient is often in the supine position and the pleura are identified through one intercostal space. In an attempt to carry out the most possible systematic study it is advisable to divide each hemithorax into various areas and quadrants as shown in Fig. 1. The “anterior area” is limited by the sternum, the clavicle and the anterior axillary line–that is divided into 4 quadrants. The “lateral area” is limited by the anterior and posterior axillary lines–that is divided into 2 quadrants.
Systematic study by quadrants of one patient in the supine position. Both the anterior and posterior axially lines mark out the anterior and lateral areas which are in turn divided into 6 quadrants. Anterior area: Quadrants 1 to 4. Lateral area: Quadrants 5 to 6. Since there is a tendency for free air to accumulate in the most elevated area we started our study by the intersection made up of the 4 anterior quadrants. If we wish to do a complete exam each one of the 6 quadrants need to be analyzed. Doing one systematic analysis it is possible to identify most pneumothoraces. AAL: Anterior axillary line; PAL: Posterior axillary line.
Several signs have been described for the echocardiographical diagnosis of pneumothorax. In our experience the following three (3) signs are the ones with the top diagnostic utility:
Lung slidingThe limit between the visceral pleura and the surface of lungs is visible in the ultrasound as an echogenic line–pleural line. Lung displacement in the thoracic cavity during respiration causes one alteration in the pleural line called “lung sliding” (video 1).
We must remember that lung sliding excludes pneumothorax with a negative predictive value and a sensibility of 100%.4 However its absence (video 2) is not a synonym of pneumothorax. In patients in critical condition with massive atelectasis, intubation of the main bronchus, pulmonary contusion, chronic obstructive pulmonary disease (COPD), acute respirator distress syndrome or pleural adherences, lung sliding can or cannot be seen.5,6 This is why the absence of a sign of lung sliding needs to be combined with other signs if we want to improve the diagnostic efficiency of this test.
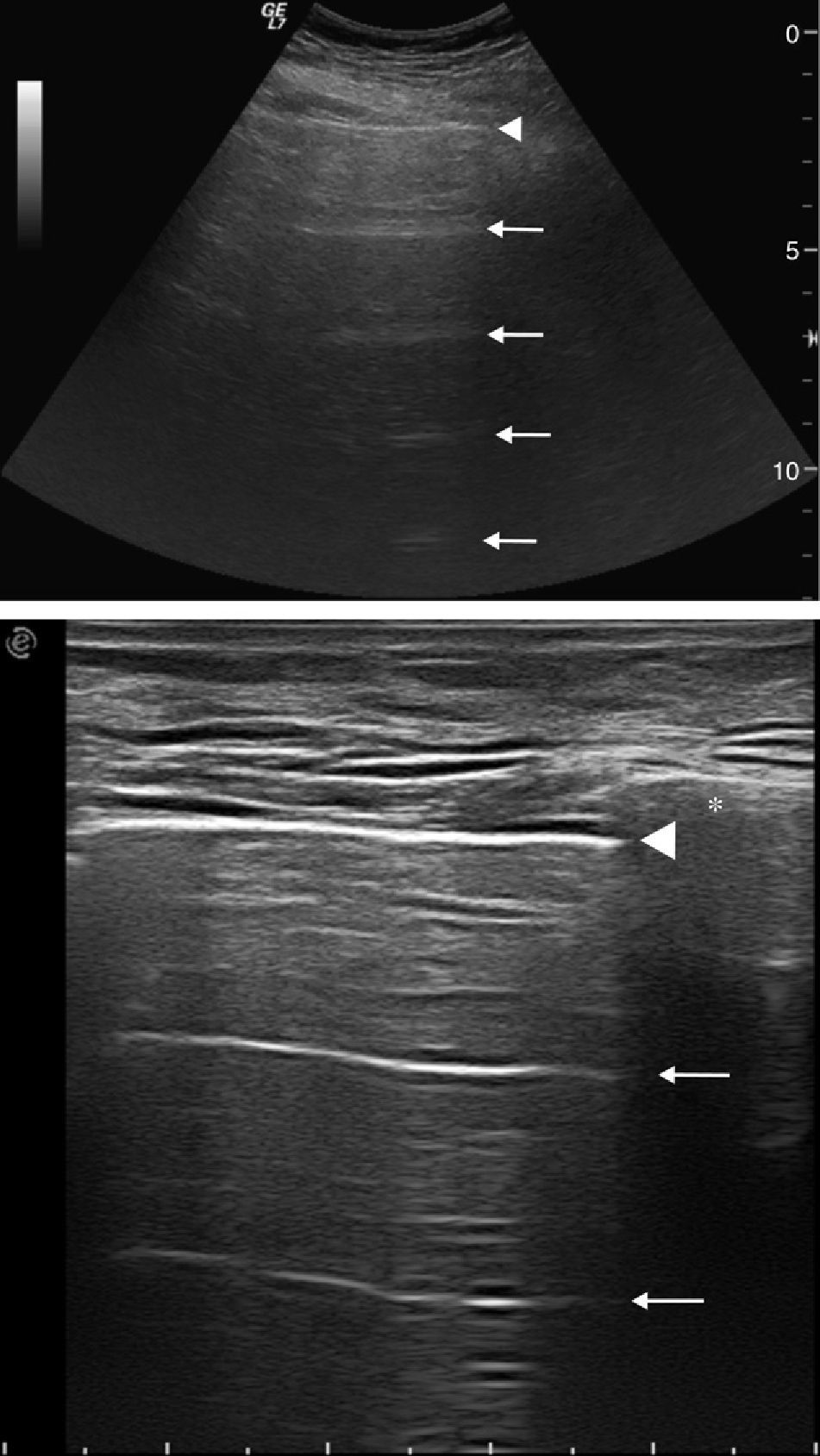
Lines A are the result of a reverberation artifact7 that translates into the appearance of several lines that run parallel to pleural lines at regular intervals.
We must remember that lines A can be seen both in the usually well-aired lung and in the pneumothorax (Fig. 2). The difference between one and the other is the presence of the absence of the sign of lung sliding. Lichtenstein et al.8 have described a sensibility of 100% and a specificity of 96% when lines A and the absence of the sign of lung sliding are combined (video 3).
Lines A. (A) fifty-two-year-old male admitted in the hospital Intensive Care Unit with a clinical presentation of right pneumothorax after thoracic trauma. Lines A are reverberating artifacts seen as horizontal lines (arrows) stemming from pleural line (arrow head) and set in irregular intervals. (B) Forty-three-year-old healthy woman showing lines A (arrows) in a breast control ultrasound set in regular intervals below the pleural line (arrow head). In healthy people we can see these reverberating artifacts with no pathological meaning as a consequence of a usually well-aired lung. The asterisk represents the rib from intercostal space with its acoustic shadow.
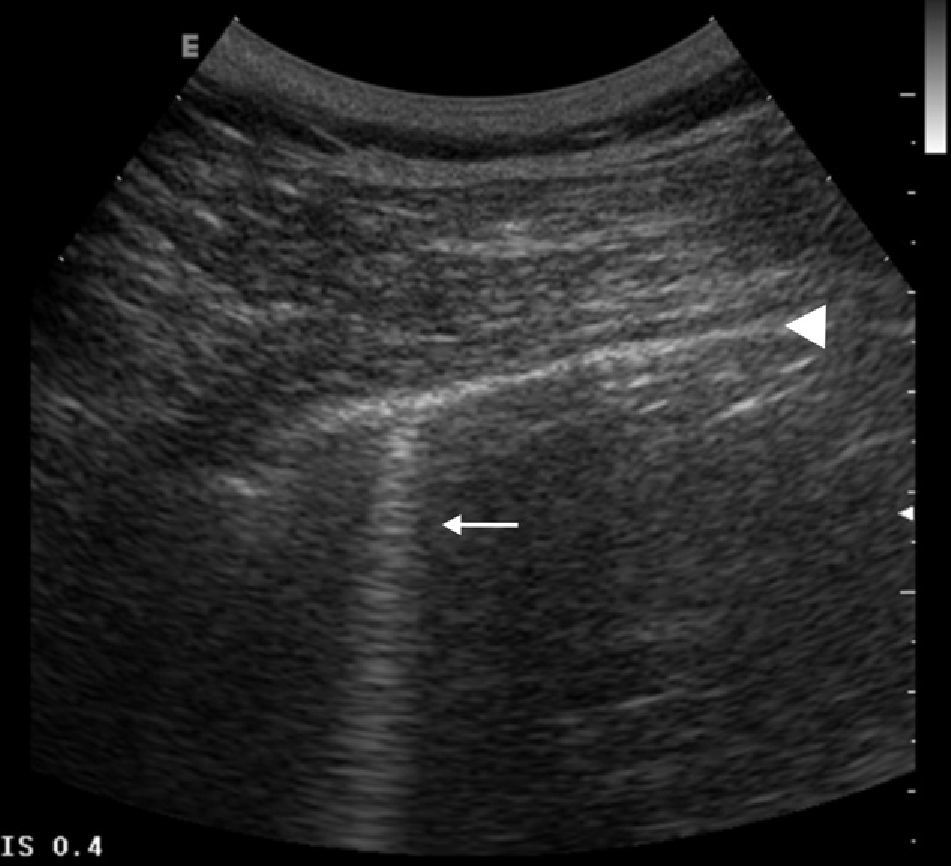
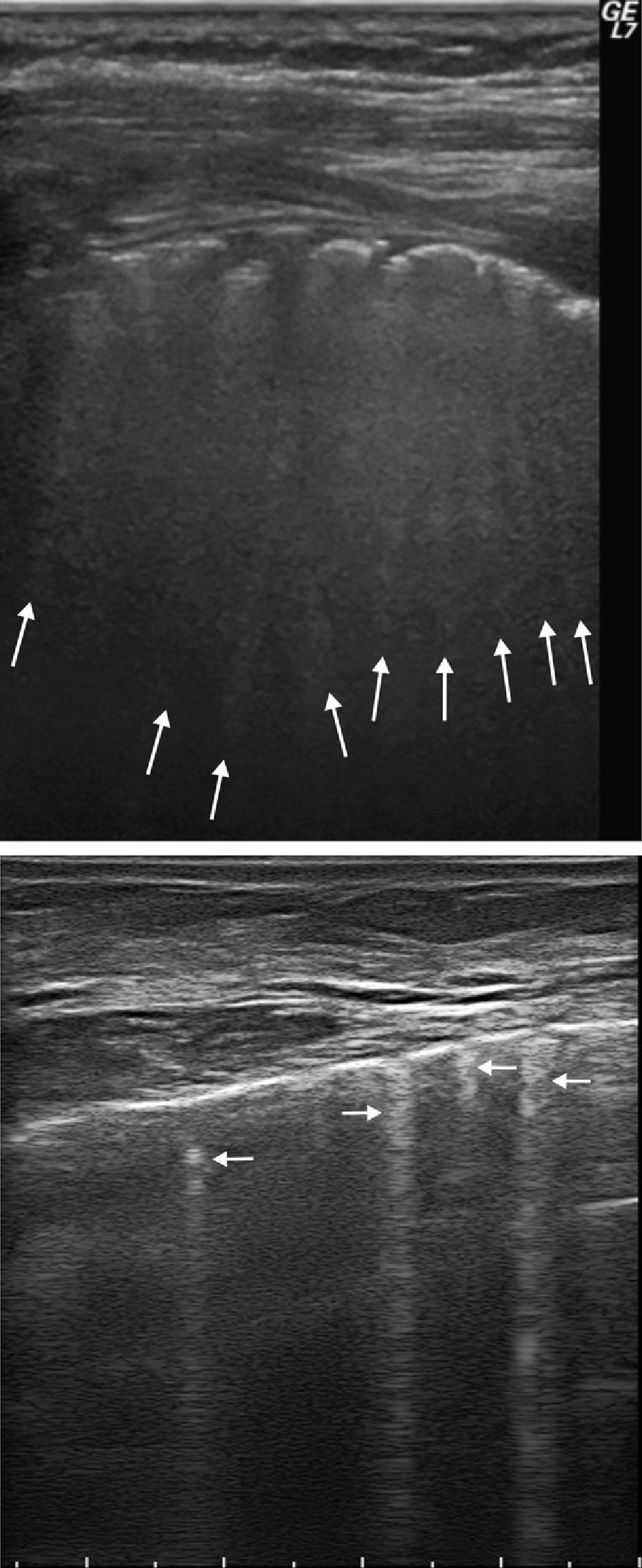
Lines B are a comet tail artifact9 produced in the pleural line at the contact zone between the visceral pleura and the usually well-aired lung.2,10 Lines B can be seen separately in the normal lung (Fig. 3) and its number goes up in cases of interstitial or alveolar affectation (Fig. 4).11–13
We must remember that its importance lies in that this artefact excludes pneumothorax.8
Line B. Sixty-one-year-old male who had previously undergone a lung biopsy of his right hemithorax. Ultrasound control 3h later to discard pneumothorax. One line B (arrow)– perpendicular and synchronic to the movement of pleural line (arrow head) shows a usually well-aired lung and allows us to exclude pneumothorax. In normal people we usually see these comet tail artifacts separately in the inferior-lateral thoracic wall.
Lines B. (A) Sixty-nine-year-old male. Thoracic ultrasound shows irregularity in the echogenic pleural line that is interrupted due to lung mass with pleural extension. The numerous lines B (arrows) are due to the fact that ultrasonic waves are transmitted through the pathological interstitium. Its presence discards pneumothorax. (B) Forty-eight-year-old woman with known affectation of lung interstitium in whom we can see multiple lines B (arrows) secondary to the presence of interstitial liquid. Because they are born from the surface of visceral pleura the importance of lines B is that its presence indicates the expansion of the lung.
It is the point where visceral and parietal pleural leaves separate. It is a dynamic image like the sign of lung sliding that contains findings of well-aired lung and pneumothorax (Fig. 5 and video 4).14 To find the lung point the transducer slowly slides into the inferior-lateral portion of the thorax (Fig. 6 and video 5). Medially the lung sliding will be absent in the area of pneumothorax. More laterally there will be lung sliding where the visceral and parietal pleural leaves are still in contact. Lung point will be identified as the intermediate point where lung sliding will be visualized intermittently given that with the respiratory movement the collapsed lung intermittently slides into the area of pneumothorax.
We must remember that the sign confirms the presence of pneumothorax14,15 and it can also be used to evaluate its importance. The more lateral and inferior the lung point is to the thoracic wall the bigger it is. One very posterior or absent lung point suggests a massive pneumothorax with complete lung actelectasis14 and predicts the need for implanting a tube for pleural drainage.16,17
Lung point. Seventy-two-year-old male who had previously undergone a lung biopsy due to the presence of a mass in his left lung. The ultrasound 3h after puncture shows the lung point (arrow) through an intercostal space (asterisk: ribs) confirming pneumothorax. The limit between the well-aired lung and the pneumothorax (lung point) can be seen as a disruption of pleural line (arrow head)–which in turn seems irregular and thickened.
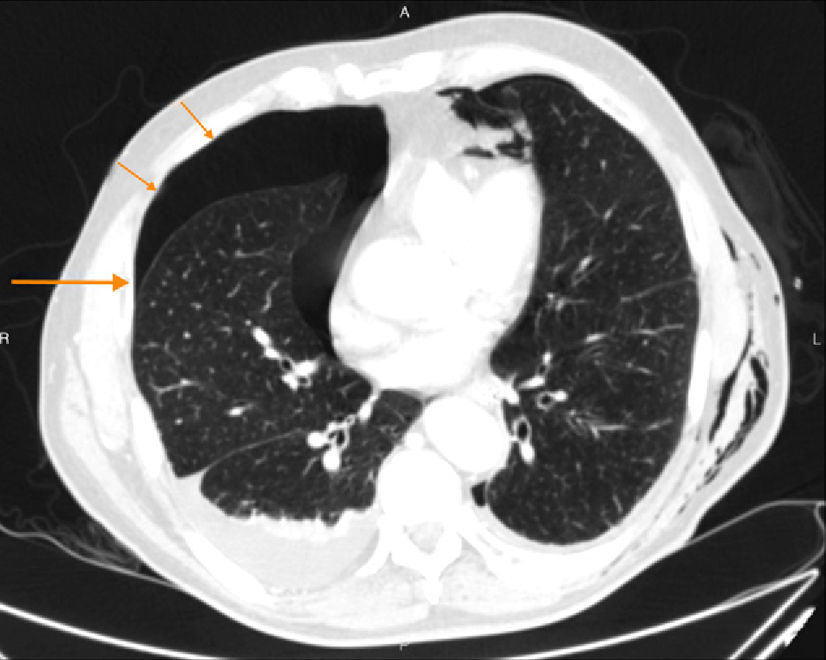
Location of lung point. CT-image of a polytraumatized patient with a large right pneumothorax and a small anterior and left posterior pneumothoraces. The arrows show the theoretical movement of the ultrasound probe toward the thoracic lateral wall in search for the lung point. The long arrows are showing the lung point in the lateral thoracic wall while predicting the extension of pneumothorax. Note the subcutaneous left emphysema that could prevent or complicate an adequate ultrasound access.
Now we will take a look at the clinical situations in which in our opinion the thoracic ultrasound can have a major role in the diagnosis of pneumothorax.
Unstable patientsICU patients are those who will benefit the most from this technique which in turn is possibly the main clinical application.
We must remember that in extremely urgent cases the ultrasound can replace the handheld portable conventional X-ray in the diagnosis of pneumothorax and it can also be used as a guide for the implantation of a drainage tube. The more critical the emergency, the easier the echographical signs on which the diagnosis should be based. This is why in unstable patients with thoracic pain, dyspnea and timpanism one echographical pattern with no sign of lung sliding with lines A and without lines B will lead to the implantation of a tube for pleural drainage.16–18
The handheld portable conventional X-ray is some times hard to interpret and frequently it is not possible to diagnose the presence of pneumothorax.19 These cases of hidden pneumothorax20 are important since they can be the product of hemodynamic instability. In polytraumatized patients requiring invasive ventilation or air transport the presence of pneumothorax16 needs to be discarded. Similarly in stable patients a small hidden pneumothorax modifies the criteria of follow-up, prognosis, and observation in the emergency room.16
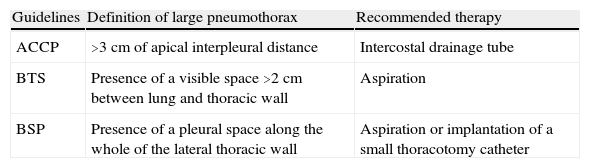
The percentage of collapsed lung is a major criterion to decide whether to implant a drainage tube or administer conservative therapy. The guidelines for the management of pneumothorax quantify its volume based on the distance between parietal and visceral pleura in the PA thorax plaque21 (Table 1). With ultrasound finding the lung point helps us quantify the extension of pneumothorax and predicts the need to implant a tube for pleural drainage.14–17,22
Comparison between the definition and the recommended therapy from the most important clinical guidelines on “large” pneumothoraces.
| Guidelines | Definition of large pneumothorax | Recommended therapy |
| ACCP | >3cm of apical interpleural distance | Intercostal drainage tube |
| BTS | Presence of a visible space >2cm between lung and thoracic wall | Aspiration |
| BSP | Presence of a pleural space along the whole of the lateral thoracic wall | Aspiration or implantation of a small thoracotomy catheter |
ACCP: American College of Chest Physicians; BSP: Belgian Society of Pulmonology; BTS: British Thoracic Society.
In our own experience with a series of 35 patients who underwent ultrasound after one CT guided-aspiration puncture that proceeded with a thin lung needle, 100% of the pneumothorax could be correctly diagnosed.23 Sartori et al.3 suggest that lung ultrasound can be the elective method to exclude, diagnose, and monitor the pneumothorax after lung post-biopsy–all guided by ultrasound. It can also be used to monitor the retraction of the thoracic tube and assess the persistence or not of the pneumothorax.24
Possible errors and limitationsThe thoracic ultrasound has a high negative predictive value in the detection of pneumothorax. The positive predictive value is somehow inferior since we can have coexisting conditions that complicate the echographical exam while giving false positives.1 The subcutaneous emphysema (Fig. 6), pleural calcifications or one patient with poor acoustic transmission can all or complicate the diagnosis.4,14,18 In patients with dyspnea, COPD, and pleural adherences lung sliding can be diminished or abolished.5,6 This sign can be the only finding enabling us to distinguish a pneumothorax from a big pleural bulla.8,25 Other possible limitations include pneumothoraces restricted to mediastinal area or posterior pneumothoraces as well as limitations from the curve of learning.
ConclusionsDespite lung ultrasound for the diagnosis of pneumothorax has been largely disregarded its practical utility has been confirmed. In our experience it is a fast, highly sensible non-invasive tool with a short curve of learning. Critical patients are the ones who will benefit the most from this modality. However if experienced in the use of this modality lung ultrasound can also be useful for the monitorization of pneumothoraces after lung post-biopsy and assessment of the retraction of pleural tube.
Ethical responsibilitiesProtection of humans and animalsAuthors confirm that no experiments have been done with humans or animals during this research.
Confidentiality of dataAuthors confirm that the protocols of their centers have been followed on matters concerning the publishing of data from patients. They also confirm that all patients included in this study have been given enough information and handed over their written informed consent for their participation in this study.
Right to privacy and informed constentAuthors confirm they have been given the written informed consent from patients and/or individuals included in this article. This paper is owned by its author of correspondence.
Authors- 1.
Manager of the integrity of the study: ALI and JAPB.
- 2.
Original Idea of the Study: ALI, JMNM, GBR, IFG and JAPB.
- 3.
Study Design: ALI, JMNM and JAPB.
- 4.
Data Mining: ALI, JMNM, GBR, IFG and JAPB.
- 5.
Data Analysis and Interpretation: ALI, JMNM and JAPB.
- 6.
Statistical Analysis: NA.
- 7.
Reference Search: ALI, IFG and JAPB.
- 8.
Writing: ALI and JAPB.
- 9.
Manuscript critical review with intellectually relevant contributions: ALI, JMNM, GBR, IFG and JAPB.
- 10.
Final Version Approval: ALI, JMNM, GBR, IFG and JAPB.
Authors declare no conflict of interest.
The following are the supplementary data to this article:
Sign of lung sliding. Spontaneous left pneumothorax. Forty-five-year-old male admitted to the intensive care unit with unknown sepsis. Suddenly he presented with non-radiating left thoracic pain and in the superior hemi-abdomen growing and worsening with deep inspiration. After performing abdominal and thoracic ultrasounds a left pneumothorax could be confirmed. This video shows the normal right hemi-thorax with preserved lung sliding. The movement of echogenic line corresponds to the sliding of pleural line seen through the intercostal space. Its presence excludes pneumothorax.
Lack of lung sliding. Spontaneous left pneumothorax. Same patient as video 1. The thoracic ultrasound of left hemithorax shows pleural line seen through the intercostal space. The lung sliding in thoracic cavity cannot be seen. Compare with the normal lung sliding of contralateral hemithorax shown in video 1.
Combination of lines A with no lung sliding. Same patient as Fig. 2A. Ultrasound shows lines A with no lung sliding in this patient with post-traumatic right pneumothorax. These combined findings enable us to diagnose pneumothorax with a high specificity.
Lung point. Same patient as Fig. 5. Lung point can be easily seen real time in the study like a dynamic image containing findings from both normal lung and pneumothorax. The limit between the well-aired lung and the pneumothorax in the pleural line (irregular and thickened) – the transition between presence and absence of lung sliding.
Location of the lung point. Same patient as Fig. 5. Medially the lung sliding will be absent in the area of pneumothorax. To find the lung point the transducer slowly slides into the inferior-lateral portion of thorax with the patient being in the supine position. Lung point will be identified as the intermediate point where lung sliding will be visualized intermittently. With the respiratory movement the collapsed lung intermittently slides into the area of pneumothorax and replaces the immobile pleural line.
Please cite this article as: Lasarte Izcue A, Navasa Melado J, Blanco Rodríguez G, Fidalgo González I, Parra Blanco J. Diagnóstico ecográfico del neumotórax. 2014;56:229–234.