Melioidosis is an endemic disease in Southeast Asia and Oceania caused by the gram-negative bacillus Burkholderia pseudomallei. We studied 15 adult patients from Colombia with microbiologically diagnosed pulmonary melioidosis. We reviewed 15 chest X-rays and 10 chest computed tomography (CT) studies. Of the 15 patients, 87% met the criteria for acute infection and 13% met the criteria for chronic infection. The most common findings on chest X-rays were consolidation (86%), nodules (26%), and cavitation (20%). On CT studies, consolidation and nodules were observed in 90% of cases; the areas of consolidation were predominantly located in the basal and central zones in 60%. Areas of cavitation were observed in 50%, pleural effusion in 60%, and mediastinal lymph nodes in 30%. In patients with acute pulmonary melioidosis (n=8), the findings observed were nodules (100%), mixed pattern with nodules and consolidation (87%), pleural effusion (88%), and mediastinal lymph nodes (25%). The two patients with chronic pulmonary melioidosis both had cavitation. Acute lung infection with B. Pseudomallei has radiologic manifestations similar to those of pneumonia due to other causes. In areas where the disease is endemic, it is essential to include acute melioidosis in the differential diagnosis of pulmonary nodules and chronic melioidosis in the differential diagnosis of cavitated chronic lung lesions.
La melioidosis es una enfermedad endémica en el suroeste asiático y Oceanía y está causada por la infección por el bacilo gramnegativo Burkholderia pseudomallei. Se estudian 15 pacientes adultos de Colombia con diagnóstico microbiológico de melioidosis pulmonar. Se revisaron 15 radiografías de tórax y 10 tomografías computarizadas (TC) de tórax. De los 15 pacientes, el 87% tenía criterios de infección aguda y el 13%, de infección crónica. Los hallazgos más frecuentes en la radiografía de tórax fueron: consolidación (86%), nódulos (26%) y cavitación (20%). En la tomografía computarizada se encontraron áreas de consolidación y nódulos en el 90% de los casos. En el 60% de los pacientes, las áreas de consolidación fueron de predominio basal y central. En el 50% de los casos se evidenciaron áreas de cavitación. Se evidenció derrame pleural en el 60% y adenopatías mediastínicas en el 30% de los casos. En los pacientes con presentación aguda (n=8), los hallazgos visualizados incluyeron: nódulos (100%), patrón mixto con nódulos y consolidación (87%), derrame pleural (88%) y adenopatías mediastínicas (25%). Los pacientes con melioidosis crónica (n=2) presentaron cavitación. La infección pulmonar aguda por B. Pseudomallei cursa con manifestaciones radiológicas similares a neumonías de otra etiología. En zonas endémicas debe considerarse la posibilidad de melioidosis aguda en el diagnóstico diferencial de nódulos pulmonares, y de melioidosis crónica en el diagnóstico diferencial de lesiones pulmonares crónicas cavitadas.
The term melioidosis describes infection caused by the Gram-negative bacillus Burkholderia pseudomallei, a saprophytic soil bacterium. Melioidosis is endemic in Southeast Asia and Australia, but cases have been reported in the Americas.1,2
This disease mainly affects people who are in contact with soil or water contaminated with B. pseudomallei. The main mechanism of infection is direct inoculation of the bacteria through breaks in the skin. Other forms of contagion are inhalation and ingestion of the microorganism. Melioidosis can manifest itself in different clinical forms, but the lungs are the most common organs to be affected in these patients.3 To simplify the analysis, in this review we classify the forms of presentation into acute (less than two months) and chronic (more than two months).
We present the radiological findings of a series of patients with pulmonary melioidosis diagnosed on the north coast of Colombia.
Materials and methodsWe retrospectively reviewed the medical records and imaging studies of 15 adult patients diagnosed with pulmonary melioidosis confirmed by isolation of the B. pseudomallei bacillus from respiratory or blood samples. The isolates were sent to a reference laboratory where their growth on Ashdown agar was verified, and microbiological identification was performed using MicroScan WalkAwayTM (Beckman Coulter, USA) and VITEK 2 Compact (BioMerieux, France). The analysis of the diagnostic images was performed retrospectively, and by consensus, by two radiologists with 25 (JACB) and three (AMA) years of experience in chest radiology.
The following variables were analysed in the chest X-rays and computed tomography (CT) scans as defined by the Fleischner Society criteria4: consolidation; ground glass opacity; cavitation; nodules; centrilobular micronodules; pleural effusion; and mediastinal lymphadenopathy. When more than one abnormality was found in the lung parenchyma, the predominant abnormality was described (subjective visual analysis).
The distribution of parenchymal changes was defined as focal or multifocal; apical (lesions above the hilum); basal (lesions caudal to the hilum); central (lesions medial to an imaginary vertical line that passes through the middle of the clavicle); peripheral (lesions lateral to an imaginary vertical line that passes through the middle of the clavicle); or diffuse (abnormalities in all four quadrants on the radiographic image).
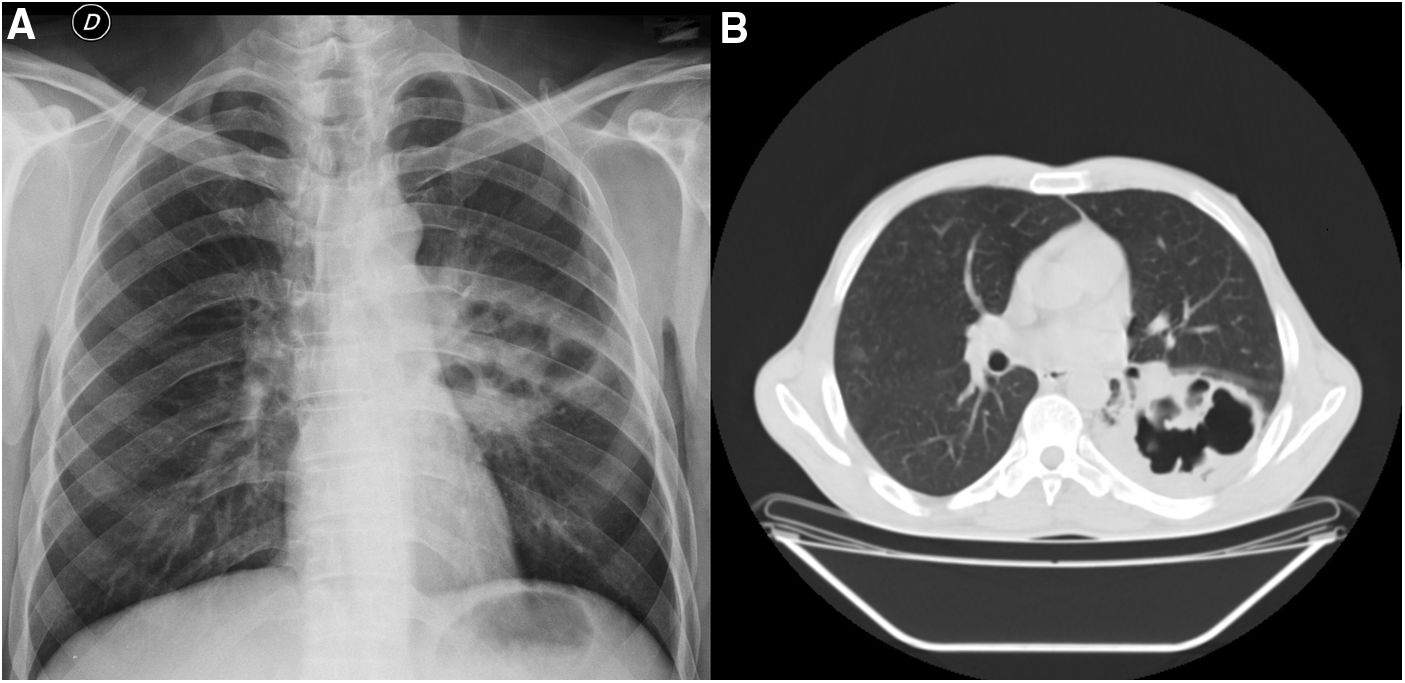
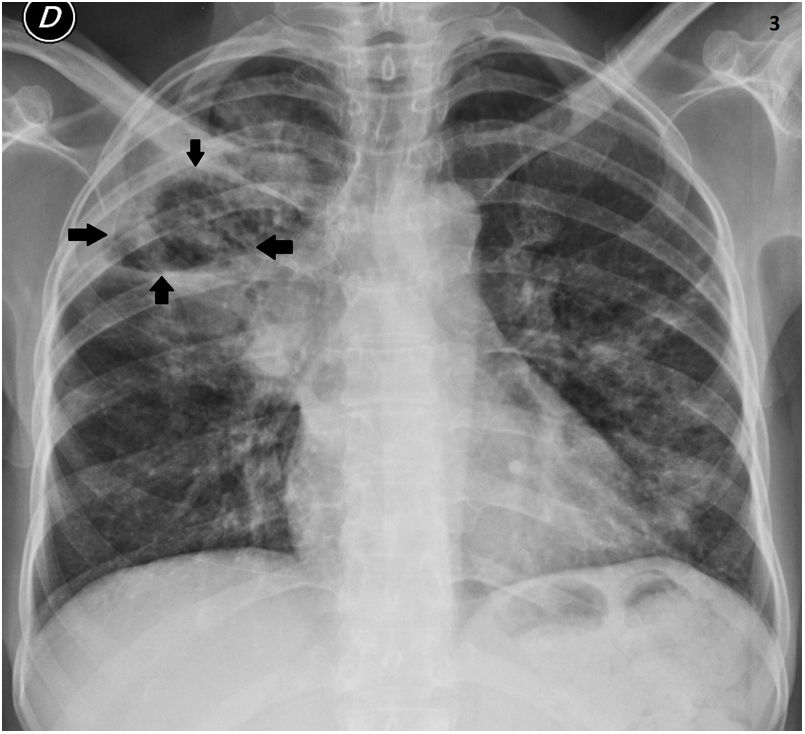
ResultsIn total, we considered 15 patients with a confirmed microbiological diagnosis of melioidosis. Of the 15 patients, 13 (87%) met the criteria for acute infection and two (13%) for chronic infection. All the patients’ chest X-rays (n=15) and chest CT for 10 of the cases were reviewed. Consolidation was the most common finding in the series of chest X-rays (87%); 11 patients with acute infection and two with chronic infection (Figs. 1–3). The distribution of the consolidation was multifocal and predominantly central in 60% and 67% of cases respectively. In four patients (26%) nodules were found on the X-ray (three patients also had consolidation). Three patients (20%) had cavitation (two with chronic infection) (Table 1).
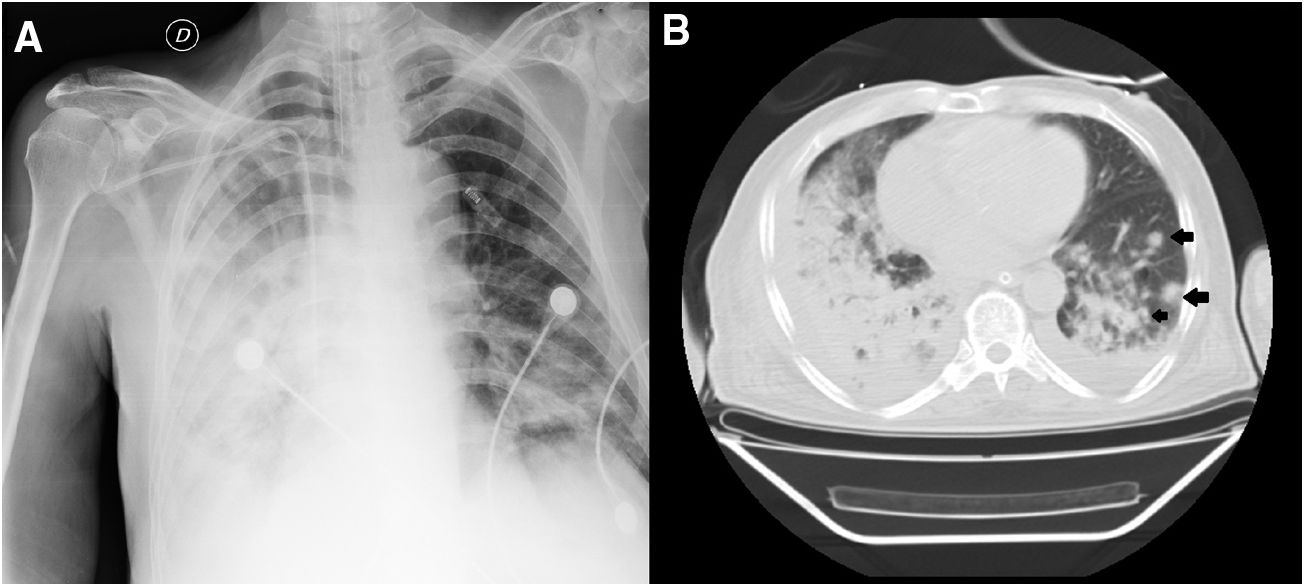
(A and B) Acute melioidosis. 72-year-old male on mechanical ventilation. (A) Chest X-ray. Diffuse alveolar opacities in the right lung and focal in the left lower lobe. Right pleural effusion. (B) Chest computed tomography. Consolidation in the right lower lobe and middle lobe, and solid nodules in the left lower lobe with irregular contours, with diameters from 4 to 11mm (arrows). Bilateral pleural effusion.
Demographic and clinical characteristics and radiological findings of patients with pulmonary melioidosis from the north coast of Colombia.
| Characteristics | No. (%) |
|---|---|
| Gender | |
| Male | 11 (73.3) |
| Female | 4 (26.6) |
| Age in years, median (range) | 58 (3–89) |
| Comorbidities | |
| Diabetes mellitus | 10 (66.6) |
| Hypertension | 6 (40) |
| Long-term steroid use | 2 (13.3) |
| Chronic kidney disease | 1 (6.6) |
| Type of pulmonary melioidosis | |
| Acute | 13 (86.6) |
| Chronic | 2 (13.3) |
| Chest X-ray findings (n=15) | |
| Consolidation | 13 (86.6) |
| Focal distribution | 4 (26.6) |
| Multifocal distribution | 9 (60) |
| Apical predominance | 4 (26.6) |
| Basal predominance | 7 (46.6) |
| Diffuse distribution | 2 (13.3) |
| Central distribution | 10 (66.6) |
| Peripheral distribution | 3 (20) |
| Nodules | 4 (26.6) |
| Cavitation | 3 (20) |
| Pleural effusion | 6 (40) |
| Chest CT findings (n=10) | |
| Consolidation | 9 (90) |
| Nodules | 9 (90) |
| Cavitation | 5 (50) |
| Pleural effusion | 9 (50) |
| Centrilobular micronodules | 2 (20) |
| Lymphadenopathy | 3 (30) |
| Ground glass | 3 (30) |
| Predominant pattern | |
| Consolidation | 5 (50) |
| Nodules | 5 (50) |
| Distribution of areas of consolidation | |
| Apical | 2 (20) |
| Basal | 6 (60) |
| Diffuse | 1 (10) |
| Central | 6 (60) |
| Peripheral | 2 (20) |
| CT findings of patients with acute melioidosis (n=8) | |
| Consolidation | 7 (87.5) |
| Nodules | 8 (100) |
| Cavitation | 3 (37.5) |
| Pleural effusion | 7 (87.5) |
| Centrilobular micronodules | 1 (12.5) |
| Lymphadenopathy | 2 (35) |
| Predominant pattern | |
| Consolidation | 3 (37.5) |
| Nodules | 5 (62.5) |
Ten chest CT scans were reviewed, eight of which were from patients with acute infection and two, chronic infection. The most common CT findings in the two groups were consolidation in nine cases (90%) and nodules in nine (90%). In eight patients (80%) a combination of nodules and consolidation was documented. In 60% of cases, the areas of consolidation were predominantly basal and central. Areas of cavitation were seen in 50% of the cases. Sixty percent of the patients had pleural effusion, 30% had mediastinal lymphadenopathy and 30% ground glass opacities.
In patients with acute presentation, the most common finding was pulmonary nodules (100%), followed by areas of consolidation (88%). Seven patients (87%) had a mixed pattern with nodules and consolidation. Pleural effusion was found in 88% and 25% had mediastinal lymphadenopathy. Of the two patients with a chronic clinical presentation, one had cavitary areas of consolidation and the other had areas of consolidation associated with cavitary nodules.
DiscussionMelioidosis is an endemic disease in Southeast Asia, India, China and northern Australia.1 Cases are found sporadically in other tropical areas such as Colombia.2 In Europe this disease has been reported in travellers who have visited endemic areas. For that reason, although it is unusual, when we find pneumonia in a patient with a history of travel to these regions, especially in the rainy season, with or without risk factors, it should be included in the differential diagnosis algorithm. This is the first case series to describe the radiological findings in patients with pulmonary melioidosis in the Americas.
The radiological manifestations of pulmonary melioidosis are nonspecific and may vary according to the chronology of the disease (acute vs chronic) and the pathophysiological mechanism of the infection (primary vs secondary). As previously published in the literature, the most common radiological manifestation in acute pulmonary melioidosis is lung nodules, a finding related to the pathophysiology of the presentation (haematogenous spread). Similarly, cavitary lesions predominate in the chronic form of presentation.5–7
In contrast to reports in the literature, in our case series the parenchymal abnormalities predominated in the lung bases. Pleural effusion and mediastinal lymphadenopathy were more common than described in the specialised literature.8–10 There were no cases of pneumothorax, hydropneumothorax, pleural empyema or pericardial abnormalities in this group of patients.
The imaging differential diagnosis varies according to the form of presentation of the disease. In patients with acute melioidosis, the radiological manifestations are indistinguishable from pneumonia caused by other germs. However, melioidosis should be suspected in patients with multiple pulmonary nodules in endemic areas. Chronic melioidosis should be considered in the imaging differential diagnosis of chronic cavitary lung diseases, including infectious disorders such as tuberculosis, chronic cavitary aspergillosis, histoplasmosis, coccidioidomycosis, blastomycosis and paracoccidioidomycosis, and non-infectious disorders such as primary bronchogenic carcinoma and metastatic disease.11 Moreover, with the current situation of the SARS-CoV-2 pandemic, in view of the wide spectrum of manifestations associated with this virus, COVID-19 must be taken into account as a differential diagnosis; not forgetting potential co-infections in regions where melioidosis is endemic.
ConclusionsAcute melioidosis infection has nonspecific radiological manifestations, which are common to other bacterial or mycobacterial infections. In areas endemic for B. pseudomallei infection, the possibility of acute melioidosis should be considered in the differential diagnosis of pulmonary nodules and chronic melioidosis in the differential diagnosis of chronic cavitary lung disease.
Authorship- 1
Responsible for the integrity of the study: JYR
- 2
Study concept: JYR and CAA
- 3
Study design: JYR and CAA
- 4
Data collection: JYR
- 5
Data analysis and interpretation: JAC and AMA
- 6
Statistical processing: JAC and AMA
- 7
Literature search: JAC, AMA and JYR
- 8
Drafting of the article: JAC, AMA and JYR
- 9
Critical review of the manuscript with intellectually relevant contributions: JAC, AMA, JYR and CAA
- 10
Approval of the final version: JAC, AMA, JYR and CAA
The authors declare that they have no conflicts of interest.