Hip and groin pain is a common clinical problem. Multiple causes can generate hip or groin pain, often sharing clinical and demographic characteristics. Diagnostic imaging tests play an important role in the etiological diagnosis. New forms of extra-articular hip impingement have recently been recognized as a cause of hip pain and limited function especially in young active patients. These conditions include ischiofemoral impingement, anterior inferior iliac spine and subspine impingement, iliopsoas impingement and greater trochanteric-pelvic impingement. In general, they are caused by a mechanical conflict with an abnormal or excessive contact between the proximal femur and pelvis and/or soft tissue between them. In this manuscript we review the physiopathology, clinical presentation, the most common radiologic findings and treatment of these forms of extra-articular hip impingement.
El dolor inguinal o de cadera es un motivo de consulta muy frecuente. Debido a las múltiples causas que pueden generarlo, y a que en muchas ocasiones comparten características clínicas y demográficas, las pruebas de imagen desempeñan un papel complementario en el diagnóstico etiológico. Se han descrito nuevas formas de atrapamiento extraarticular de la cadera como causa de dolor y limitación funcional, en especial en pacientes jóvenes activos. Incluyen el atrapamiento isquiofemoral, el choque subespinoso o de la espina iliaca anteroinferior, el atrapamiento del iliopsoas y el choque pélvico-trocantéreo. De forma general, se deben a un problema mecánico que conduce al contacto anormal o excesivo entre el fémur proximal y la pelvis ósea, o las partes blandas interpuestas. Realizamos una revisión actualizada de estas formas de atrapamiento extraarticular de la cadera, describiendo la fisiopatología, las manifestaciones clínicas, los hallazgos radiológicos más comunes y el tratamiento.
Hip and groin pain is a common clinical problem that can be due to a great variety of causes of very different physiopathology but often sharing clinical and demographic characteristics, which is why the final etiological diagnosis is a challenge.
Hip impingement – whether intra-articular (femoroacetabular impingement) or extra-articular, has recently been described as a cause of hip pain and limited function especially in young active patients.
Back in 2003, Ganz et al.1 described femoroacetabular impingement (FAI) as the “abnormal contact between the femur and the acetabular cavity secondary to morphological alterations, or an articular movement in an excessive or supraphysiological range”. The FAI syndrome has recently been redefined as a clinical condition associated with the movement of the hip representing a premature symptomatic contact between the femur and the acetabulum, and whose diagnosis requires the presence of symptoms and findings that are compatible both in the physical examination and the imaging modalities.2
During the last few years, new forms of extra-articular impingement have been reported including ischiofemoral impingement, anterior inferior iliac spine and subspine (AIIS) impingement, iliopsoas impingement and greater trochanteric-pelvic impingement.
In general, they are caused by a mechanical conflict with an abnormal or excessive contact between the proximal femur and the osseus pelvis and/or the soft tissues between them.3
In the diagnosis of these forms of extra-articular hip impingement, the clinical presentation and the dynamic physical examination are essential. The role of the imaging modalities is to support the clinical suspicion and even, sometimes, participate in the treatment whether guiding the percutaneous administration of therapy, or assisting the traumatologist in his surgical planning.
It is not rare to find compatible radiologic findings in asymptomatic patients and, on the other hand, the border lines between the morphological changes that can be the pathological substrate and the normality variate are still very confusing. This is why we should emphasize the need to be particularly cautious in the radiologic diagnosis of these syndroms only in order to avoid unnecessary interventions.
There is a growing interest to define the predisposing factors, the physiopathological mechanisms, and the imaging findings of these forms of extra-articular hip impingement, yet, today, there are still numerous things we simply do not understand, which is why new studies are needed to help us improve our understanding and diagnostic accuracy through the validation of clinical and radiologic criteria.3–7
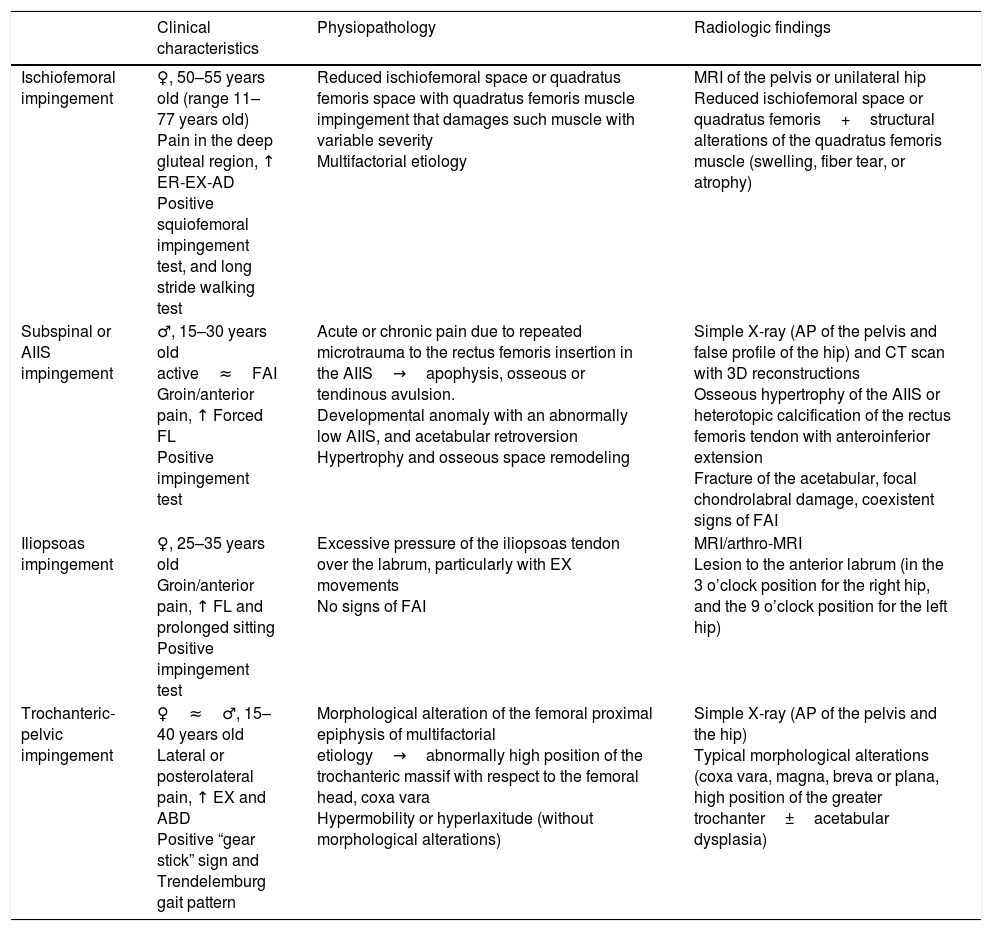
In this paper we will be providing an updated review on these forms of extra-articular hip impingement describing its physiopathology, clinical presentation, and its most common radiologic findings; finally, we will be discussing the treatment of these forms of extra-articular hip impingement (Table 1).
Summary of the different forms of extra-articular hip impingement.
| Clinical characteristics | Physiopathology | Radiologic findings | |
|---|---|---|---|
| Ischiofemoral impingement | ♀, 50–55 years old (range 11–77 years old) Pain in the deep gluteal region, ↑ ER-EX-AD Positive squiofemoral impingement test, and long stride walking test | Reduced ischiofemoral space or quadratus femoris space with quadratus femoris muscle impingement that damages such muscle with variable severity Multifactorial etiology | MRI of the pelvis or unilateral hip Reduced ischiofemoral space or quadratus femoris+structural alterations of the quadratus femoris muscle (swelling, fiber tear, or atrophy) |
| Subspinal or AIIS impingement | ♂, 15–30 years old active≈FAI Groin/anterior pain, ↑ Forced FL Positive impingement test | Acute or chronic pain due to repeated microtrauma to the rectus femoris insertion in the AIIS→apophysis, osseous or tendinous avulsion. Developmental anomaly with an abnormally low AIIS, and acetabular retroversion Hypertrophy and osseous space remodeling | Simple X-ray (AP of the pelvis and false profile of the hip) and CT scan with 3D reconstructions Osseous hypertrophy of the AIIS or heterotopic calcification of the rectus femoris tendon with anteroinferior extension Fracture of the acetabular, focal chondrolabral damage, coexistent signs of FAI |
| Iliopsoas impingement | ♀, 25–35 years old Groin/anterior pain, ↑ FL and prolonged sitting Positive impingement test | Excessive pressure of the iliopsoas tendon over the labrum, particularly with EX movements No signs of FAI | MRI/arthro-MRI Lesion to the anterior labrum (in the 3 o’clock position for the right hip, and the 9 o’clock position for the left hip) |
| Trochanteric-pelvic impingement | ♀≈♂, 15–40 years old Lateral or posterolateral pain, ↑ EX and ABD Positive “gear stick” sign and Trendelemburg gait pattern | Morphological alteration of the femoral proximal epiphysis of multifactorial etiology→abnormally high position of the trochanteric massif with respect to the femoral head, coxa vara Hypermobility or hyperlaxitude (without morphological alterations) | Simple X-ray (AP of the pelvis and the hip) Typical morphological alterations (coxa vara, magna, breva or plana, high position of the greater trochanter±acetabular dysplasia) |
ABD: abduction; AD: adduction; AP: anteroposterior; FAI: femoroacetabular impingement; AIIS: anterior inferior iliac spine and subspine; EX: extension; FL: flexion; ER: external rotation; MRI: magnetic resonance imaging; CT scan: computed tomography scan.
The ischiofemoral impingement was first described in patients with no history of arthroplasty back in 20088,9 and includes hip pain attributed to the space between the ischial tuberosity of the hamstring muscle insertion, and the lesser trochanter, with intermittent repetitive compression of the quadratus femoris muscle.3,6,10
The ischiofemoral space can, in turn, be assessed through the assessment of two spaces (measured on an axial plane at the lesser trochanter level):
- -
The ischiofemoral space (IFS) is defined as the shortest distance between the ischial tuberosity and the lesser trochanter.
- -
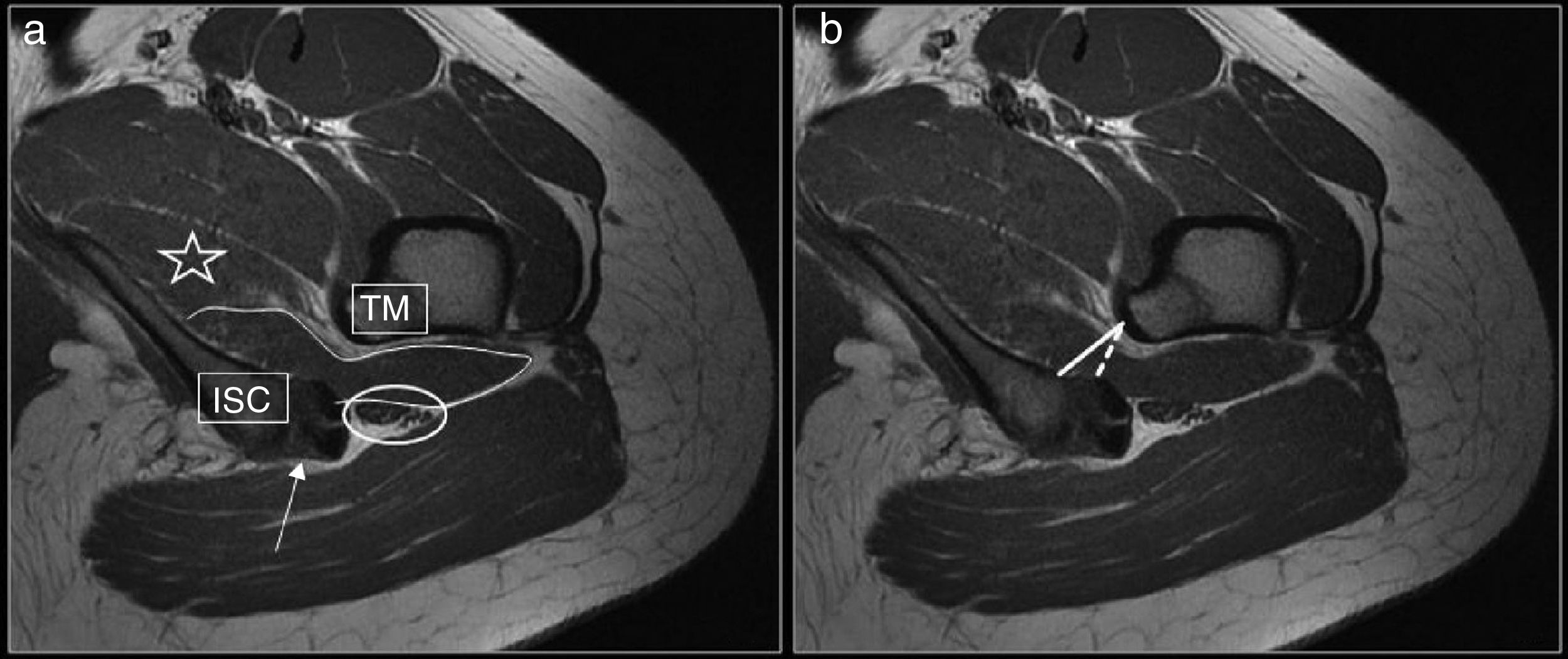
The quadratus femoris space (QFS) is the narrowest space crossed by the quadratus femoris muscle outlined by the lateral side of the harmstring tendons (mainly the semimembranous tendon) and, laterally, by the lesser trochanter or the medial margin of the psoas tendon, or both11 (Fig. 1).
Figure 1.T1-weighted MRI on the axial plane. Anatomical relations of the ischiofemoral space (a) and differentiation between the ischiofemoral space and the quadratus femoris space (b). Quadratus femoris muscle (outlined by the straight line) in the ischiofemoral space located between the greater trochanter (GT) and the ischium (ISC). Tendinous insertion of the hamstrings (white arrow). Sciatic nerve (circle). External obturator (star). Ischiofemoral space (straight line). Quadratus femoris space (dotted line).
(0.24MB).
Although the limits of normality for these two spaces have not been standardized yet, in several case control studies published during the last few years it has been confirmed that in symptomatic patients, the IFS, and the QFS are significantly shorter than in asymptomatic patients.11–13
In a meta-analysis conduct by Singer et al.,14 they say that there is a strong correlation between the narrowing of the IFS and the QFS and the presence of swelling or atrophy in the quadratus femoris muscle in the context of a painful hip, but still the isolated presence of narrowing in these two spaces is not enough to achieve the diagnosis. Also, they suggest as normality thresholds, measurements of 15mm for the IFS and 10mm for the QFS.14 In the past, other studies11,12 have suggested normal measurements around 20mm, and 10mm, respectively. However, we should take into account that only from the quantitative assessment of these spaces as fixed measurements we cannot achieve a diagnosis of ischiofemoral impingement since, in a given patient, they can vary substantially based on the degree of hip rotation, abduction, and extension at which the images are acquired.15–17
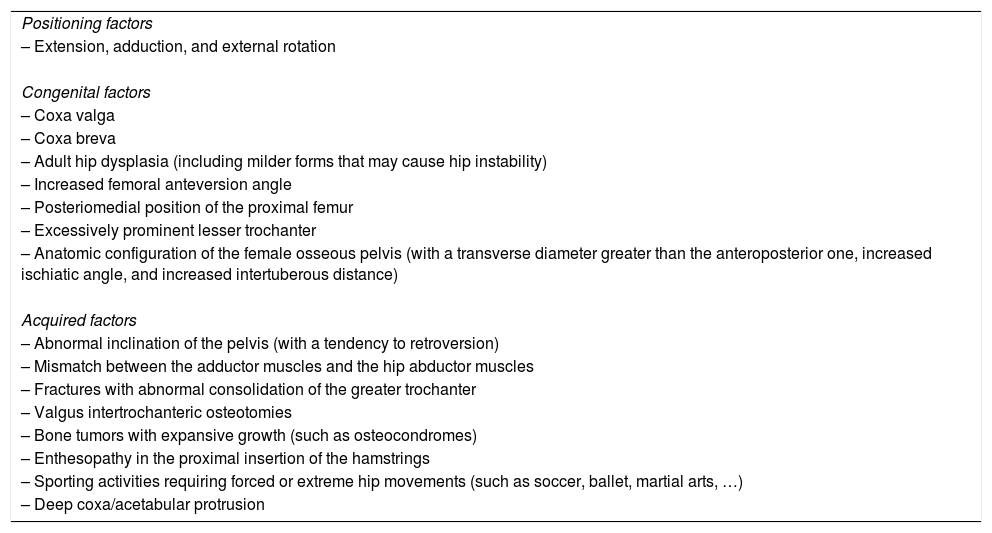
Numerous causes and predisposing factors that may contribute to the narrowing of the IFS have been reported. They can be categorized into positional, congenital, or acquired factors10–12,17–20 (Table 2).
Etiological and predisposing factors of ischiofemoral impingement.
| Positioning factors |
| – Extension, adduction, and external rotation |
| Congenital factors |
| – Coxa valga |
| – Coxa breva |
| – Adult hip dysplasia (including milder forms that may cause hip instability) |
| – Increased femoral anteversion angle |
| – Posteriomedial position of the proximal femur |
| – Excessively prominent lesser trochanter |
| – Anatomic configuration of the female osseous pelvis (with a transverse diameter greater than the anteroposterior one, increased ischiatic angle, and increased intertuberous distance) |
| Acquired factors |
| – Abnormal inclination of the pelvis (with a tendency to retroversion) |
| – Mismatch between the adductor muscles and the hip abductor muscles |
| – Fractures with abnormal consolidation of the greater trochanter |
| – Valgus intertrochanteric osteotomies |
| – Bone tumors with expansive growth (such as osteocondromes) |
| – Enthesopathy in the proximal insertion of the hamstrings |
| – Sporting activities requiring forced or extreme hip movements (such as soccer, ballet, martial arts, …) |
| – Deep coxa/acetabular protrusion |
Ischiofemoral impingement is more prevalent in middle-aged women (50–55 years). Patients complain of groin pain, or pain in the deep gluteal region that increases with movements of external rotation with extension and abduction of the hip.21 When the impingement is secondary to extreme movements of the hip such as what happens with activities like dancing or performing martial arts … the onset of symptoms may be more acute. It is not rare to see pain radiating from the posterior side of the thigh all the way up to the knee due to irritation of the sciatic nerve. Sometimes patients may complain of a snapping or blocking sensation and they can experience limitations in situations of prolonged sitting and while performing activities of daily living—usually long walks.7,16,18,22
Clinical tests have been described for this condition including the ischiofemoral impingement test (considered positive when in the lateral decubitus position on the painful hip, the patient's pain can be reproduced through the passive extension and abduction of the affected hip), and the long stride walking test (considered positive when the patient's pain is reproduced through the extension of the hip when taking long strides, and is alleviated with short steps or abduction of the hip).16,18
When it comes to the radiologic findings of the ischiofemoral impingement, one simple X-ray of the pelvis or the hip usually looks normal, although, at times, we may find structural alterations conditioning the narrowing of the IFS such as coxa valga, coxa profunda, exostosis, … or chronic osseous changes in patients with long-term clinical manifestations such as sclerosis or subcortical cysts in the or the lesser trochanter.4,10,18
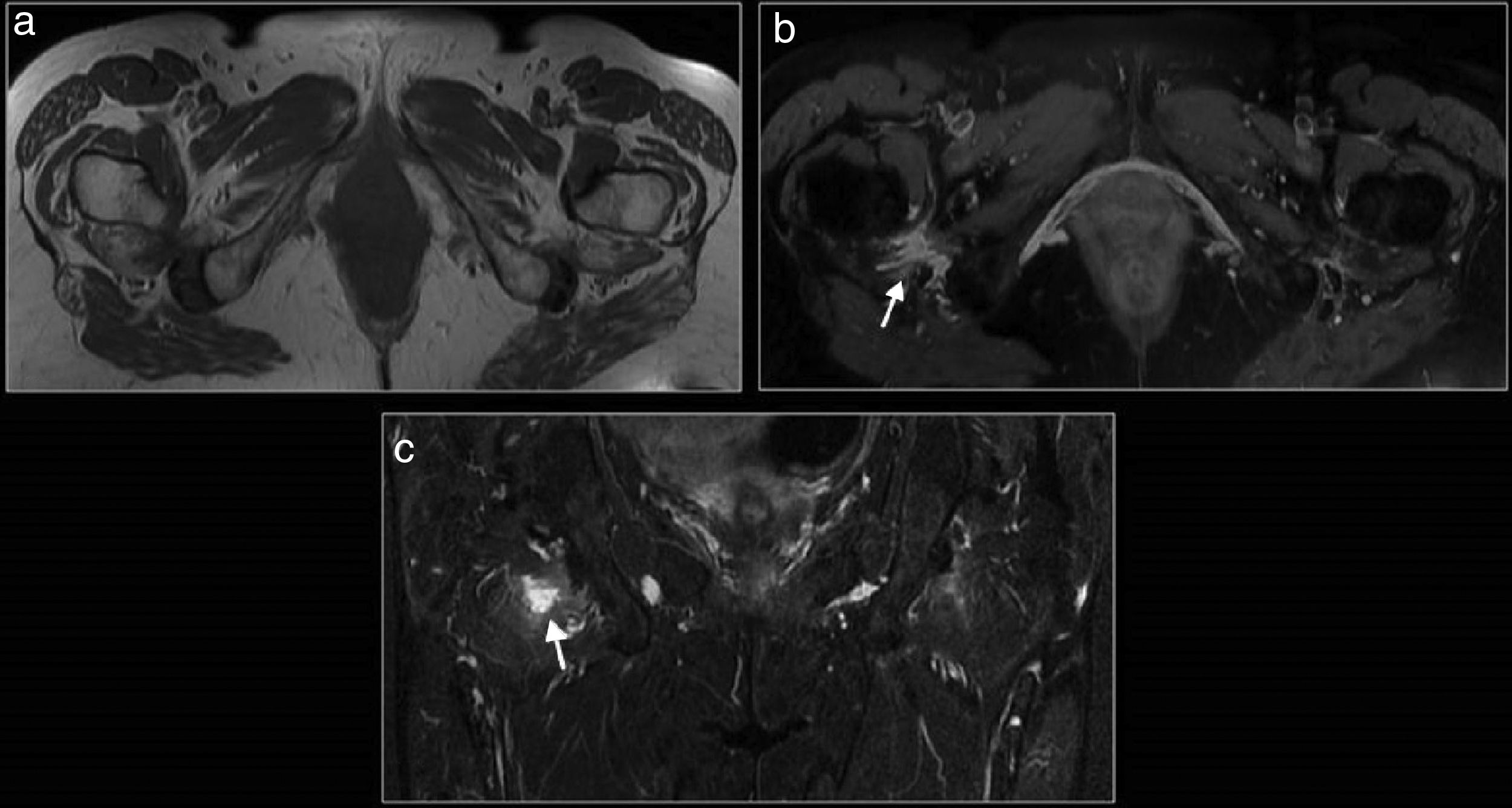
The MRI of the pelvis or the unilateral hip is the imaging modality of choice for the diagnosis of ischiofemoral impingement. The findings suggestive of the diagnosis are a reduced IFS or QFS together with signal alterations of the quadratus femoris muscle. These alterations of the quadratus femoris muscle go from swelling (in variable grade from mild to moderate) to fiber tears that usually happen in the area of maximum narrowing of the IFS. In patients with long-term clinical presentations, significant atrophy with fat infiltration from the quadratus femoris muscle can be identified. Findings may be bilateral in up to 30% of the cases3 (Figs. 2 and 3).
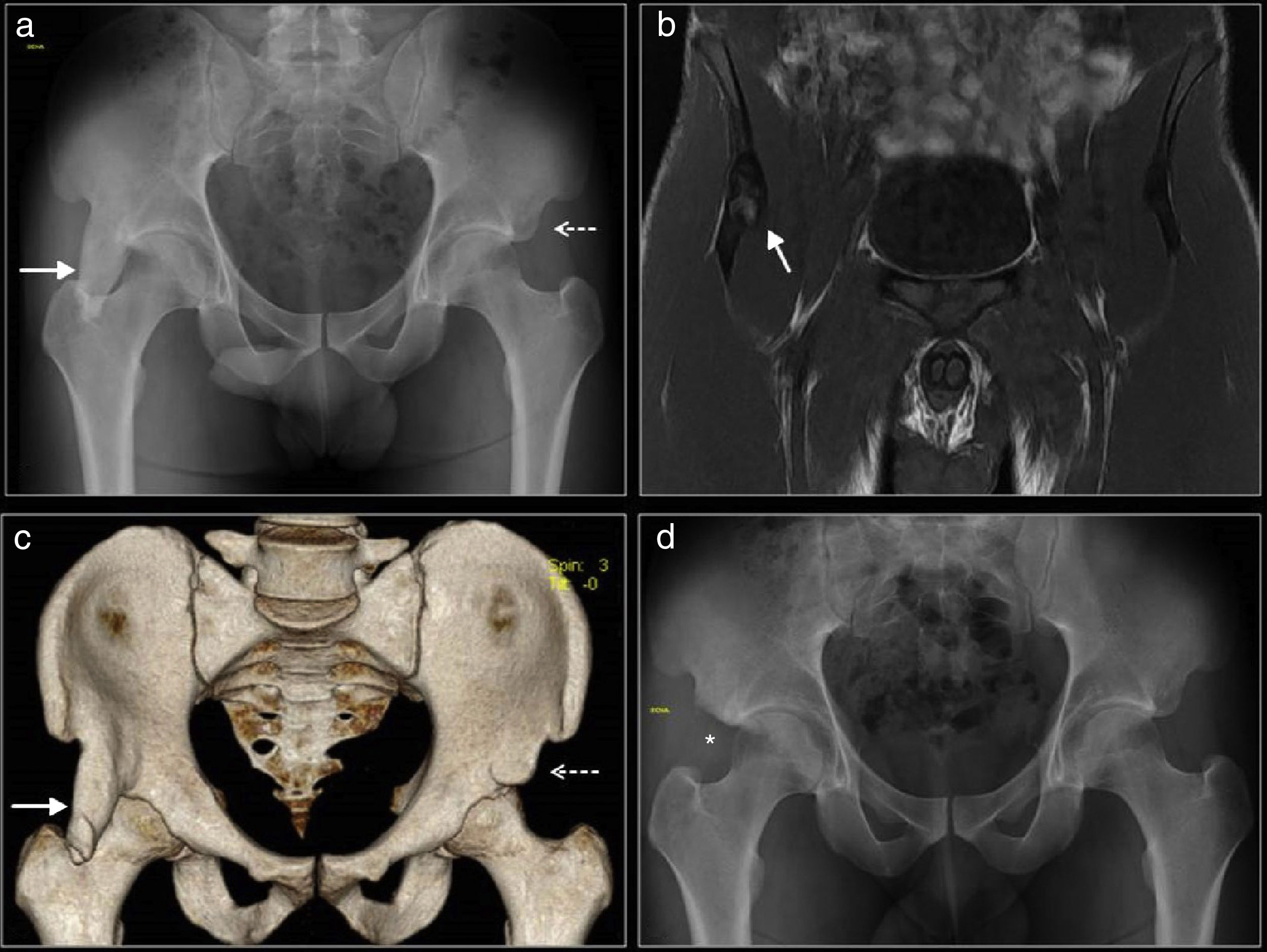
Forty-two year-old-woman with long-term left mechanical coxalgy radiating to her knee. The CT scan (a) shows the asymmetric reduction of the ischiofemoral space of her left hip (dotted lines). MRIs with STIR sequences (b), fat-suppressed PD sequences (c) and T1-weighted images (d) showing atrophy of the left quadratus femoris muscle with fiber swelling in the region of greater space narrowing (arrows in b and c), and mass effect on the left sciatic nerve (arrow in d).
Ischiofemoral impingement. Sixty-two year-old-woman with long-term pain in her right gluteal region radiating to her thigh that gets worse when sitting and has been more painful during the last few weeks. MRIs with T1-weighted sequences (a), T2-weighted with fat suppresion (b) and STIR sequences (c) showing a reduced quadratus femoris space with atrophy and rupture of the quadratus femoris mucle on its right side (arrows in b and c).
Other signs we may find are swelling around the iliopsoas tendon, swelling or tendinopathy of the harmstrings, osseous swelling, or chronic changes (sclerosis, subcortical cysts, …) in the ischium or the lesser trochanter, and the formation of neural bursae4,6,10–12,16 (Fig. 4).
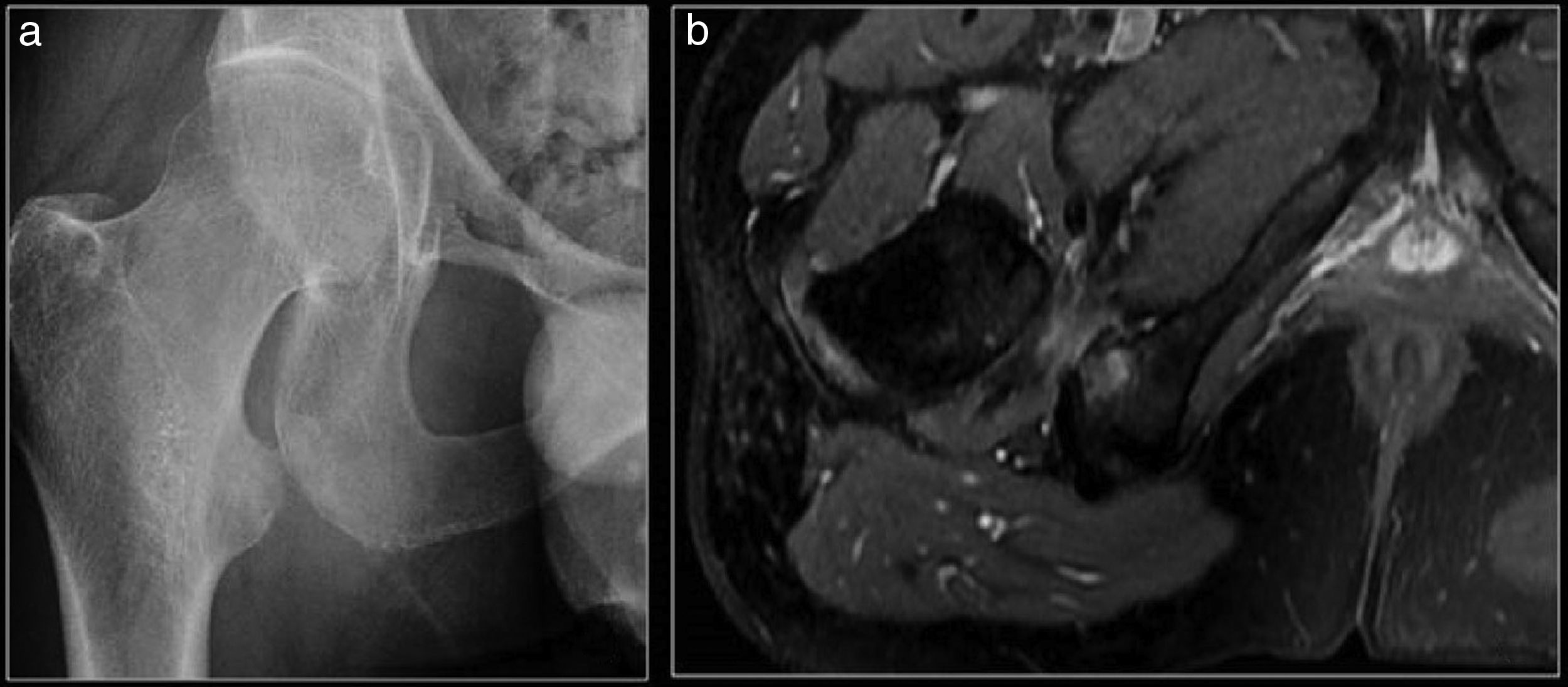
Ischiofemoral impingement. Forty-five year-old-male with right groin pain. (a) Simple X-ray of his hip showing irregularity, and sclerosis on the lesser trochanter and the ischion. (b) MRI with STIR sequences showing a reduced ischiofemoral space, swelling in the quadratus femoris muscle, and osseous swelling in the ischion.
It is essential to make a correlation between the radiologic data and the patient's clinical manifestations since the narrowing of the IFS, whether associated or not with alterations of the quadratus femoris muscle, may be found in asymptomatic patients.14,23–25
On the other hand, very symptomatic patients not always have the narrowest IFS of all; as a matter of fact, it is not rare to find patients with narrowing of their IFS and swelling of the quadratus femoris muscle in both hips complaining of pain in one hip only.6,7,11
This is why if we wish to make reliable diagnoses of the ischiofemoral impingement condition, there should be narrowing in one or both spaces (IFS/QFS), structural alterations (swelling or atrophy) in the quadratus femoris muscle, and painful clinical manifestations in the homolateral hip.14
The main differential diagnosis should be established with one traumatic strain or tear of the quadratus femoris muscle. In these cases, there is usually a clear traumatic history, no narrowing of the IFS, and the muscle tear usually occurs in the myotendinous junction region.6,8,26
When it comes to management, the initial therapy is usually conservative with restriction of the physical activity, rehabilitation, and pharmacologic treatment with anti-inflammatory drugs. The following therapeutic step in the management of the IFS is the ultrasound-guided or CT-guided local administration of corticoids, local anesthetic drugs, or irritating substances (prolotherapy).7,13,16,27,28 This measure can also be used with diagnostic purposes in questionable cases, or cases with atypical clinical manifestations, since symptomatic relief has been reported.10,13,16,18
In cases with clinical manifestations that are refractory to conservative therapy, surgery may be an option through decompression of the IFS by resection of the lesser trochanter, and release or debridement of the quadratus femoris muscle.5,7,18,22,29
Anterior inferior iliac spine and subspine impingementThe AIIS impingement is a relatively recent clinical-radiologic diagnosis.30 It is due to a mechanical problem following an altered position or morphology of the AIIS that impacts the distal femoral neck, especially when flexing the hip joint, causing osseous impingement, soft-tissue interposition, or both.4–6,31,32
Carton and Filan32 distinguish between AIIS impingement with an extra-articular location only from the subspine impingement that follows a structural alteration of the subspinal space, located between the inferior margin of the AIIS and the acetabular margin which is, basically, of intra-articular location. Both forms of impingement can coexist and share clinical and demographic characteristics, yet the radiologic manifestations and management are completely different.7,21,32,33
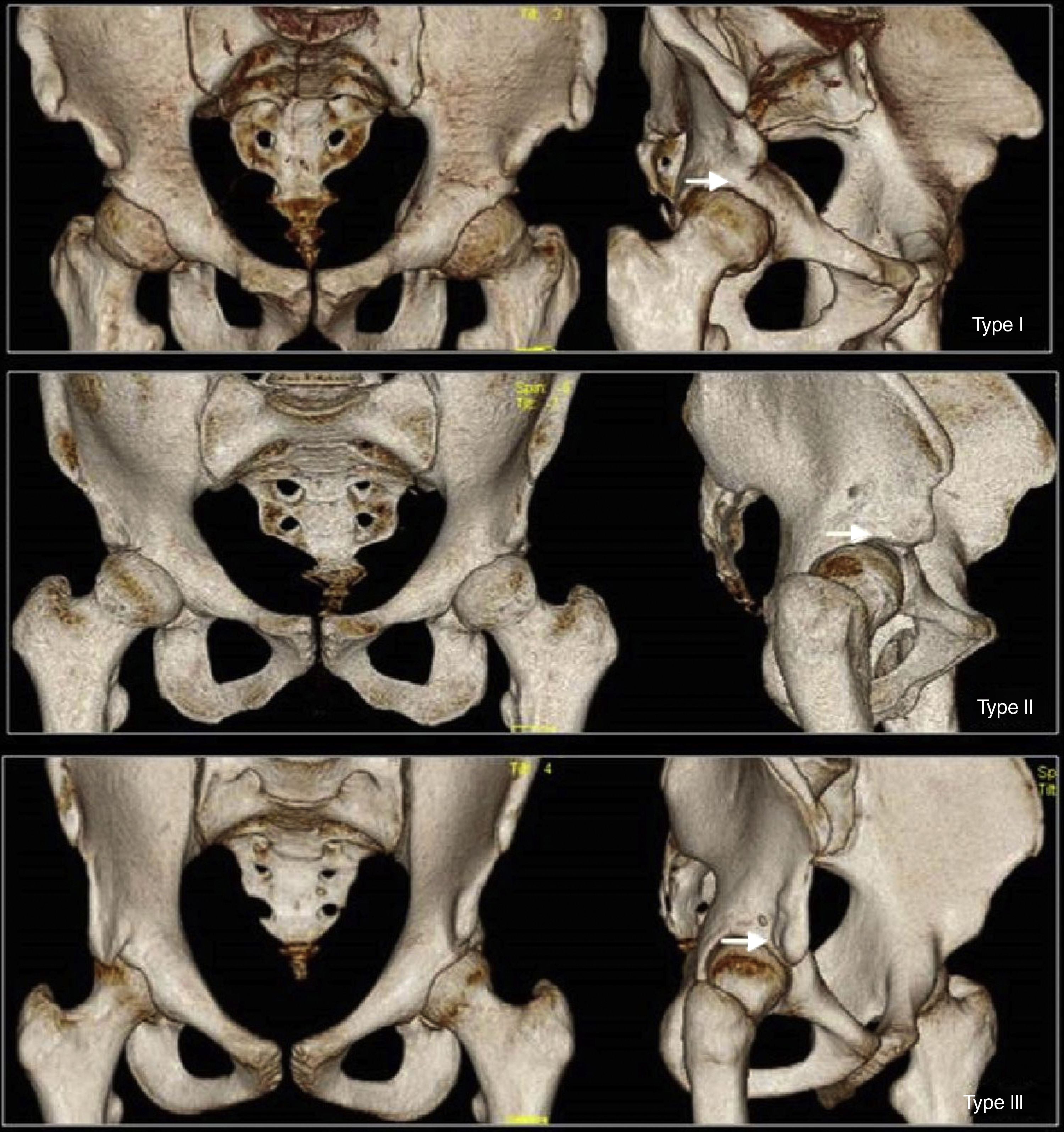
The AIIS is located cranially to the anterosuperior acetabular rim, and it is where the direct tendon of the rectus femoris muscle and the tendon of the iliocapsularis muscle originate, and may have a variable morphology. Hetsroni et al.34 propose a tree type-method for the morphological classification of the AIIS based on the relations between the AIIS and the anterosuperior acetabular rim: type I—where the iliac crest cortical bone located between the inferior level of the AIIS and the anterosuperior acetabular rim is smooth, without osseous prominence; type II—where one prominent AIIS reaches the level of the acetabular rim; and type III—where one prominent AIIS extends caudally to the acetabular rim (Fig. 5). Based on this classification, type I morphology would be considered normal, and types II and III would associate limitation of movement based on the generation of symptoms, type II in the subspinal impingement, and type III in the AIIS impingement.21,32–35
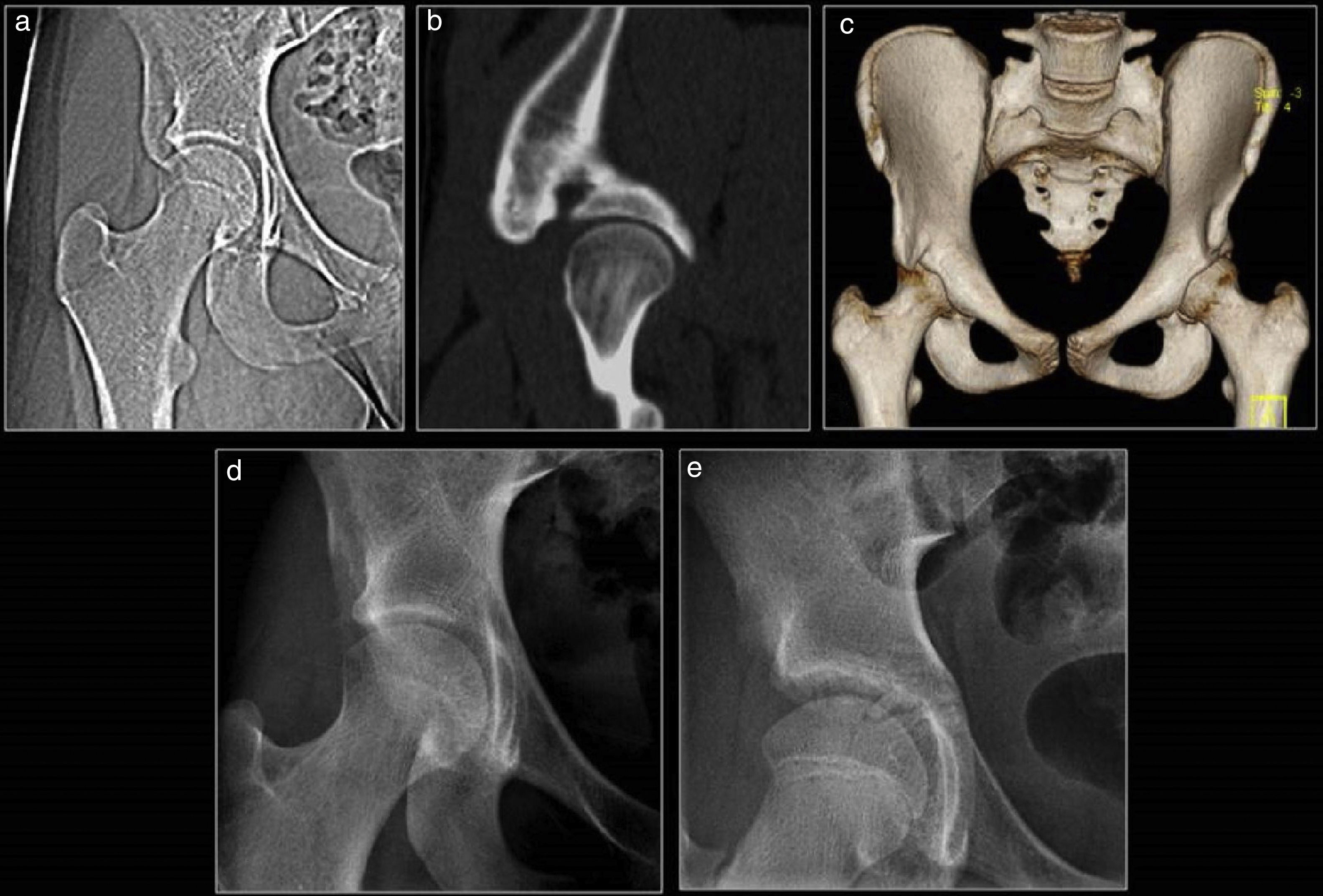
CT scans with 3D reconstructions. Types of anteroposterior ilical spine (AIIS) based on Hetsroni's classification. Type I: the AIIS has normal size and the iliac crest cortical bone located between the inferior level of the AIIS and the anterosuperior acetabular rim is smooth, without osseous prominence (arrow); type II: the AIIS is prominent and reaches the level of the acetabular rim (arrow); and type III: the AIIS is elongated and extends caudally to the acetabular rim (arrow).
In their study, Balazs et al.36 say that there is a high percentage of individuals with type II and III asymptomatic AIIS, and that Hetsroni's classification is highly sensitive in patients with symptoms of impingement, but has low specificity, which is why other factors must be contributing to the generation of symptoms. The AIIS impingement is due to AIIS hypertrophy or elongation and may be secondary to:
- -
One traumatic accident, which is usually the most common cause. We may find the AIIS apophysitis due to repetitive traction microtrauma, or the osseous apophysis avulsion, or the insertion of the direct tendon of the rectus femoris muscle. Although most patients who suffer from traumatic AIIS avulsion have a good response to conservative therapy, in some cases the inferior displacement of the apophysis leads to poor junction, and an abnormally elongated or hypertrophied AIIS. If there is damage to the tenon of the rectus femoris muscle, there may be presence of heterotopic calcification as part of the healing process.
- -
One developmental anomaly with an unusually low AIIS associated with the acetabulum retroversion.
- -
An excessive correction following one periacetabular osteotomy in patients with hip dysplasia.6,31,32
The subspinal impingement is due to a morphological alteration in the subspinal space. The bone between the AIIS (that in this case may have normal morphology and location) and the acetabular rim is usually concave with medial insertion of the articular capsule and the iliofemoral ligament, and lateral insertion of the tendon reflex or indirect tendon of the rectus femoris. Due to an excessive traction of these structures with certain hip movements (especially during hyperextension and forced rotation), the hypertrophy of the subespinal bone may occur (that remains straight or convex), with effective reduction of this space, and secondary soft-tissue impingement with the movements of flexion, abduction, and internal rotation of the hip.32
The subspinal impingement and the AIIS share clinical and demographic characteristics.7,32 There is a higher incidence in young patients who practice sports, usually between 15 and 30 years of age—predominantly male patients. It starts with groin pain, or pain in the anterior region of the hip when the patient makes a move of forced or maintained flexion, and it becomes worse with certain sporting activities such as the ball-kicking and speed-running when playing soccer,3 and sometimes it unilaterally affects the dominant leg.7,35
In the physical examination, the impingement test is positive with limitation in the abduction and internal rotation maneuvers when the hip joint is flexed to 90°, and there is hypersensitivity to touch and palpation over the AIIS.4–7,31,32
While establishing the radiologic diagnosis, the simple X-ray (in the anteroposterior projections of the pelvis and Lequesne's false profile of the hip) and the CT scan (particularly in 3D volumetric reconstructions) play important roles since they allow the orthopedic surgeon to perform his preoperative evaluation.
The most significant radiologic findings both on the simple X-ray and the CT scan are:
- -
Osseous hypertrophy with deformity or excessive elongation of the AIIS, with caudal extension at acetabular rim level, or below the acetabular rim (Figs. 6 and 7).
Figure 6.Anterior inferior iliac spine and subspine (AIIS). Thirty-two year-old-male who plays soccer and presents with groin pain and limitation while flexing his hip. The simple X-ray of the pelvis (a), the T1-weighted MRI (b), and the CT scan with 3D reconstruction (c) show one hypertrophied AIIS with type III morphology (straight line). The patient was operated using the endoscopic decompression procedure of the AIIS (asterisk in d), with significant clinical improvement. Notice that the left AIIS is also prominent and reaches the acetabular roof with type II morphology (dotted arrow).
(0.39MB).Figure 7.Anterior inferior iliac spine and subspine (AIIS). Sixteen year-old-woman who plays soccer and presents with right groin pain, functional limitation, and positive impingement test. Topogam images (a) sagittal CT-scan (b) and 3D reconstruction (c) showing type III hypertrophy of the AIIS in her right hip over the acetabular roof. The postoperative simple X-ray (d) confirms the partial resection of the elongated AIIS. One simple X-ray conducted five years before this (e) confirmed the normal development of the AIIS.
(0.55MB). - -
Heterotopic ossifications in the path of the rectus femoris muscle.
- -
Occasionally, we will see cysts in the femoral neck in a more distal location than the ones reported in the femoroacetabular impingement.4,6,32,33
- -
Osseous hypertrophy in the subspinal space21,32 (Fig. 8).
Figure 8.Subspinal impingement. Thirty-two year-old-male with groin pain and limitation in his right hip. The X-rays (a and b), the CT scan images (c), and the arthro-MRI (d and f) show the prominence of the anteroinferior iliac spine and the subspinal space reaching the acetabular rim, together with signs associated with femoroacetabular impingement with cam-type deformity and labral tear (arrow in e).
(0.46MB).
Since both conditions usually coexist with signs of FAI,31,32,35 the role of the MRI and the arthro-MRI is detecting associated intra-articular pathology – something particularly significant in subspinal impingements where fractures of the acetabular rim and focal chondrolabral lesions similar to the ones visible in the pincer-type of FAI have been reported – something that some authors attribute to a component of acetabular overcoverage as a result of the morphological alterations of the subspinal space.21,32
The incidental finding of one abnormally elongated AIIS, or heterotopic ossifications is not uncommon following the path of the rectus femoris tendons in asymptomatic patients.5,36
Taking all this into consideration, and for an optimal therapeutic management, a correct correlation between the radiologic findings and the clinical assessment of every patient needs to be established.21 Treatment is surgical, and the surgical access will depend on the type of impingement and presence of associated intra-articular pathology. If the clinical manifestations are attributed to distal impingement due to an elongated AIIS only, the treatment of choice will be the arthroscopic decompression of the AIIS through extra-articular approach. When it comes to the management of subspinal impingements, and as long as we have data on the intra-articular pathology (usually associated with the FAI syndrome), the arthroscopic decompression with intra-articular approach of the subspinal space will be the treatment of choice which, in the same surgical time, will allow us to repair of both the chondrolabral junction and the associated femoroacetabular osseous abnormalities.5,7,21,30–32,35,37
Iliopsoas impingementThe iliopsoas impingement is a rare condition described back in 200738 based on arthroscopic findings consistent with the presence of lesions in the anterior labrum (in the 3 o’clock position for the right hip, and the 9 o’clock position for the left hip) attributable to excessive pressure exerted by the psoas tendon.
Both in the FAI and the rest of conditions associated with labral damage (trauma, developmental hip dysplasia, hyperlaxitude of the joint capsule, …), most labral ruptures usually occur in the anterosuperior region (in the 1–2 o’clock position for the right hip, and the 10–11 o’clock position for the left hip).4–7,39,40
In two studies of series of patients published by Domb et al.,39 and Cascio et al.41 labral lesions atypically and exclusively located in the anterior labrum have been reported associated with an abnormal pressure of the psoas tendon that can be reproduced through passive movements during the arthroscopic procedure, with clinical improvement in most patients after labrum repair and psoas tenotomy.
Several etiopathogenic theories have been proposed trying to explain the lesion mechanism:
- -
One swollen or tense iliopsoas tendon that would be causing the impingement of the anterior labrum during the movements of hip joint extension.
- -
One iliopsoas tendon attached to the capsulolabral complex that would be damaging the labrum due to repetitive traction with movement.6,39,42
On the clinical level, this condition is rare, and most cases occur in young women with an average age of 25–35 years old. They complain of groin pain, or pain in the anterior region of the hip that gets worse with movements of flexion or prolonged sitting; the impingement test conducted during the physical examination is positive. There are times that the patients complain of pain at the psoas tendon palpation.
The iliopsoas impingement should not be mixed up with the extra-articular internal snapping hip (coxa saltans intera), or the iliopsoas impingement occurring after a total arthroscopy of the hip. The extra-articular internal snapping hip occurs after the iliopsoas muscle tendon displacement over the pectineal eminence or the anterior capsulolabral complex and the femoral head and is described as a painful snapping that can sometimes be heard and is reproducible during the physical examination. The iliopsoas impingement occurring after a total arthroscopy of the hip follows iliopsoas tendinopathy due to friction between the tendon and the prosthesis (due to oversizing or poor alignment of some components).43–45
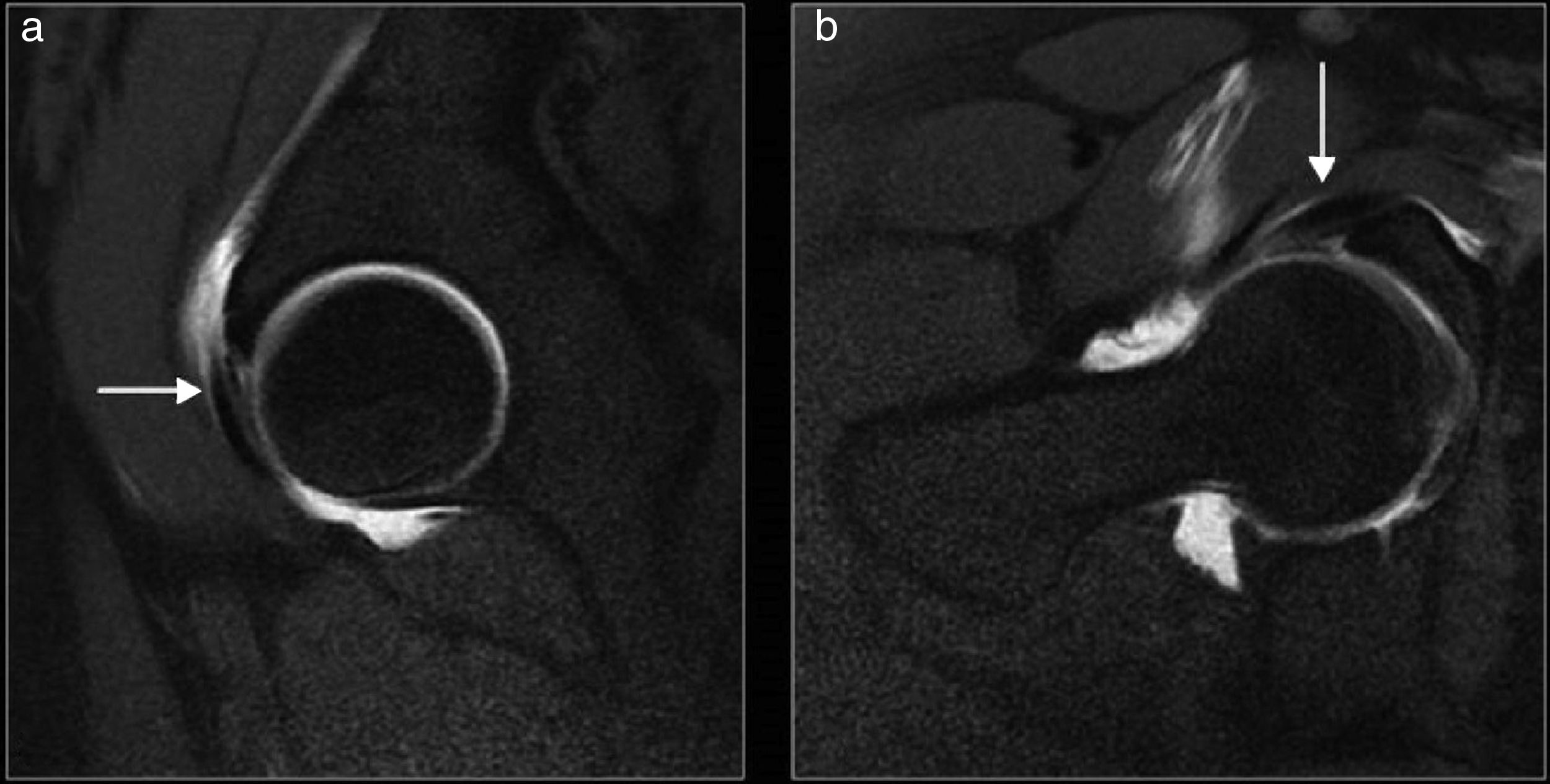
Although we still do not have valid imaging criteria to achieve a conclusive preoperative diagnosis, the MRI or arthro-MRI findings of one isolated lesion in the anterior labrum (in the 3 o’clock position for the right hip, and the 9 o’clock position for the left hip) without extension toward the anterosuperior labrum, and in the absence of radiologic signs suggestive of FAI or acetabular dysplasia, should be indicative of a diagnosis of iliopsoas impingement39,40,45 (Fig. 9).
Iliopsoas impingement. Twenty-four year-old-woman with hip pain and groin pain in her left side. Positive impingement test and pain to touch and palpation in her groin region. The arthro-MRIs with T1-weighted sequences with fat suppression on the sagittal (a) and oblique planes (b) show the tear of the anterior labrum, deep to the iliopsoas tendon, without extension to the anterosuperior labrum (arrow). The simple X-ray (not shown) did not show any signs of femoroacetabular impingement.
The definitive diagnosis of iliopsoas impingement is established during the arthroscopic procedure when in the presence of damage to the labrum of variable severity (from mucoid degeneration to rupture) located underneath the path of the iliopsoas tendon, without evidence of other alterations that may explain it. There are times when we will see local inflammatory changes with capsule deflection and focal synovitis in the anterior articular recess at iliopsoas tendon level.4,39–41,46 It is important to stress out here the possibility of achieving this diagnosis preoperatively, because there is a chance it can go misdiagnosed during the arthroscopic procedure.41
The management of iliopsoas impingement is surgical, with debridement and repair of labral damage, and iliopsoas tendon tonomy at acetabulum level.4,7,39,41,42,46 It is important to rule out here the presence of hip dysplasia prior to the surgery, since in these patients the iliopsoas tenotomy may cause significant anterior hip instability.20,46
Trochanteric-pelvic impingementThe trochanteric-pelvic impingement is a rare condition defined as the abnormal and painful contact between the greater trochanter and the osseous pelvis (acetabular rim, iliac crest, …) with abduction and extension movements.3,21
The physiopathogenic mechanism consists of one complex morphological alteration of the femoral proximal epiphysis due to an early ischemic lesion during the development of the femoral head and neck (intracapsular vascularization) with respect to the trochanteric massif (extracapsular vascularization).7
It is usually described in association with Legg-Calvé-Perthes disease, but as predisposing factors we have all those causing similar deformities of the femoral proximal epiphysis such as infections; proximal femoral epiphysiolysis; trauma-related femoral osteonecrosis; skeletal dysplasia; surgical treatment to correct the hip congenital dysplasia; or varus intertrochanteric osteotomies.3,5,21
Regardless of the etiological factor, the morphological alteration of the femoral proximal epiphysis consists of the presence of coxa breva, coxa magna, coxa plana (with or without acetabulum-related dysplasia), and coxa vara of variable degree, with relative growth of the trochanteric massif that shows an abnormally high position with respect to the femoral head. Consequently, the distance between the greater trochanter and the pelvis is reduced causing a decreased efficiency of the abductor muscles, and a problem of space with certain movements of the hip.3,7
However, the trochanteric-pelvic impingement has also been described in patients with normal femoral morphology, but hypermobility or hyperlaxitude of the hip (such as dancers, patients with connective tissue diseases, …).47
On the clinical level, it is more prevalent in young patients but there is no predominant sex, and it frequently coexists with intra-articular pathology.5,21 Patients complain of pain in the lateral or posterolateral regions of the hip, especially with movements of extension and abduction, with early fatigue when walking or even in bipedalism. The physical examination confirms presence of pain and limitations in the hip movements of abduction and extension; also, the “gear stick” sign may be positive (limitation to the hip passive abduction while in extension, not flexion). Sometimes there is shortening of the damaged limb, and presence of Trendelemburg gait pattern (due to fragility of the abductor muscles).3,7,21
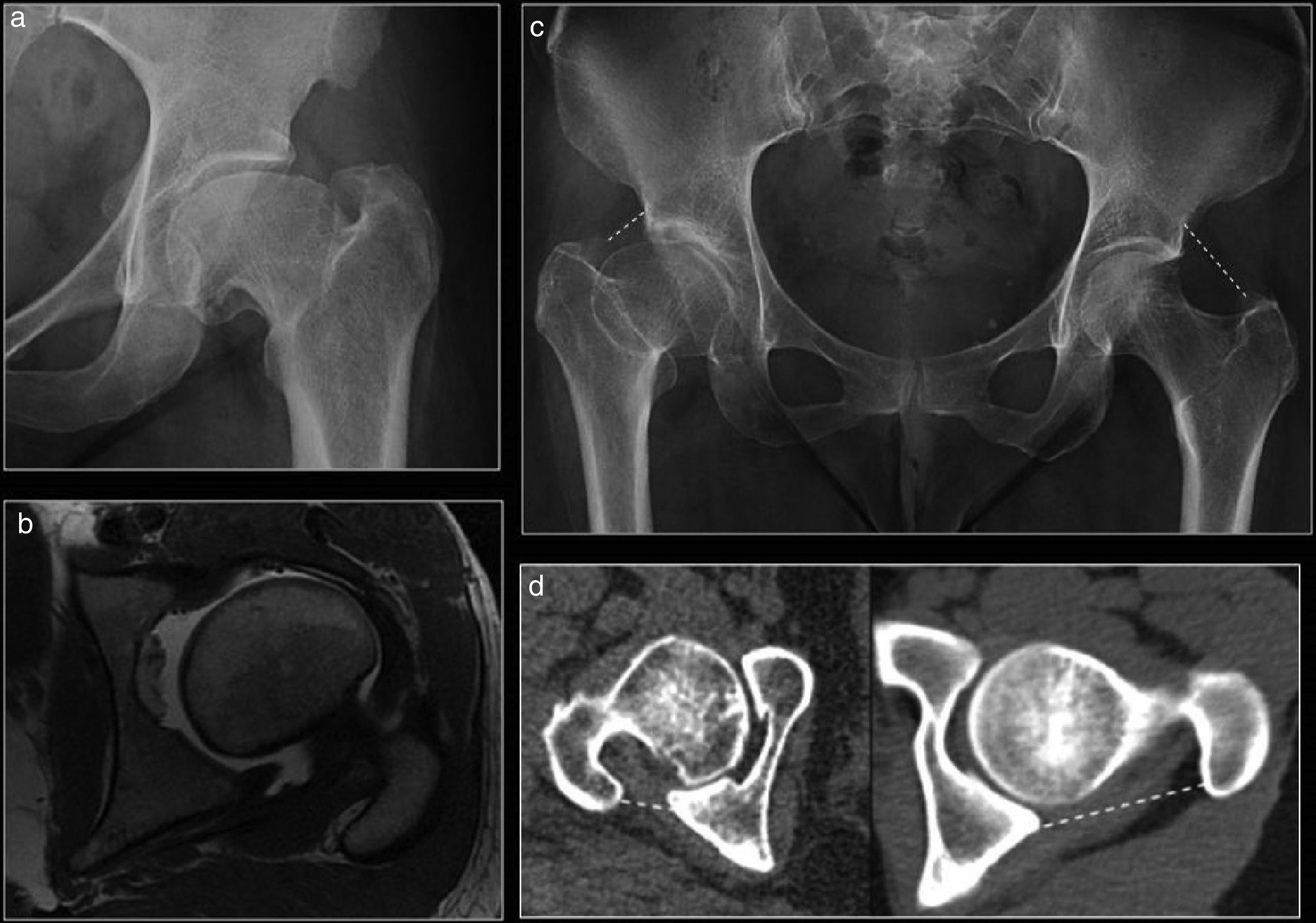
The diagnosis of the trochanteric-pelvic impingement is based on the correlation between the clinical manifestation and findings made at the simple X-ray (anteroposterior projection of the pelvis or hip) and the morphological alterations seen in the proximal femoral epiphysis, especially the reduced cervical diaphysiary angle of the femur (coxa vara), and the abnormal position of the trochanteric massif overtaking the level of the femoral neck or head. The more cranial the tip of the greater trochanter is to the center of the femoral head, the greater the radiologic suspicion of trochanteric-pelvic impingement should be3,5,7,21,48 (Fig. 10).
Trochanteric-pelvic impingement. Different patients with typical alterations of their femoral proximal epiphysis (a and b), with an oversized femoral head and flattened morphology (coxa magna and plana), shortening of the femoral head (coxa breva), and a reduced cervical diaphysiary angle (coxa vara) causing an elevated trochanteric massif with respect to the femoral head, with the corresponding shortening of the space between the greater trochanteric and the osseous pelvis (dotted lines in c and d). Compare with the normal left hip.
The management of the trochanteric-pelvic impingement is initially based on conservative measures with restriction of the physical activity, rehabilitation, and local infiltrations. When conservative measures fail, surgical treatment is indicated and, in general, it consists of the distal transfer of the greater trochanter followed, or not, by corrective osteotomies. The studies confirm the postoperative clinical improvement and functional limitations.5,7
ConclusionsHip or groin pain is a common cause for medical consultation, and imaging modalities play an additional role in their etiological diagnosis.
Although less common than the FAI syndrome, other forms of extra-articular hip impingement have also been described including ischiofemoral impingement; subspinal impingement; AIIS impingement; iliopsoas impingement; and trochanteric-pelvic impingement, as the cause of hip pain, particularly in young active patients.
Getting to know the clinical manifestations and findings from the imaging modalities of these forms of extra-articular impingement allows radiologists to suggest even more specific diagnoses to eventually help the traumatologist decide what the optimal treatment should be.
Ethical responsibilitiesProtection of human and animal subjectsThe authors declare that no experiments with human beings or animals have been performed while conducting this investigation.
Confidentiality of dataThe authors confirm that in this article there are no data from patients.
Right to privacy and informed consentThe authors confirm that in this article there are no data from patients.
FundingThe authors confirm no source of funding whatsoever.
Authors contributions- 1.
Manager of the integrity of the study: NAG.
- 2.
Study Idea: NAG and NSG.
- 3.
Study Design: NAG and NSG.
- 4.
Data Mining: NAG, NSG, JGM and MGB.
- 5.
Data Analysis and Interpretation: NAG and NSG.
- 6.
Statistical Analysis: N/A.
- 7.
Reference: NAG, NSG and JGM.
- 8.
Writing: NAG, NSG y MGB.
- 9.
Critical review of the manuscript with intellectually relevant remarks: NAG, NSG, JGM and MGB.
- 10.
Approval of final version: NAG, NSG, JGM and MGB.
The authors declare no conflict of interests associated with this article whatsoever.
We wish to thank Dr. Óliver Marín-Peña, MD from the Unit of Traumatology of the Hospital Universitario Infanta Leonor for his opinions while preparing this manuscript, and his pioneer dedication to the study and research of these conditions.
Please cite this article as: Arévalo Galeano N, Santamaría Guinea N, Gredilla Molinero J, Grande Bárez M. Atrapamientos y choques extraarticulares de la cadera: revisión de la literatura. Radiología. 2018;60:105–118.