Continual improvements in diagnostic modalities used for shoulder imaging have led to better resolution, sensitivity, and specificity. There is no consensus about whether conventional MRI, direct MR arthrography, indirect MR arthrography, or CT arthrography is the best method. Many publications from very diverse origins propose different criteria for selecting the technique to apply in different patients. However, the application of rigid protocols that do not include all the imaging options does not help patients. Moreover, this approach also restricts radiologists’ creativity, especially in countries in which resources are more limited. It is important to ensure the rational use of the techniques depending on the patient and the place, considering the patient's age, associated diseases, surgical possibilities, complications, and available equipment. This article reviews the state of the art in imaging rotator cuff and superior labral anterior and posterior lesions, considering the indications, advantages, and advantages of the different techniques in different cases.
La evolución constante de las modalidades diagnósticas para el hombro han mejorado la resolución, la sensibilidad y la especificidad. No hay consenso sobre cuál es el mejor método entre la resonancia magnética simple, artroRM directa, indirecta y artro-tomografía computarizada. Las publicaciones, de orígenes muy diversos, plantean diferentes criterios para seleccionar la técnica a emplear. La aplicación de protocolos de estudio rígidos que no incluyan todas las alternativas de imágenes no ayudan a los pacientes y restringen la creatividad, particularmente en nuestros países donde la limitación de los recursos es una constante. Es importante usar racionalmente las técnicas dependiendo del paciente y del lugar, teniendo en cuenta la edad, las enfermedades relacionadas, la posibilidad quirúrgica, las complicaciones y los equipos disponibles. En este artículo se revisa el estado actual de las imágenes para las lesiones del manguito de los rotadores y del labrum, considerando sus indicaciones, ventajas y desventajas.
Shoulder lesions are frequent and varied, particularly those involving the rotator cuff and the superior labrum. There is no consensus as to which is the most accurate diagnostic technique to study them, considering among them magnetic resonance (MR) without contrast, MR with intraarticular contrast injected directly (direct arthroMR), MR with intravenous contrast medium (indirect arthroMR) and CT arthrography. No doubt MR without contrast (simple) is the most accepted method to study shoulder lesions, however, due to the complexity of the rotator cuff, that of the labrum, the cartilage and that of other small structures, greater accuracy is required in many patients to indicate an adequate medical or surgical treatment.
This article will revise the current status of images for rotator cuff and labrum lesions, and their indications, advantages and disadvantages will be discussed, combining what is described in the bibliography with our own experiences.
Shoulder lesions that may need studies with direct or indirect articular contrastRotator cuff lesionsRotator cuff lesions are divided into two groups: the intrinsic and the extrinsic ones. The intrinsic lesions may be subdivided into those caused by age-related vascular or metabolic changes, which cause degeneration and rupture, and into intratendinous lesions generated by stretching and stress. The extrinsic ones include subacromial compression and other forms of external pinching, internal pinching, shoulder instability, acute trauma and repeated trauma. The most common scenario is a combination of these trigger factors.1
Rotator cuff ruptures may occur as a normal aging process. In a study of 306 shoulders in cadavers, Lohr et al.2 established that the incidence of complete and partial rupture of the supraspinous tendon was 19 and 32% respectively.
The location and extension of the lesions is variable. The tendon's rupture may be complete or partial, in which case, it may be located intrasubstance, on the articular surface, or in the bursa or in a mixed manner. Yamanaka et al.3 described within the group of partial lesions percentages of 2.4% for bursa lesions, 7.2% for those of intrasubstance and 3.6% for the articular ones in 249 specimens. Several authors have noticed a frequency 2–3 times greater than partial lesions on the articular surface on the bursa,1 and some have demonstrated up to 91% of the lesions of the articular type in young athletes.4
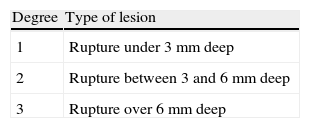
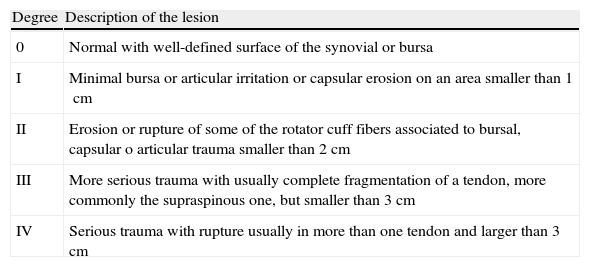
Lesions of the rotator cuff tendons may be classified in different ways. Neer5 initially defined Stage I (inflammation, hemorrhage, edema and pain), Stage II (tendon fibrosis) and Stage III (progressive rupture). Ellman6 established a classification for partial lesions according to the articular or bursa location, and the rupture area in mm2 (Table 1). Later on Snyder et al.7 proposed other criteria according to the location (articular, in the bursa or complete; A, B and C respectively) and its seriousness according to the arthroscopic findings (Table 2).
Snyder's classification of rotator cuff lesions.
| Degree | Description of the lesion |
| 0 | Normal with well-defined surface of the synovial or bursa |
| I | Minimal bursa or articular irritation or capsular erosion on an area smaller than 1cm |
| II | Erosion or rupture of some of the rotator cuff fibers associated to bursal, capsular o articular trauma smaller than 2cm |
| III | More serious trauma with usually complete fragmentation of a tendon, more commonly the supraspinous one, but smaller than 3cm |
| IV | Serious trauma with rupture usually in more than one tendon and larger than 3cm |
In rotator cuff lesions, it is recommended to determine the muscular volume to plan surgery and prognosis. Muscular atrophy is assessed according to the criteria of Goutallier et al.8 Originally, the parameters were described for computer tomography (CT), but they have later been used in MR taking as point of reference the oblique sagittal cuts where the 4 muscle groups are observed (Degree 0: there are no fat deposits; Degree 1: some fat bands; Degree 2: more muscle than fat; Degree 3: equal amount of muscle tissue and fat; Degree 4: more amount of fat than muscle; Degree 2 or higher is considered as substantial). One simple way of assessing supraspinous atrophy is to establish the so-called “tangent sign”, according to the Zanetti's method, drawing an imaginary line between the coracoids and the acromion on a sagittal plane shoulder image. A muscle is considered to be markedly atrophied when no muscle fibers are observed above the line drawn.9,10
Labrum lesionsUpper labrum lesions are not infrequent. The incidence recorded in the bibliography ranges 3.7 and 10% in patients who underwent arthroscopy.11–14
Different labrum trauma mechanisms have been proposed such as shoulder compression after falling on a hyperextended arm, or sudden traction. In addition, repetitive overuse is recognized among baseball pitchers, swimmers or tennis players as the origin of the lesion and microinstability. Urban et al.15 have postulated and summarized the relation between the trauma mechanism and the Slap (superior labral anterior and posterior) lesions, and they have stressed the compromise of the labrum with Slap II in acute trauma and traction mechanisms. When there is a mild repetitive trauma without a marked base instability, Type I lesions occur. Contrariwise, the patients with previous trauma-associated instability develop advanced and complex labrum lesions (Slap III or higher).
It is important to define superior labral lesion according to the initial arthroscopy classification by Snyder et al.16 into Type I (degeneration or fibrillation without rupture), Type II (oblique rupture. Subtypes: II A or anterior-superior; II B or posterior-superior, and II C or complete), Type III (in “cube loop” with preservation of biceps tendon insertion) and Type IV (in “cube loop” with extension to the bicep tendon). Maffet et al.17 added 3 types: Type V (superior labral lesion combined with the lower labrum), Type VI (partial flap lesion displaced down to the articular space) and Type VII (extended to the mid glenohumeral ligament). Later on Resnick et al. (Unpublished data) has described Type VIII lesions (a combination of the superior and posterior labrum) and Type IX (global labral lesion). Finally, Beltrán described Type X (with extension to the rotator interval including the superior coracohumeral and glenohumeral ligaments) (presented in the year 2000 during the congress of the American Society of Radiology).
None of these classifications takes into account the seriousness of the symptoms or the prognosis. The greatest usefulness of the typification of the lesions using contrast is directly related with the medical or surgical treatment. Many treatment protocols have been described. When conservative treatment is not enough, for Type I lesions debridement is generally accepted; for those of Type II, repair and fixation; for those of Type III, cleave of the “loop” fragment and repair of the remnant; for those of Type IV, in addition to cleave of fragment, bicep tendon repair or tenodesis is performed; in Types V and VI lesions, labral damage is repaired and a tenodesis is performed; in Slap VII tenodesis plus mid glenohumeral ligament repair is accepted; variant Type VIII requires capsulolabral reconstruction; in Types IX and X lesions debridement of labral complex and shoulder stabilization are performed.18
Other lesionsOther alterations that are not any less important such as humeral and glenoid head chondromalacia, glenohumeral and coracoid ligament rupture, compromise of bicep tendon and its pulley, or intra and extraarticular complex affections may require sophisticated images for its diagnosis. Therefore, the analysis must be comprehensive acting on the labrum and the rotator cuff. The study of shoulder instability in any of its variants is very complex because it involves several structures simultaneously, which often requires the use of articular contrast. Detailed description of these lesions is not the objective of this article.
Shoulder direct magnetic resonance arthrography, indirect magnetic resonance arthrography and computed tomography arthrographyThe concept of glenohumeral arthrography was introduced in 1930 according to what was published in an article by Oberholzer.19 The contrast is usually introduced by fluoroscopy-guided injection, which makes it an invasive method with higher radiation doses. With the advent of new techniques, conventional radiologic projections have been replaced by TC or MR.
Direct MR arthrography has used different contrast media such as saline, Ringer's solution and other types of saline. Nowadays paramagnetic media are more widely accepted (dimeglumine gadopentetate and the like). In order to guide the injection of these substances, several techniques and equipment are used including fluoroscopy, ultrasounds and, in some centers, MR or TC. However, the most usual procedure is fluoroscopy-guided anterior approach.20 In our center, the patient is laid supine and the injured shoulder is disinfected. The puncture point is marked, a local anesthetic is injected with a 24–26G needle, and then a lumbar puncture 20–22G needle is inserted in the articular space. In order to corroborate the position, 1–5ml of iodized contrast medium diluted in 50% saline is injected. Once the needle's correct position is confirmed, a 0.1ml solution of dimeglumine gadopentetate or other paramagnetic contrast medium, diluted in 20ml of normal saline (1:200) is injected. 12–15ml is usually introduced while monitoring entry and the patient's tolerance.
Indirect MR arthrography is based on the intravenous paramagnetic contrast's capacity to differentiate normal articular structures from lesions, attaining a so-called “arthrographic” effect, similar to that produced by the direct method. The contrast as such does not produce a signal, but it alters the relaxation of the neighboring substances improving tissue differentiation.21 The articular space usually contains little synovial fluid. The blood vessels in the synovial membrane lack basal membrane; therefore, synovial fluid is equivalent to a plasma ultrafiltrate, similar to the interrelation between plasma and interstitial space. A balance is quickly established between the plasmatic substance concentrations, including the contrast media bonded to the proteins and the synovial fluid. The contrast migrates to the articular space by two mechanisms: the pressure gradient between blood flow and the synovial fluid, and the osmotic diffusion capacity of the substances through the basal membrane. Active exercise has a positive effect by increasing on the one hand systemic pressure and on the other by scattering the synovial fluid outside the joint; this way, the osmotic diffusion gradient and the substances’ concentration difference are increased. Active exercise may have some negative effect when intraarticular pressure increases, similar to what happens when there is articular effusion, infection, inflammation or hemorrhage. Passive exercise, which does not increase intraarticular pressure, allows for the amount of contrast to be increased in the synovial cavity.22–25 The most widely accepted contrast medium to attain intraarticular or indirect effect must bond to the proteins weakly, have a high ionic charge to achieve an optimal fixation to the cartilage proteoglycans, and a high relaxation capacity in the proteinaceous medium.21–25
For indirect MR arthrography intravenous dimeglumine gadopentetate or an equivalent is administered at a dose of 0.1–0.2mmol/kg of weight. After the injection, the shoulder is moved passively abducting from 0° to 90° for 10min at the most, with 10–15 repetitions per minute to obtain the maximum amount of contrast in the articular fluid.
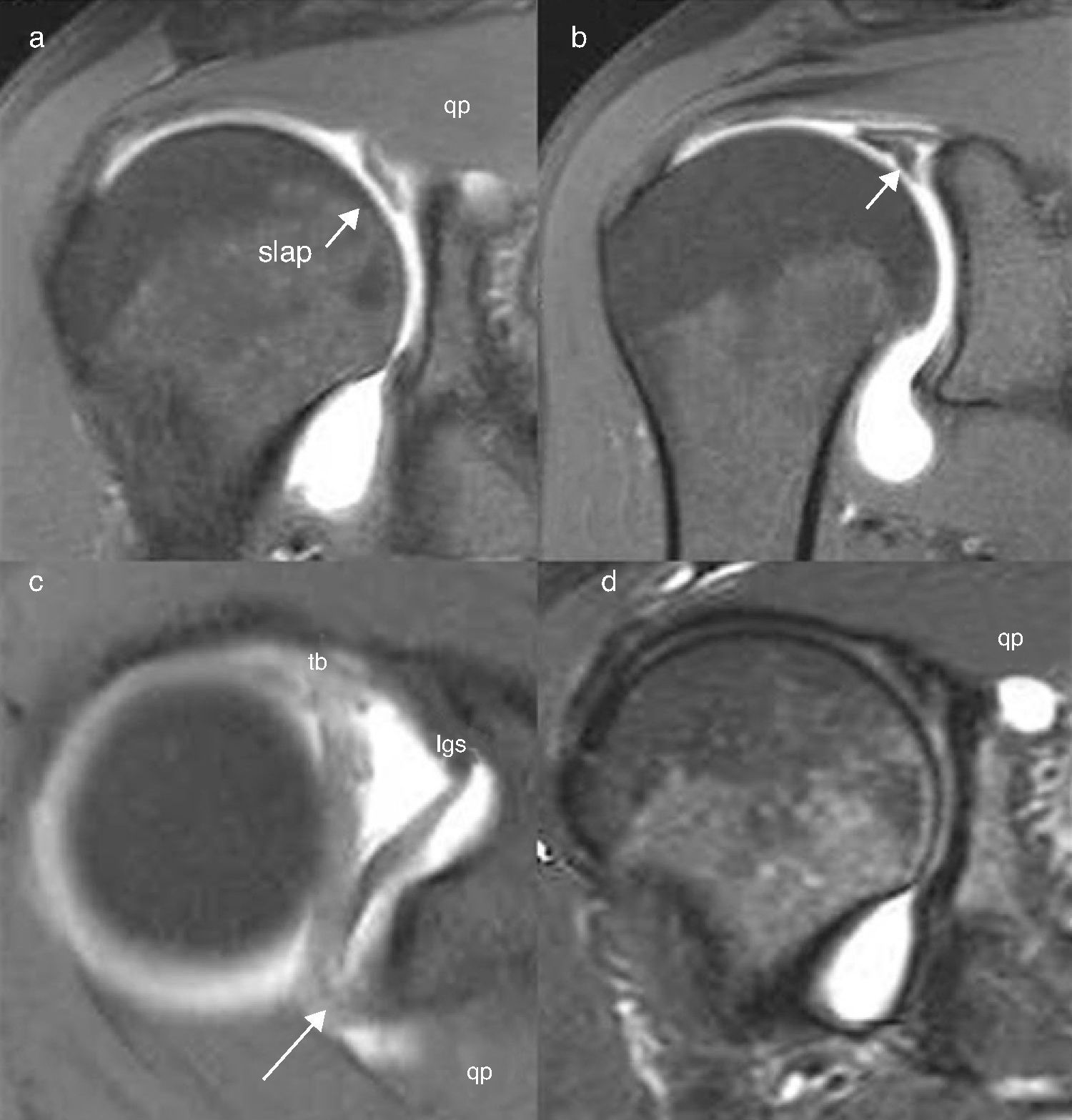
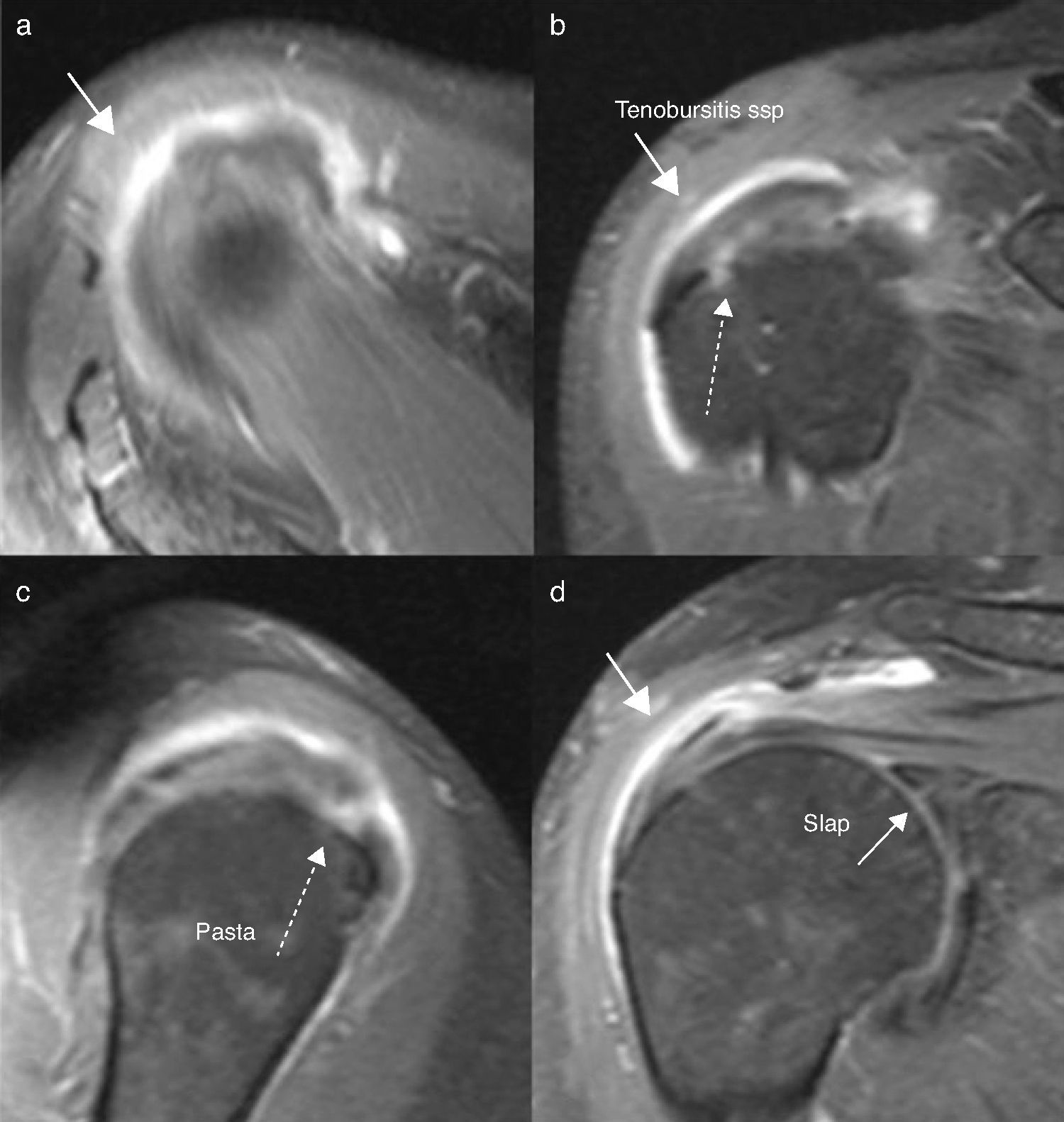
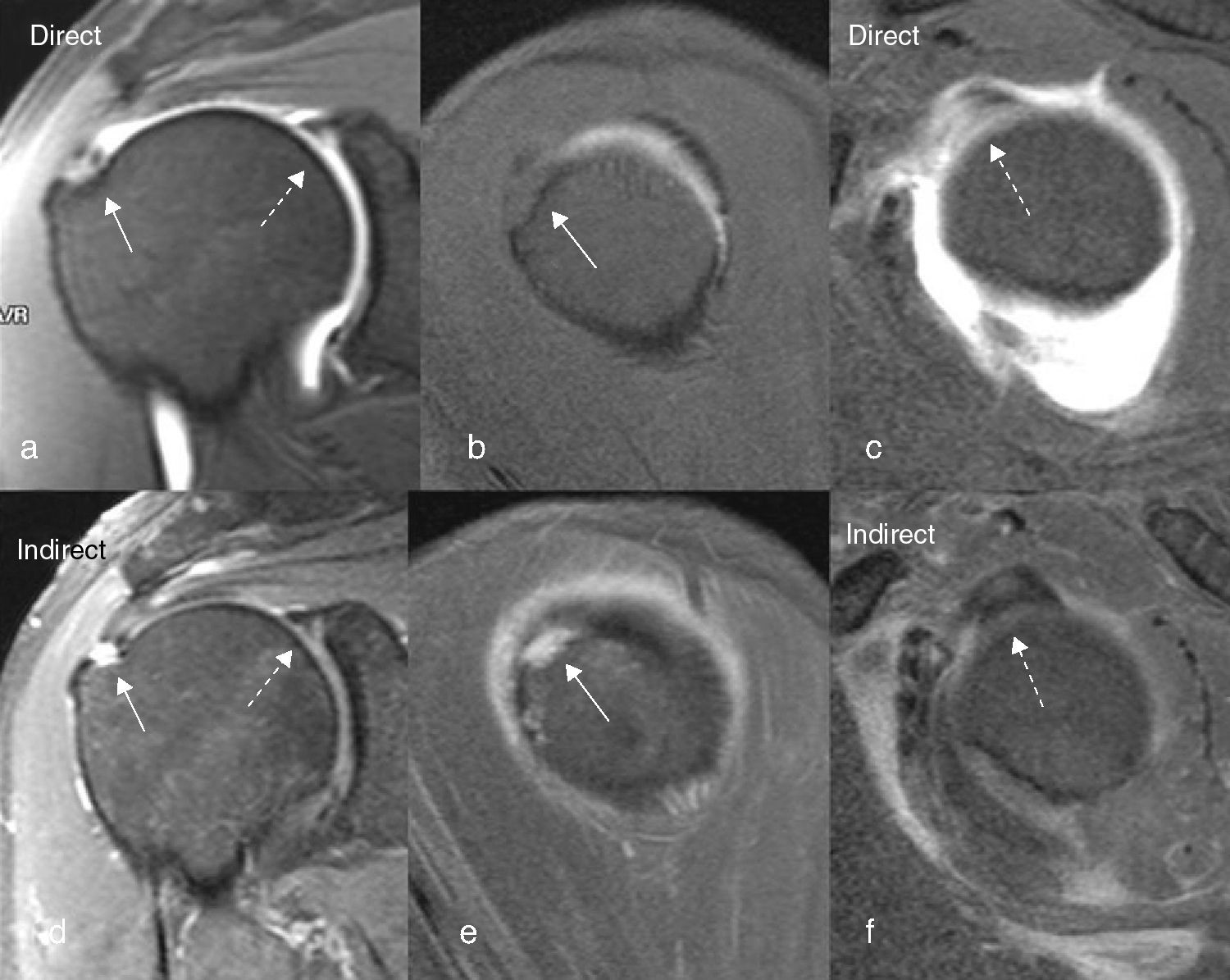
The MR study must begin not more than 30min after contrast has been injected either directly or intravenously. The protocols are different according to the experience of the centers. In our service, with 1.5-tesla equipment, for the MR arthrography studies, we use weighted sagittal oblique sequences T1 (TR: 600–800ms; TE: 15–20ms), T2 with fat saturation in the oblique coronal plane (TR: 2000ms; TE: 100ms), and T1 with fat saturation in the oblique coronal, oblique sagittal and transversal planes (TR: 600–800ms; TE: 15–20ms). The cut is 3mm thick with 1mm of space between cuts. The field of vision (FOV) ranges from 16 to 18cm and the reconstruction matrix from 256 to 512. In Figs. 1 and 2 it is possible to observe the characteristics and resolution of direct and indirect MR arthrography with this protocol, which underline complex, small structure lesions.
Direct MR arthrography. Slap II and paralabral cyst. Weighted images in T1 with fat saturation on the planes: (a) anterior coronal, (b) posterior coronal, (c) axial and (d) coronal STIR plane. Observe superior labrum oblique fissure connected to the paralabral cyst. Capsule distension and resolution are adequate. lgs: superior glenohumeral ligament; qp: paralabral cyst; tb: bicep tendon. Arrow: Slap.
Indirect MR arthrography. Slap II, subdeltoid bursitis and partial rupture of supraspinous articular surface (described as Pasta). Weighted images in T1 with fat saturation in the planes: (a) axial, (b) coronal, (c) sagittal and (d) coronal. The capsule and the adjacent soft tissue stand out adequately underlining the inflammatory process. The Pasta lesion is well defined. Thin arrow: Slap II. Thick arrow: subdeltoid bursitis. Broken arrow: Pasta.
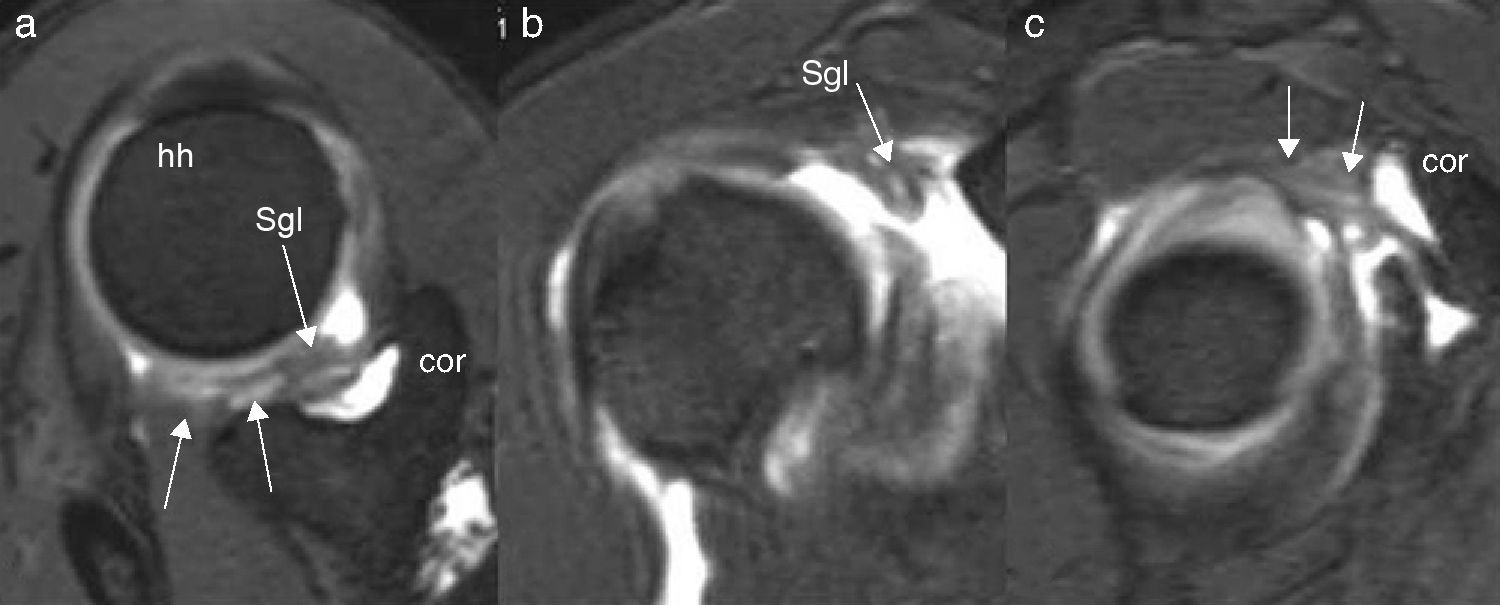
For approximately 5 years we have added high resolution volumetric sequences to all the direct or indirect MR arthrography protocols in order to achieve a better evaluation of the lesions. The sequences used get different names depending on the equipment. In Siemens equipment we use 3D Dual Echo Steady State (DESS) sequences weighted in T2 (FOV: 18cm; cut thickness: 0.8mm; TR: 21.4ms; TE: 5.9ms; 40° angle; matrix: 256×256; number of cuts: 144) and TrueFISP (T2 TRUFI 3D; FOV: 18cm; cut thickness: 0.9mm; TR: 10.41ms; TE: 4.6ms; 40° angle; matrix: 256×256; number of cuts: 60) (Fig. 3).
High-performance athlete evaluated to rule out labral lesion. Direct MR arthrography. High resolution volumetric images with T2 DESS 3D WE technique on the planes: (a) axial, (b) coronal and (c) sagittal. The arrows outline Slap II type lesion that compromises all the superior labrum, from posterior to anterior, and it expands to the superior glenohumeral ligament, forming a Slap X. hh: humeral head; cor: coracoids; sgl: superior glenohumeral ligament.
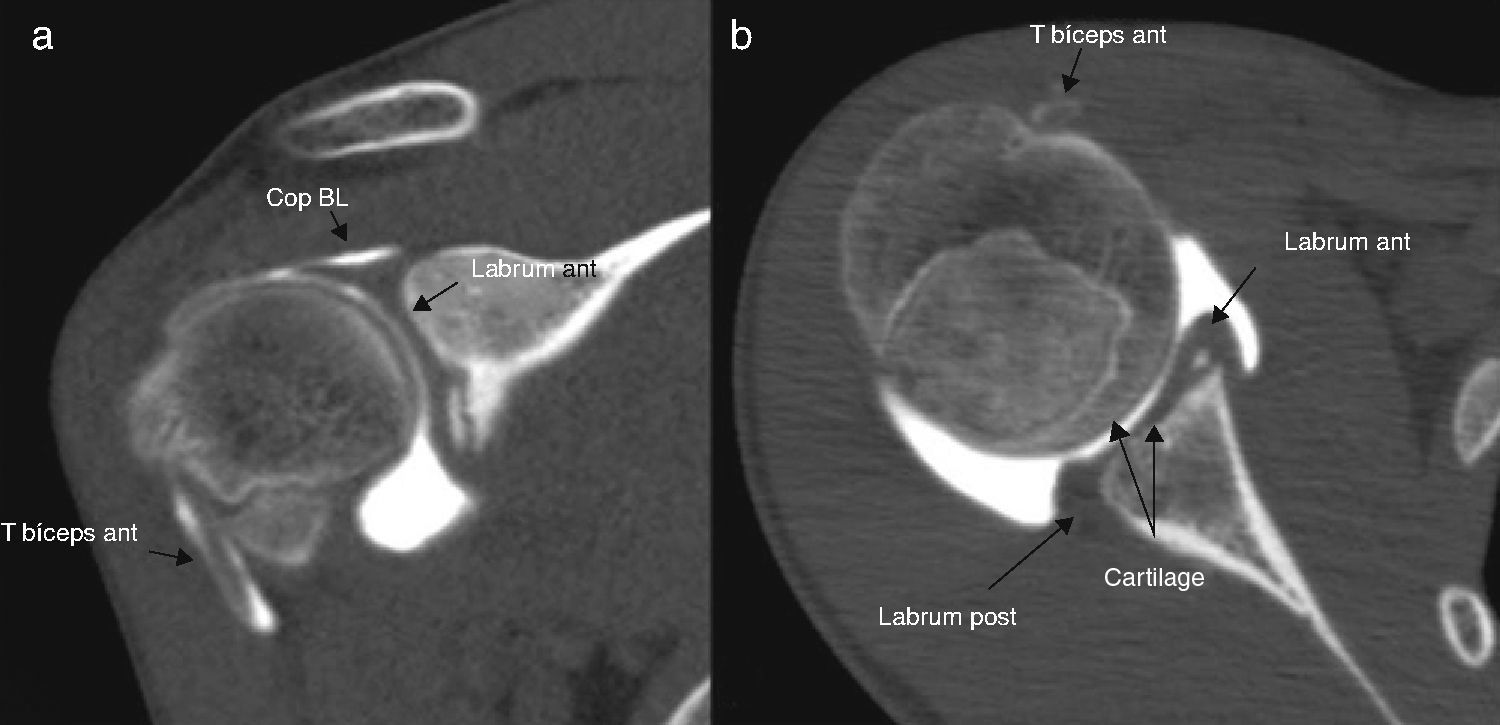
ArthroTC uses a similar method to inject the contrast, by means of fluoroscopy or other techniques. It uses iodized contrast diluted at 50% with saline in a volume similar to that of direct MR arthrography. Within the next 30min the TC is performed. When complex glenoid fractures are suspected, simple images can be acquired before contrast is injected, to the end of defining the fragments better and planning surgery.
High resolution equipment with the largest number of detectors possible are required to obtain the best multiplane reconstructions with a low isotropic thickness (between 0.5 and 0.7mm), which is essential for diagnosis. If necessary, special filters and algorithms are added to suppress artifacts (movement and metal ones among others), which improves image quality. During reading on the monitors different windows and contrasts are resorted to (Fig. 4).
CT arthrography of a 19-year-old young man with normal study. Images obtained in a 64-detector TC with multiplanar postprocess on the planes: (a) coronal and (b) axial where it is possible to observe, in spatial high resolution, the biceps tendon, articular cartilage, the bicipital-labral complex, the superior and inferior labrum, bone and muscle structures.
Complete ruptures of the rotator cuff are identified by MR with and without contrast with accuracy close to 84–100%.26–29 Partial ruptures are hard to diagnose. When they are less than 25% and are located on the tendon's articular surface they may cause enough pain to require treatment with debridement.3,30 MR without contrast has not proved to be totally satisfactory for rotator cuff examination with sensitivity between 56 and 72% and specificity of 85%.31–35
Direct MR arthrography studies for rotator cuff have a sensitivity of 84%, a specificity of 96%, and a positive predictive value of 93% and a general accuracy of 91%.30 Peh et al.36 have described sensitivity and specificity values close to 100%. For some authors, indirect MR arthrography sensitivity is 100% and specificity 77.8–88.9% with accuracy ranging 91.7–95.8%.28
The study of the labrum in all its length and in particular the superior component including the Slap lesions as well as those of the bicipital-labral complex, are hard to identify. The works performed yield sensitivity and specificity values in general that range from 82 to 92% and from 82 to 98% respectively.12,26,37,38
In a direct MR arthrography study published by Waldt et al.,11 sensitivity was 82% and specificity 98% for Slap I–IV, in keeping with other works conducted. The values in this work concurred with the types of lesions in 66%. Bencardino et al.12 obtained similar results with 89% sensitivity and 91% specificity, 90% general diagnostic accuracy and 76% correlation with Snyder's classification. Jee et al.38 obtained similar results in general, with 92% sensitivity, 92% specificity 85% accuracy for the observer who obtained the highest values. These values are better than the ones described with MR without contrast,39–41 with the exception of one publication by Connell et al.42 in which simple MR showed 98% sensitivity, 89.5% specificity and 95.7% accuracy.
Anatomical variants, including the sublabral recess and foramen, the types of insertion of the bicipital-labral complex and Buford's complex make the analysis of the affection difficult in these areas.
Indirect MR arthrography of Slap lesions in the study by Herold et al.43 shows 91% sensitivity, 85% specificity and 89% accuracy. Correlation for classification of lesions according to Snyder's description was 82%.
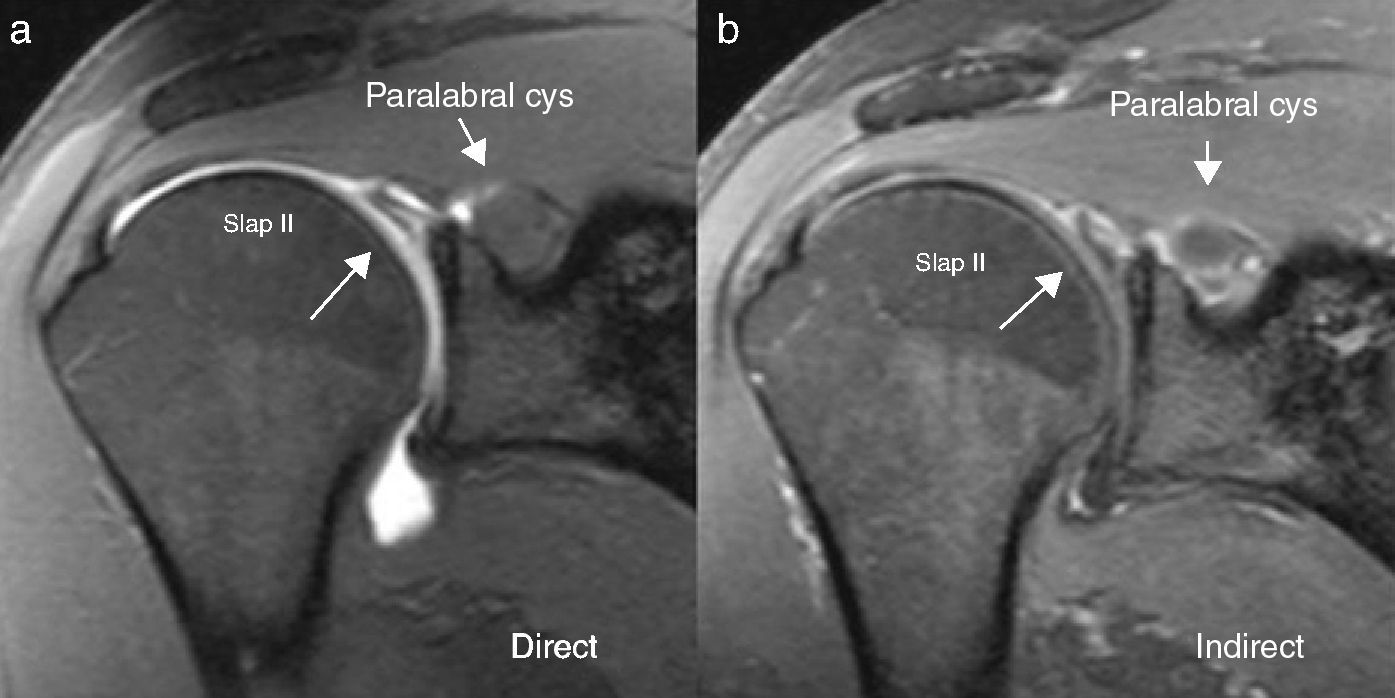
In a study conducted by the author (under process for publication), with a population of 20 patients who had initially undergone direct and then indirect MR arthrography, comparing the results with the arthroscopy or surgery findings, the hypothesis put forward was validated, where the indirect method is acceptable for diagnostic of Slap and rotator cuff lesions without any significant difference from the direct one. In said work a 78.57% sensitivity by direct MR arthrography was demonstrated for Slap in general (without specifying the type of lesion), and 85.71% by indirect MR arthrography, without any significant difference between both. Sensitivity for Slap II was 88, 89% by both methods as well as 100% for IV. Specificity for Slap in general was 66.67% by the two methods. For Slap II, specificity by direct MR arthrography was 90, 91% and for the indirect one 72, 73%. The positive predictive value for Slap did not show any significant difference (84 and 85% respectively). The negative predictive value for Slap was 57.14 and 66.67% respectively, without any significant difference. Total supraspinous rupture was diagnosed with 100% sensitivity, specificity, positive and negative predictive value by both methods. The results for “Pasta” type lesions, the intrasubstance and those of the supraspinous bursa aspect are similar. The intraobserver concord and the Kappa indexes (comparing the direct and the indirect methods by each of the three participating radiologists, obtained by blind reading), ranged from 0.6 to 0.8 for the different variables including Slap type and rotator cuff lesion. Figs. 5 and 6 illustrate the characteristics of direct and indirect MR arthrography images with the advantage that they may be compared in the same patient with a similar protocol. First the direct MR arthrography was performed and in the following 7 days, the indirect one.
Weighted sequences in T1 with fat saturation in a direct MR arthrography study on the planes: (a) coronal, and (b) and (c) sagittal and indirect MR arthrography, on the planes (d) coronal, and (e) and (f) sagittal, in the same patient and with similar protocol, with three days apart between both studies. A partial supraspinous rupture is observed in the insertion site “rim-rent” (continuous arrows) and a small Slap II (broken arrows). The particularities of each method to identify lesions are underlined.
Direct (a) and indirect MR arthrography (b) obtained in the same patient a week apart and with similar protocols. Although each method has its specific characteristics, diagnosis of Slap II and the paralabral cyst is evident in both. Notice how the cyst is defined and identified better in the indirect study.
The values described in the bibliography for CT arthrography are in some cases similar to those of other methods. For complete supraspinous rupture 99% sensitivity and 100% specificity have been described, but the values decrease a little for the infraspinous and the subscapular ones.44 Partial articular lesions must be deep in order to be detected and those of the bursa and the intrasubstance are not evaluated well with CT arthrography. Muscle atrophy, contrariwise, can be studied well. For Slap lesions, the work by Kim et al.45 using the multidetector technique showed a general sensitivity, not including type I, ranging from 94.3 to 97.7%, specificity ranging from 72.6 to 76.7%, depending on reader 1 or 2 and similar 86.3% accuracy for both readers.
Indications, advantages and disadvantages of direct magnetic resonance arthrography, indirect magnetic resonance arthrography, and computed tomography arthrographyThere is a certain consensus in the bibliography about the general indications of the studies; however, debate persists regarding which the ideal method is for given patients and lesions.
Direct MR arthrography is the examination of choice to study the superior labrum, the bicipital-labral complex, less clarified rotator cuff lesions (including partial tendinous lesions, especially the articular ones), the capsulolabral complex, the integrity of glenohumeral ligaments, the rotator interval, bicep lesions, intraarticular free bodies and postsurgical shoulder.26,27,29,37,38,46–49 The direct way is one of the most important and recognized indications for young patients, high-performance athletes or surgery candidates.26,27,29,37,38,46–49
In our experience we have observed that the direct method may have some advantages due to articular capsule distension and the input of the contrast medium in fissures and orifices, enabling to see better the normal and abnormal structures directly related with the articular cavity, but not beyond it. Contrariwise, it has the disadvantage that it makes conventional MR an invasive technique; it does not prevent exposure to ionizing radiation when fluoroscopy or TC-guided, and it increases the risk of secondary complications by the introduction of a needle into the joint. In addition, it implies that the study needs 2 different wards (when planned by fluoroscopy or TC) and, in turn, higher costs.13,50 Another disadvantage lies in the fact that it does not make it possible for intrasubstance or bursa ruptures to be observed in all the cases, which can be done with the indirect method, although with greater sensitivity than specificity, because internal tendinous inflammatory processes may increase with the contrast.28
Indirect MR arthrography has been recommended for small joints or those with large articular surface, that is, where there is more contact between the fluid and the synovial membrane. It is recommended for the shoulder due to the abundant synovial invaginations and creases.28,36,43,51–53 It makes it possible for intra and extraarticular affection to be studied. Moreover, some works defend that it is more appropriate to study lesion recurrence in patients who have undergone surgery.54 No doubt it is more useful for study patients with systemic diseases, arthropathies, infection, collections, abscesses or tumors. Just as lesions are examined in other joints with intravenous contrast, the indirect method is very useful in our service to study patients. Due to its tolerance, it is ideal for elderly patients (in general older than 50 years) or for those whose health is compromised, those for whom puncture is difficult or contraindicated. The lower cost of the study, as well as its ease of logistic execution must be considered when making a decision.
The main disadvantages of MR indirect arthrography include no articular capsule distension and less penetration in articular tissues, which may decrease diagnostic resolution in some cases. Lack of interpretation experience limits the use of the method as a routine procedure in many centers, therefore, training and experience are necessary so as not to overvalue the findings and generate false positives.
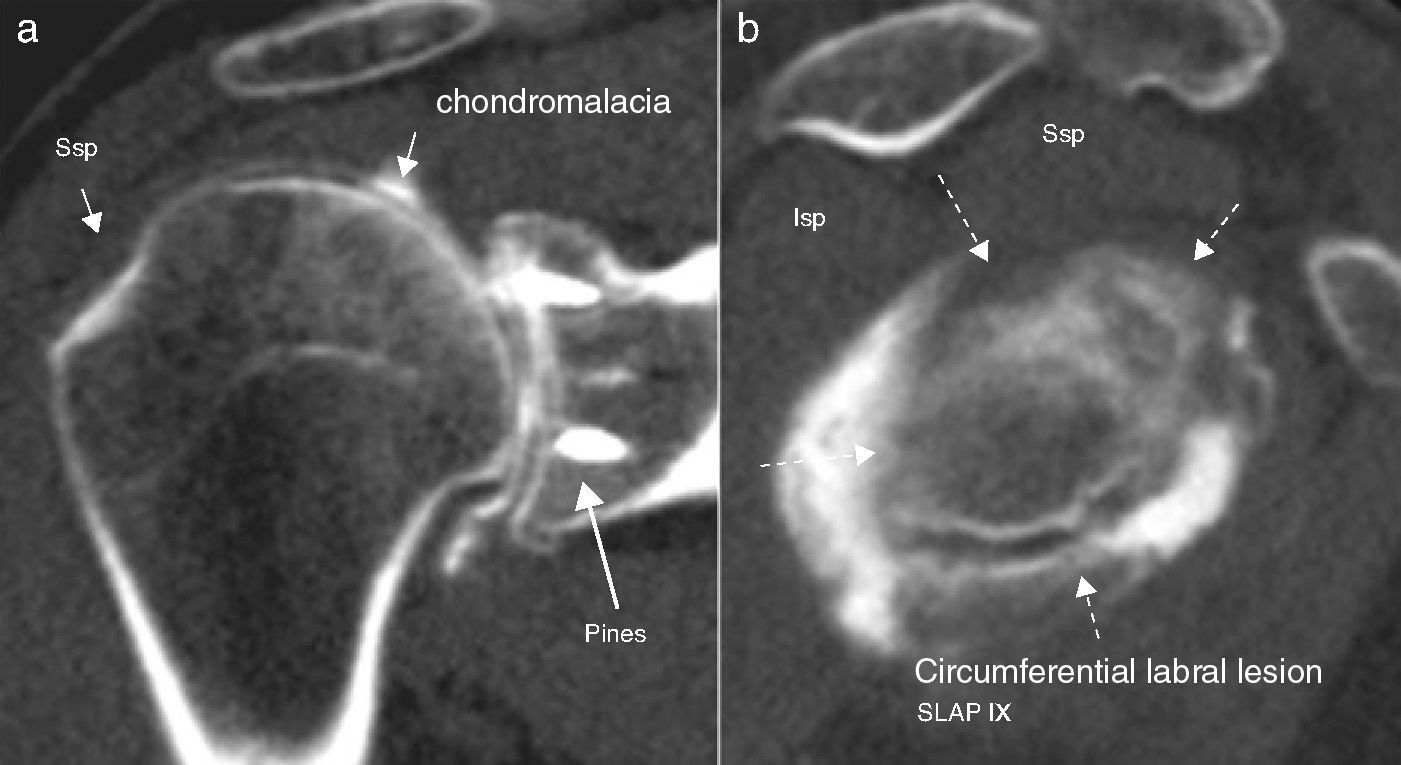
CT arthrography is indicated for patients who cannot undergo MR as a first option due to the presence of pacemakers, antecedents of reaction to paramagnetic contrast, claustrophobia or metal artifacts. It may offer interesting results in patients with soft-tissue and fracture combined lesions. Furthermore, it may be used with limitations where MR equipment is not available (Fig. 7).
CT arthrography of a 49-year-old male with previous surgery. Images obtained with a 64-detector TC with multiplanar post-process on the planes: (a) coronal and (b) sagittal. The study was made on the MR due to the artifacts. It is possible to observe advanced diffuse chondromalacia and a circumferential labral lesion (Slap IX); partial supraspinous rupture without detachment of insertion and without advance atrophy, fundamental information for treatment. Observe the adequate spatial resolution. Isp: infraspinous; Ssp: supraspinous.
We have presented the most common shoulder lesions that require contrasted studies such as partial rotator cuff ruptures and labral lesions. The different types of examinations have been described, including direct and indirect MR arthrography and CT arthrography, underlining their technique, indications, advantages and disadvantages. Likewise, several works published on the diagnostic sensitivity, specificity and accuracy of each of the modalities have been revised.
We share the consensus described in the bibliography recommending direct MR arthrography for labrum lesions and partial rotator cuff ruptures, mainly for young patients (under 50 years of age), high-performance athletes or surgery candidates and, contrariwise, we consider that the indirect method is a very good choice for older people, on whom an early surgery is not necessary due to the clinical manifestations, in postsurgical patients, in infection, regional or systemic inflammatory affection, mass, tumor or when it is not possible to perform the direct method.
CT arthrography is also a valuable study, especially to evaluate the labrum and the cartilage in patients who cannot undergo MR (pacemakers, claustrophobia, and equipment availability) or in those cases of ferromagnetic artifacts in which MR quality is bad.
According to our experience and the bibliography published, where it is not possible to establish a significant difference that disqualifies completely a given study modality, we recommend accepting the advantages of all these methods. The most important issue is to use appropriately the resources available in each place so as to apply them in the best possible way on each patient, taking into account their age, probable medical or surgical treatment and the diseases related with the affection, including the conditions after the surgery and the complications. We do not believe that rigid positions or behaviors where some diagnostic techniques are arbitrarily excluded help solve the patients’ problems restricting creativity, particularly in countries where limitation of resources is ever-present.
Ethical responsibilitiesProtection of people and animalsThe authors declare that the procedures followed comply with the ethical standards of the responsible human experimentation committee and that they are in accordance with the World Medical Association and the Helsinki Declaration.
Data confidentialityThe authors declare that that no patient data appear in this article.
Right to privacy and informed consentThe authors declare that that no patient data appear in this article.
Conflict of interestsThe author declares that he has no conflict of interests.
Please cite this article as: Restrepo González R. Artroresonancia directa, indirecta y artrotomografía para lesiones del mango rotador y Slap. Estado actual. Radiología. 2013;55:283–293.