We present the case of a 60-year-old man referred to our institution with a diagnosis of muscle-invasive high-grade urothelial bladder cancer (BC), resected transurethral (TURB), with suspected extension to the abdominal wall. The referring physician requested a review of prior computed tomography (CT) and ordered in-house magnetic resonance imaging of the bladder with and without gadolinium (MRI) and [18]FDG-PET/CT for local and distant staging.
Review from foreign CT obtained before TURB [Fig. 1] showed the biopsy-proven BC of the anterior-superior bladder wall, which was inseparable from an irregularly shaped mass at the right internal inguinal ring. After TURB [Fig. 2], MRI did not delineate residual bladder mass, and the inguinal ring lesion was hypointense on T1- and T2-weighted images without post-contrast enhancement. On 18FDG-PET/CT, such lesion had low-level radiotracer avidity, and there was no evidence of distant disease. The diagnosis was that such lesion represented a hernia plug mimicking extravesical cancer spread into the abdominal wall. After interdisciplinary discussion, the decision was to administer neoadjuvant chemotherapy, followed by cystectomy with neobladder formation. The pathology showed the absence of residual carcinoma and the lymph nodes samples showed benign features.
Axial contrast-enhanced CT, portal-venous phase, before TURB. It shows an irregular and enhancing solid mass of the anterior-superior bladder wall (short arrow), the biopsy-proven BC, measuring 6.6×3.3cm. Such mass is inseparable from an irregularly shaped mass with soft-tissue density at the right internal inguinal ring (long arrow), measuring 3.5×2.5cm. The latter represents a plug-mesh inguinal hernia repair mimicking extravesical tumor extension into the anterior abdominal wall.
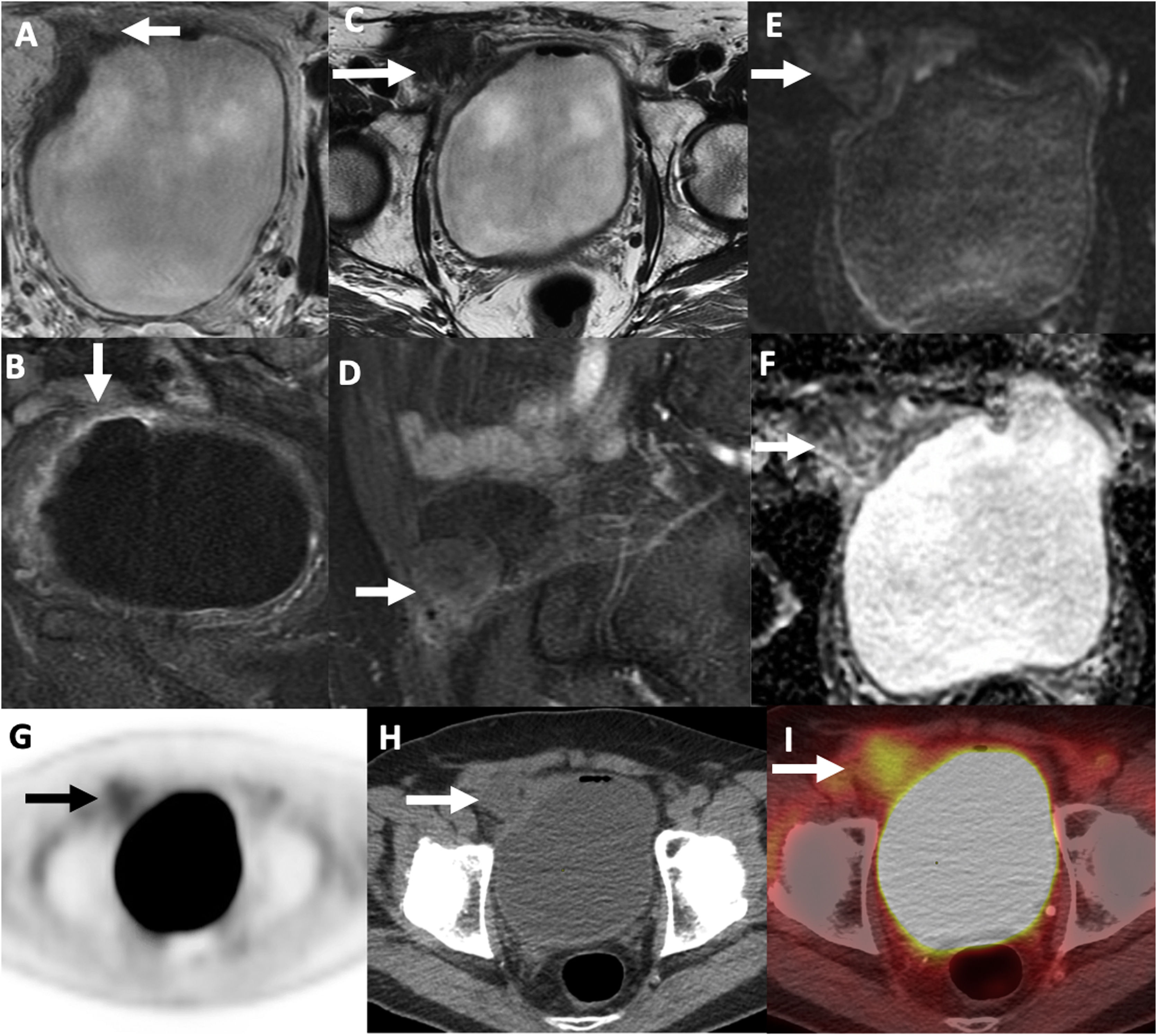
(A–F) Contrast-enhanced MRI of the bladder after transurethral resection (TURB). (A) Axial T2-weighted, (B) axial T1-FS contrast enhanced, (C) axial T2-weighted, (D) sagittal T1-FS without contrast, (E) DWI, b value: 1000, (F) ADC map. No residual bladder malignancy (short arrows) was identified on T2-weighted (A) or contrast-enhanced (B) sequences. The right inguinal hernia mesh-plug initially delineated on CT (arrows on C–F) was an irregular solid lesion hypointense on T2-weighted images (C), without contrast-enhancement (D) or restricted diffusion (E: B1000, F: ADC map), representing granulation tissue from the prior hernia repair. G–I: 18FDG PET/CT after TURB. (A) PET, (B) PET/CT fused, (C) CT. The right inguinal hernia plug (arrows) had low-level tracer uptake (SUV: 2.6g/ml) on PET (G) and fused PET/CT (I) and was isodense to muscle on non-contrast CT (H), supporting the diagnosis of granulation tissue.
In the patient presented, there is an anterior-superior bladder wall tumor and a mass-like lesion due to granulation tissue in the inguinal ring. The review of the patient's history, visualization of the overlying postsurgical changes at the inguinal ring, along with the delineation of the features described on CT, MRI, and PET/CT, led to the appropriate diagnosis and aided in the clinical management.
While the biopsy is necessary to discriminate muscle-invasive from non-muscle-invasive BC, imaging is useful to assess for extravesical tumor spread, adjacent organ invasion, nodal and distant metastatic disease, and synchronous upper tract urothelial cancers.1
BC extension into the abdominal or pelvic walls (i.e., tumor stage T4b) is relatively rare. In a cohort of 917 patients undergoing cystectomy, for example, it was present in 4.3% of cases and associated with a poor prognosis.2 The current standard-of-care treatment options for stage T4b BC include systemic chemotherapy or concurrent chemoradiotherapy.3 Only selected individuals might be candidates for cystectomy.3
MRI is the most appropriate modality to assess BC's local extent. The disruption of perivesicular fat planes characterizes extravesical tumor spread; this and tumor extension into adjacent structures are best evaluated on multiplanar T2-weighted images; contrast-enhanced and diffusion-weighted imaging can help equivocal cases.1 While CT and 18FDG-PET/CT may help assess the local tumor extent, they are mainly used to screen for nodal and distant metastatic disease.4
Mesh-plug repair of an indirect inguinal hernia involves the placement of a conical plug through the hernia defect and reinforcement with an overlying mesh. This can induce a foreign body reaction, including inflammation and granulation tissue formation. On imaging, the plug is located at the internal inguinal ring in proximity to the epigastric vessels and may have a round, oval, or irregular shape. It can be iso- or hypodense to soft tissue on CT. On MRI, it is typically hypointense on T1-weighted images. The signal intensity on T2-weighted and contrast-enhanced sequences is variable and driven by the relative amounts of inflammation, granulation tissue, and scarring. Contrast-enhancement, if present, is usually rim-like in the periphery of the plug. The radiotracer avidity of hernia plugs on 18FDG PET/CT is variable, and there is no specific pattern of FDG uptake.5
In conclusion, BC extension into the abdominal/pelvic wall is infrequent and has significant prognostic and therapeutic implications. Plugs from a prior hernia repair can mimic the extravesical spread of BC. Clues to the correct diagnosis include a plug's location at the internal inguinal ring, the presence of postsurgical changes, and correlation with the patient's surgical history. As illustrated with the patient presented, imaging provides valuable information aiding in the patient management.
Conflict of interestAuthors were supported in part through NIH / NCI Cancer Center Support Grant P30 CA008748.
Dr. Andreas Wibmer and Dr. Guido Dalbagni for their generously support and help.
Please cite this article as: Causa Andrieu PI, Tzeng M. Tapones de hernia inguinal que imitan la invasión de la pared abdominal de un cáncer de vejiga: un posible obstáculo para la interpretación de imágenes. Radiología. 2022;64:274–276.