Radiologists must be able to recognize the imaging signs of intestinal malrotation because this condition can lead to potentially lethal complications such as midgut volvulus. The correct diagnosis depends on both high clinical suspicion and the radiologist's ability to recognize the specific signs of malrotation and the normal variants that can lead to the wrong diagnosis. Although the location of the third portion of the duodenum outside the retroperitoneal area on ultrasonography, CT, or MRI seems to be a reliable sign of malrotation, the gold standard for determining whether the duodenojejunal flexure is in an abnormal location continues to be the upper gastrointestinal series. In this article, we review the most important imaging signs of malrotation and emphasize the role of ultrasonography in diagnosing midgut volvulus.
El radiólogo debe ser capaz de reconocer los signos de la malrotación intestinal en la imagen al tratarse de una entidad patológica con complicaciones potencialmente letales, como el vólvulo de intestino medio. Para diagnosticarla correctamente, es tan importante que exista un índice de sospecha clínica elevado como que el radiólogo sepa reconocer los signos específicos de malrotación y las variantes de la normalidad que pueden conducir a un diagnóstico erróneo. Aunque la posición no retroperitoneal de la tercera porción duodenal en ecografía, TC o RM parece ser un signo fiable para el diagnóstico, el tránsito gastrointestinal continúa siendo el estándar de referencia para ver la unión duodeno-yeyunal en una posición anómala. Nuestro objetivo es revisar los principales signos radiológicos de esta enfermedad y hacer hincapié en el papel de la ecografía para diagnosticar el vólvulo de intestino medio.
Intestinal malrotation involves a spectrum of abnormalities in the middle intestine (MI) due to an abnormal loop rotation and mesenteric fixation.1,2 It is a predisposing factor for both the volvulus and intestinal obstruction during the neonatal and childhood periods–entities requiring urgent surgery due to the risk of massive intestinal necrosis.3–5 Occasionally there are clinical signs of alert though they are not specific.6 It is essential to diagnose this condition precisely to avoid catastrophic consequences and unnecessary interventions.3 Our goal is to focus both on the main radiologic findings and the use of ultrasound for the diagnosis of volvulus and middle intestine.
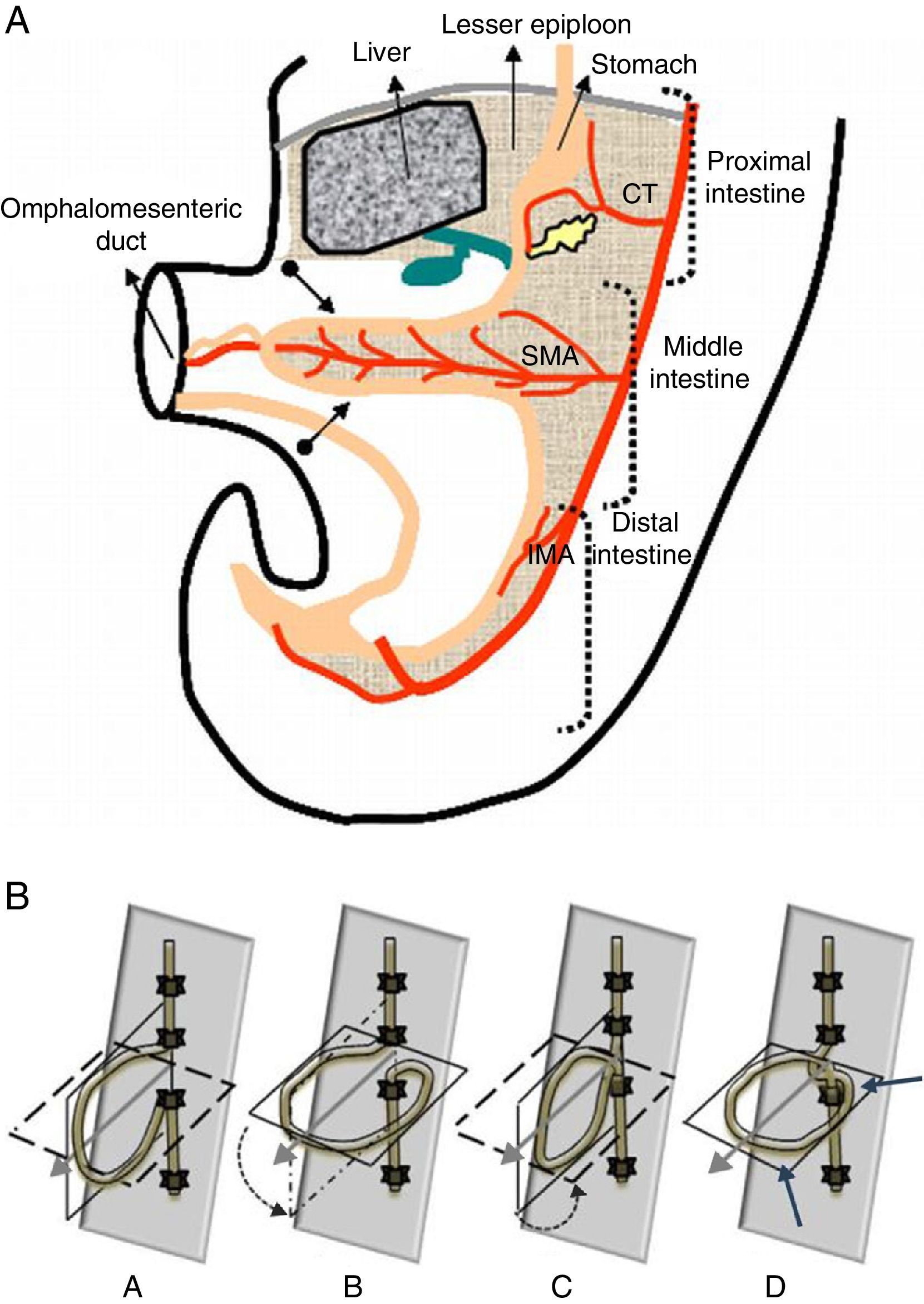
Embryology and categorizationThe intestine evolves from the vitelline sac.7 In an early embryo phase the primitive gastrointestinal tract looks like a straight tube that is divided into three (3) different segments: proximal intestine irrigated by the celiac trunk; middle intestine running from the biliary duct insertion toward the distal-medial end of transverse colon and irrigated by the superior mesenteric artery (SMA); and distal intestine irrigated by the inferior mesenteric artery (IMA).2,6,7 In turn the MI is divided into one cranial, periarterial or duodenum–jejunal junction (origin of distal duodenum, jejunum and proximal ileum) and one caudal, postarterial or cecocolic segment (origin of distal ileum, cecum, appendix, ascending colon and transverse colon), based on its position relative to omphalomesenteric vessels (future SMA)2,6,8,9 (Fig. 1A). During the development of the embryo the MI undergoes a process of growth and enlargement including herniation, rotation, reduction and fixation.1 This process–key for intestinal loops to assume a normal positioning starts–during gestation week#5 and ends shortly after birth.6
(A) Scheme of intestine in a 5-week old embryo. Initially the digestive tube looks like a straight tube and is divided into three (3) different sections: the proximal intestine–irrigated by the celiac trunk (CT), the middle intestine–irrigated by the superior mesenteric artery (SMA), and the distal intestine–irrigated by the inferior mesenteric artery (IMA). Then it elongates and the middle intestine is divided into the duodenumjejunal loop above the SMA and the cecocolic loop below the SMA–both highlighted in the scheme with an arrow. (B) Model of the cord of intestinal rotation. A. The upper section above the SMA corresponds with the duodenumjejunal loop and the lower section with the cecocolic loop. B. The cord has rotated 90° anti-clockwise. C. Location of the cord after rotating another 90° anti-clockwise. D. Location after the last 90° rotation–three-fourths of one complete turn. Arrows indicate the final location of cecocolic loop.
The rotation process begins with an MI elongation disproportionate with respect to the embryo so by the sixth week of gestation the intestine ends up herniated in the umbilical cord to be able to keep growing.2,6,10 The loop-or-“U”-shaped herniated intestine undergoes one 90° anti-clockwise rotation around the SMA with the duodenum–jejunal junction looking right and down and the cecocolic section left and then up.6,7 While the MR stays herniated its length keeps on growing at the expense of–above all–the duodenum–jejunal junction that rotates another 90°-anti clockwise once more. The disproportionate elongation of the cranial section influences the position of the cecocolic loop yet it will not undergo any more rotations during this stage.6 Around gestation week#10 the embryonic intestine enters again the abdominal cavity but first it is the proximal loop that enters it by making its third 90° anti-clockwise rotation until the duodenum acquires its typical “C” shape with its distal section looking posterior–inferior to the SMA and the Treitz angle being located left to the spinal cord2,6,9,10 (Fig. 1B). Then the caudal MI comes back to the abdomen by rotating again inside the abdominal cavity some 180° clockwise until the colon acquires its normal framework disposition ahead of the SMA being the cecum located to the right6,7,11; cecum elongates itself again descending toward inferior quadrants during the remaining gestational period.6
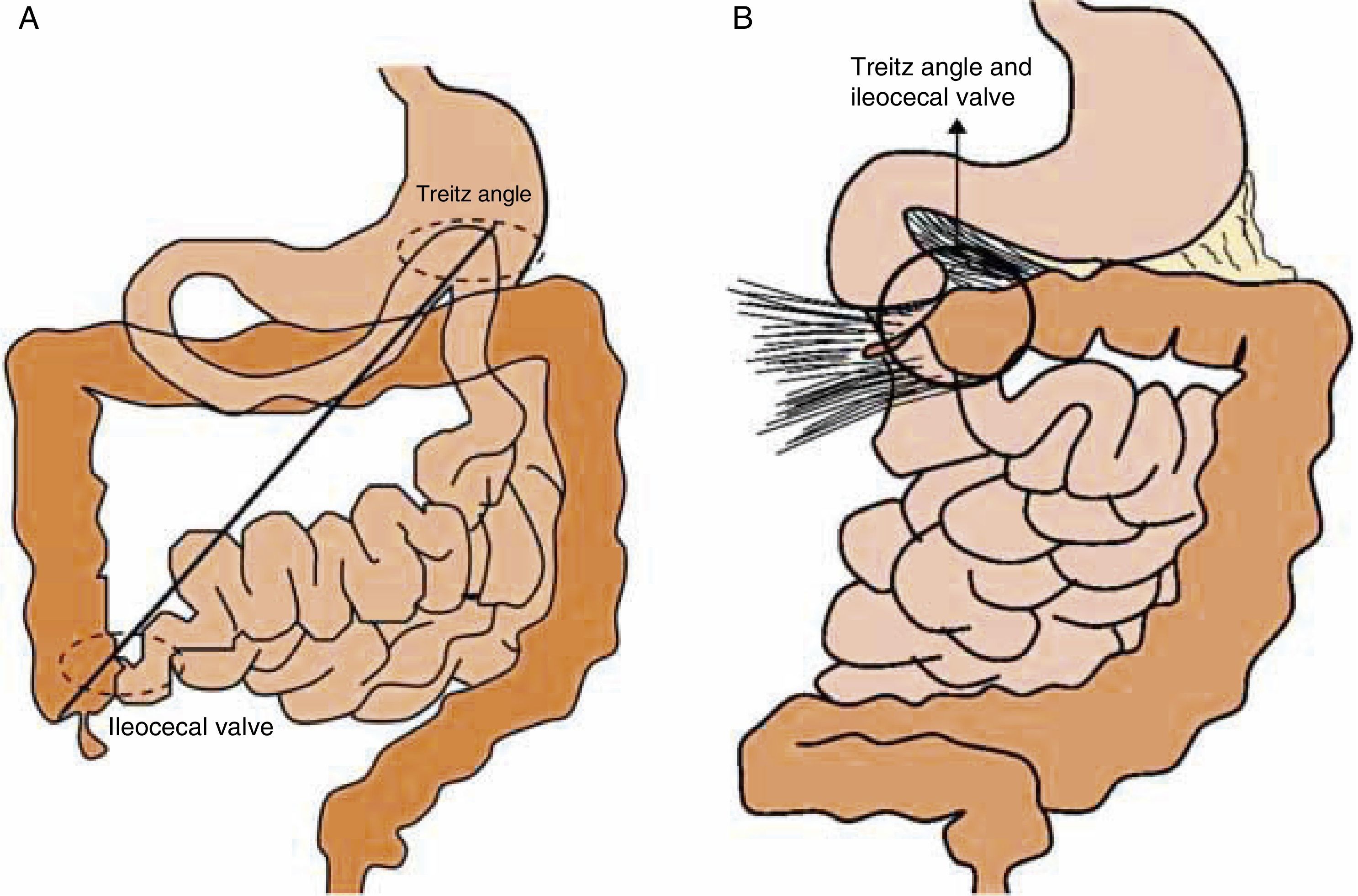
Finishing the process of intestinal rotation at week#12 the loops connect themselves to the posterior parietal peritoneum through several anchor points.7 Intestinal rotation needs to be complete until the attachment of loops to the walls of the abdominal cavity is correct.7,10 The mesentery of the second, third and fourth duodenal section connects itself to the retroperitoneum and one extension of the right diaphragm crura of the fibrous tissue surrounding the celiac trunk anchors the duodenum–jejunal junction to the superior left quadrant making up the Treitz ligament.6,9 The mesentery of the cecum and the ascending and descending colon merges with the posterior wall of peritoneum, the mesentery of sigma partially merges with the retroperitoneum, and the mesentery of transverse colon merges with the large epiploon.6 On the left of a fixation line along the SMA and its branches the mesos that stays ahead remains free making up the mesentery of the small intestine that connects obliquely from the Treitz angle to the posterior wall and all the way toward the ileocecal valve. Both anchor points are far away from one another which enables a wide implantation base that stabilizes the loops of the small intestine while preventing volvulation6,12 (Fig. 2).
(A) Normal fixation. Jejunoileal loops fixate to the parietal peritoneum through one ample mesentery extending from the duodenum–jejunal junction in the upper abdominal region toward the ileocecal valve in the right inferior quadrant. So in normal conditions the small intestine mesentery has two (2) different anchor points one far away from the other–one in the duodenum–jejunal junction and the other one in the cecum. (B) Incomplete intestinal rotation (type IIIA). The duodenum located to the right of the middle line and one high cecum condition the existence of one narrow pedicle predisposing the intestinal volvulus.
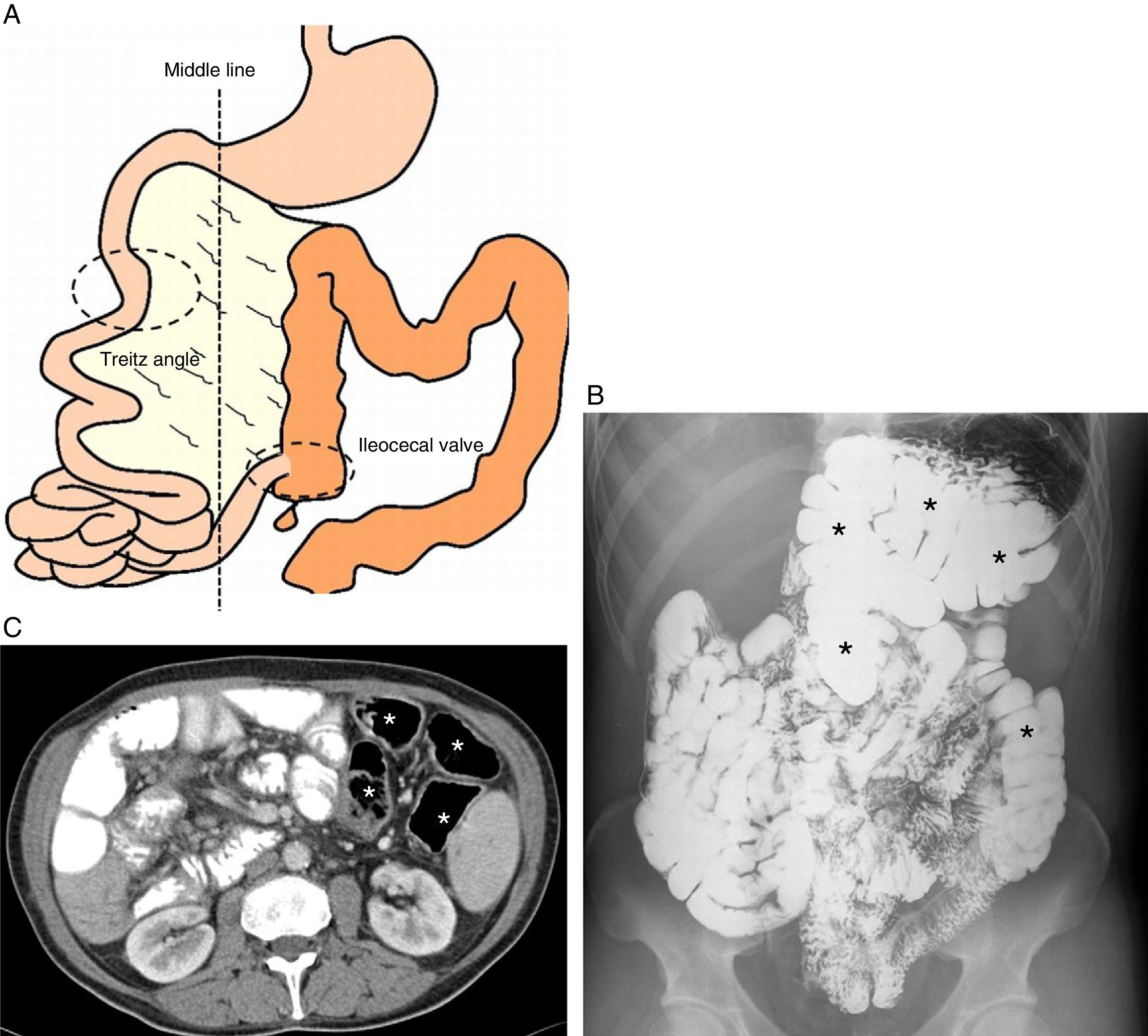
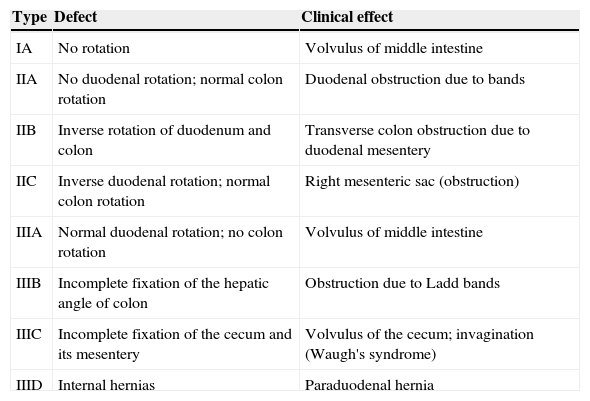
The generic term “malrotation” defines a wide continuous spectrum of abnormalities characterized by one abnormal positioning of the loops in the abdominal cavity (malposition) accompanied by anomalous fixation (mal-fixation).6,7,13. There are several variants of malrotation depending on when the normal growth of the MI is interrupted2,10,11,13,14 (Table 1). From a practical standpoint malrotation can be categorized into three (3) types2,6,13: non-rotation or type IA (Fig. 3)–when the first 90° anti-clockwise rotation occurs6,10,11,15; incomplete intestinal rotation–partial or mixed including several abnormalities due to alterations in anti-clockwise rotation of the last 180° of the intestine or colon; and inverse rotation–when the postarterial section of the middle intestine first re-entries the abdominal cavity.6,10,11,15 There is a cluster of additional abnormalities in which only the latest stage fails whether it is the loop fixation of small intestine with the appearance of internal hernia, the elongation of the cecum or the fixation of colon6,11,15 (Fig. 4).
Types of intestinal malrotation.
| Type | Defect | Clinical effect |
|---|---|---|
| IA | No rotation | Volvulus of middle intestine |
| IIA | No duodenal rotation; normal colon rotation | Duodenal obstruction due to bands |
| IIB | Inverse rotation of duodenum and colon | Transverse colon obstruction due to duodenal mesentery |
| IIC | Inverse duodenal rotation; normal colon rotation | Right mesenteric sac (obstruction) |
| IIIA | Normal duodenal rotation; no colon rotation | Volvulus of middle intestine |
| IIIB | Incomplete fixation of the hepatic angle of colon | Obstruction due to Ladd bands |
| IIIC | Incomplete fixation of the cecum and its mesentery | Volvulus of the cecum; invagination (Waugh's syndrome) |
| IIID | Internal hernias | Paraduodenal hernia |
(A) Scheme of intestinal non-rotation (type IA). The cecum is located to the left of mesenteric vessel but it is usually located in the middle line. The points of proximal and distal fixation of the mesentery are not close to one another as it happens in the incomplete intestinal rotation that reduces the predisposition of middle intestine to volvulate. (B and C) Examples of esophageal and gastroduodenal transit and CT (respectively) of different adult patients with intestinal non-rotation in whom the small intestine is located to the right and colon (asterisks) to the left of the middle line.
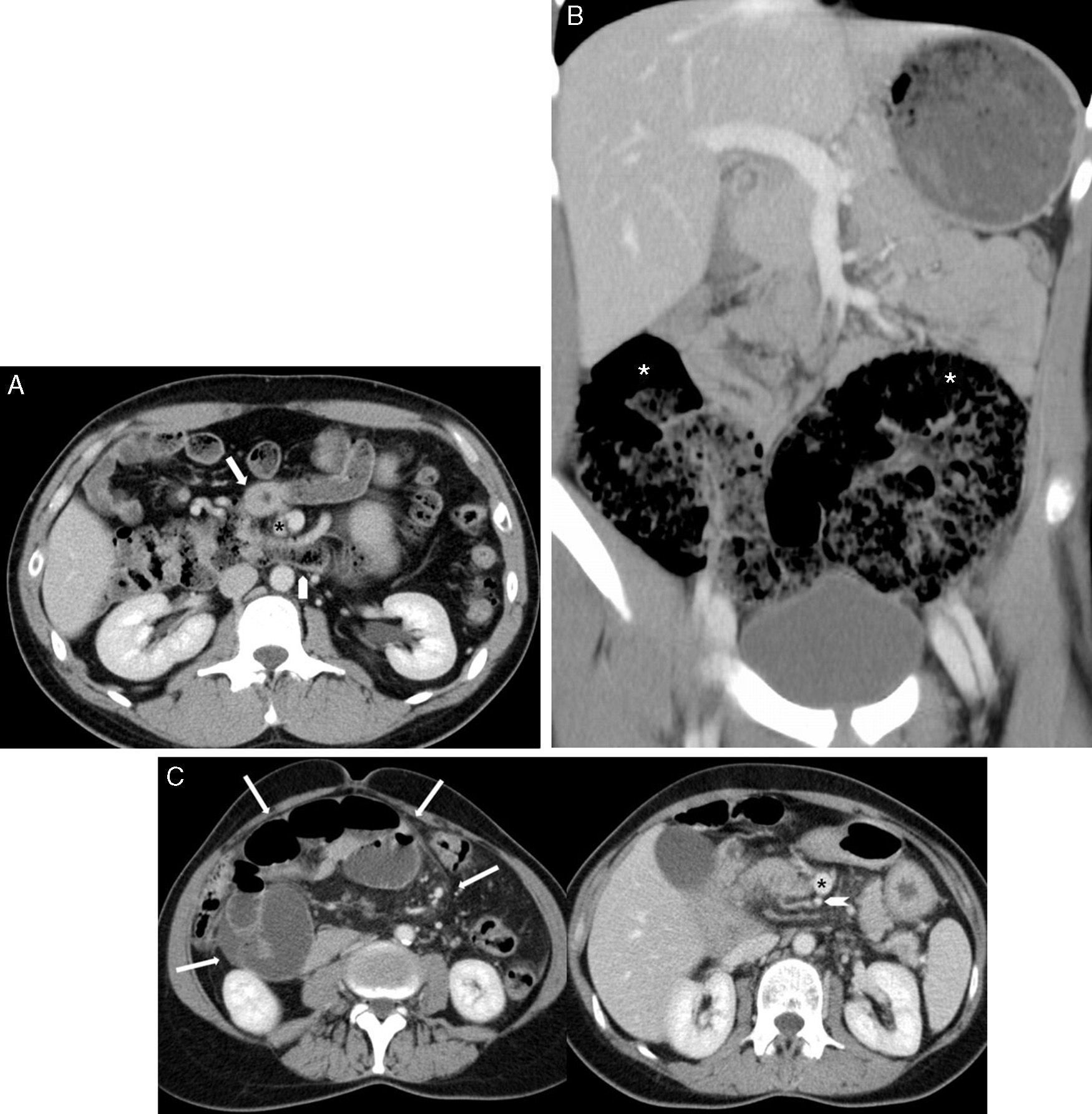
Examples of the rarest forms of malrotation. (A) Type IIB or inverse rotation of duodenum and colon–CT transverse cut of one adult patient with portal phase images with the duodenum (arrow) anterior to the superior mesenteric artery (asterisk) and transverse colon (arrow head) in posterior location; (B) Type IIIB or incomplete fixation of the hepatic angle of the colon–coronal CT image of a child with the cecum in RIF but with the hepatic and the splenic angles of colon (asterisks) mal-fixated and positioned in the inferior hemi-abdomen; (C) Type IIID–CT transverse cut of one adult symptomatic patient with one internal paraduodenal hernia (outlined by arrows in the left image) and one alteration of the relation artery (arrow head)–superior mesenteric vein (asterisk).
Intestinal mal-fixation produces peritoneal bands or Ladd bands–fibrous cords that try to fixate and stabilize the malpositioned intestine. They normally run from the cecum and proximal colon to the liver, abdominal wall and retroperitoneum usually trapping the second or third duodenum section.2,6 They are usually associated with malrotation types IIA and IIIB.11,15 Furthermore when the normal fixation points of the mesentery are close to one another the base of the mesentery shrinks creating one pedicle with a trend to spontaneously volvulate the small intestine around the axis of the SMA.2,6,7,13,14 Malrotation type IIIA usually volvulates which is rarer in malrotation types I and II.11,15
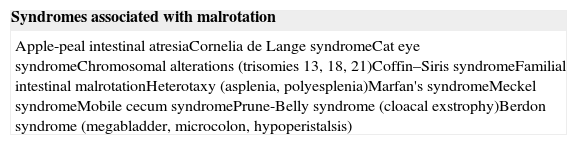
Epidemiology and clinicMalrotation usually occurs in approximately 1/500 births6,7,13,16 and is usually diagnosed in newborn babies and children. Its real incidence is not easy to estimate since it is asymptomatic and remains lifelong.2,11,13,16 Symptomatic cases only occur in 1/5000 babes that are born alive,11 up to 75% during the first month,6,7,11,16 and 80–90% during the first year of life.7,11,16 Cases occurring during the neonatal period tend to occur during the first week of life.6,10 The most common cases are type IA and type IIIA11 and even if it is true that the incidence of symptomatic cases goes down with age, the atypical patterns of malrotation go up proportionately.10 Clinically we need to assume that any intestinal malrotation patterns different from a normal pattern cause abdominal symptoms particularly in children with no other cause to blame for the clinical characteristics.2 There are numerous syndromes and abnormalities associated with 30–62% of cases of malrotation6,7,11,17 (Tables 2 and 3).
Syndromes associated with intestinal malrotation.
| Syndromes associated with malrotation |
|---|
| Apple-peal intestinal atresiaCornelia de Lange syndromeCat eye syndromeChromosomal alterations (trisomies 13, 18, 21)Coffin–Siris syndromeFamilial intestinal malrotationHeterotaxy (asplenia, polyesplenia)Marfan's syndromeMeckel syndromeMobile cecum syndromePrune-Belly syndrome (cloacal exstrophy)Berdon syndrome (megabladder, microcolon, hypoperistalsis) |
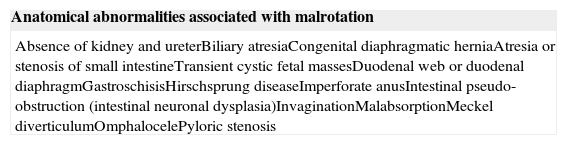
Anatomical abnormalities associated with intestinal malrotation.
| Anatomical abnormalities associated with malrotation |
|---|
| Absence of kidney and ureterBiliary atresiaCongenital diaphragmatic herniaAtresia or stenosis of small intestineTransient cystic fetal massesDuodenal web or duodenal diaphragmGastroschisisHirschsprung diseaseImperforate anusIntestinal pseudo-obstruction (intestinal neuronal dysplasia)InvaginationMalabsorptionMeckel diverticulumOmphalocelePyloric stenosis |
The symptoms of malrotation are those of an intestinal obstruction due to loop torsion-volvulation around the pedicle channel of the mesentery that fixates the loops to the retroperitoneum or due to an obstruction of the second-third duodenum section due to Ladd bands.1,2,14,18
It is rarely due to internal hernia.1 Both the symptoms and surgical emergency vary based on the degree of obstruction–that can be intermittent–and the existence or not of vascular involvement.1
The volvulus of MR is a surgical emergency due to the risk of massive extensive intestinal necrosis.19 It is an intestinal twist around the axis of the SMA that can exceed 720° that obstructs light, lymphatic and venous drainage and eventually arterial supply.6 The classic form of presentation is abdominal distension with vomits and occasionally hematochezia.2,7,19 Vomits are biliary because the obstruction is distal to the blister of Vater but it should not be considered specific of the volvulus.2,6 Most children with bilious vomits do not show mechanic obstruction yet tests to discard malrotation are justified.6,18
Peritoneal bands can compress the duodenum, the duodenum–jejunal junction or the proximal jejunum also causing obstructive symptoms with vomits and acute and intermittent abdominal pain.6 When the obstruction due to bands is intrauterine complete the findings simulate duodenal atresia.6,20 However the bands rarely cause complete duodenal obstruction or vascular involvement so there are no serious consequences to the surgical emergencies associated.12
When malrotation occurs outside the neonatal period it usually presents in a more anodyne and insidious form with chronic or recurrent abdominal pain that is exacerbated with food, intermittent vomiting, pondoestatural delay, diarrhea, and malabsortion.2,14 This makes the average diagnostic delay around 1.7 years and patients are usually diagnosed of other conditions like cholecystitis, pancreatitis, ulcerous, celiac disease, or psychological disorders.2,6,11,21
In the adult malrotation is usually asymptomatic and is diagnosed by chance through radiological examination for other causes. An elevated percentage of these adults show clinical signs of malnutrition since the intermittent chronic volvulus can alter venous and lymphatic drainage of the intestine producing malabsorption with hypoproteinemia. Other manifestations are chylous ascites, lymphoceles and melena secondary to intramural varices due to chronic venous obstruction.2,6,11 Nevertheless it has to be said that intestinal acute volvulus can occur at any age.2,7
Imaging diagnosisSimple radiologyIn any symptomatic patient it is advisable to start with a simple X-ray of the abdomen to exclude other causes.2,6 The radiological appearance of malrotation is widely variable1,2 and is unusually diagnosed with an X-ray.2,6 The most common pattern is on normal luminogram.6 Seeing proximal jejunal loops pneumatized on the right side during the early postnatal period or small intestine loops to the right and colon loops to the left in a child are findings indicative of malrotation.6,13
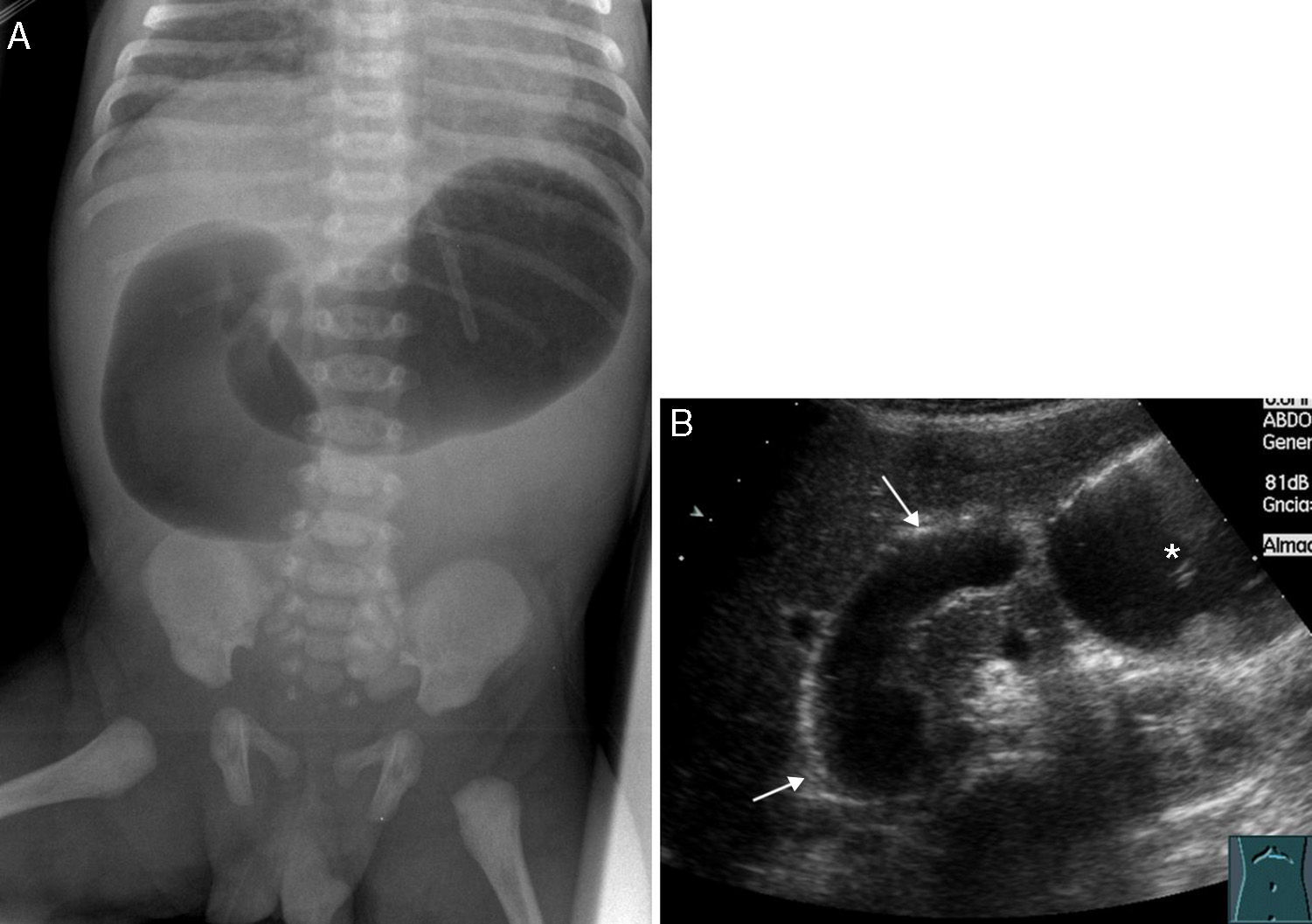
When duodenal obstruction is complete in the newborn baby the image of double bubble is with in the gastric chamber and in the proximal duodenum without distal intestinal gas–indistinguishable from duodenal atresia (Fig. 5). In some occasions continuous vomiting totally eliminates intra-abdominal gas and it is advisable to inject air through one nasogastric probe to provoke the sign of double bubble.2 This form of presentation is uncommon and duodenal obstruction is usually incomplete with gastric and duodenal distension and distal air.2 When the volvulus produces intestinal ischemia there are signs of poor prognosis like distended loops–“tubulized” or with digitiform impressions/thickened folds widely separated among them due to wall edema or ascites and with whirly disposed areas or centro-abdominal mass effect. The intestinal luminogram may disappear showing intestinal pneumatosis, portal gas, or pneumoperitoneum.2,6 In very extreme cases with loop gangrene the X-ray can simulate one low intestinal obstruction due to the interference of vascular occlusion in the reabsorption of distal gas to the obstruction.2,6
(A) Simple X-ray of a newborn baby's abdomen with prenatal suspicion of high intestinal occlusion. Double bubble sign with gastric and proximal duodenum distension and no distal air. Surgery confirmed one duodenal membrane. (B) Ultrasound transverse cut showing the image equivalent to the sign of the double bubble with two (2) liquid filled-distended cavities: stomach (asterisk) and proximal duodenum (arrows).
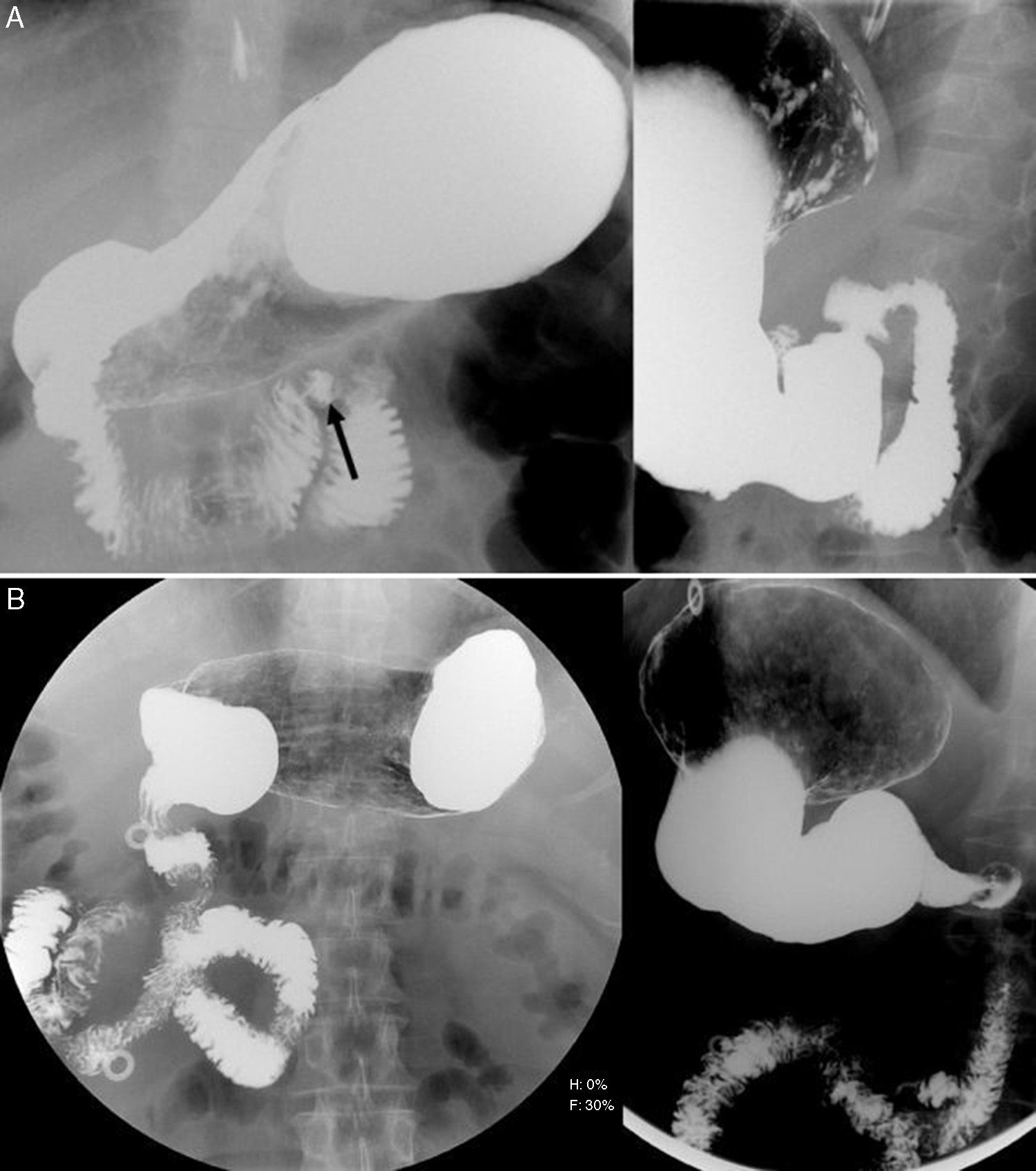
This is the modality of choice for the diagnosis of malrotation,1,8,22,23 with 93–100% sensitivity but 54% sensitivity for the intestinal volvulus only.7 Diagnosis is based on the duodenum–jejunal junction in one anomalous position and thus Treitz ligament.2,7,8,16,24 A normal duodenum has a C shape with four (4) sections or segments of which bulb and commonly one short postbulbar segment are intraperitoneal and mobile.6,9 The rest is fixated to the retroperitoneum and barely moves.3 In the anterior–posterior projection the duodenum–jejunal junction is usually located to the left of left vertebral pedicles at the level of the inferior margin of duodenal bulb or pylorus,2,3,7,9,16,24,25 at the level of the left pedicle of L1 but never again medial.3,25,26 The location of duodenum in the lateral projection is posterior with one parallel orientation in the 2nd and 4th sections always above the superior plateau of the L2 vertebral body6,7,24–26 (Fig. 6). However in cases of splenomegaly, gastric or intestinal distension, abdominal or retroperitoneal masses, scoliosis, renal agenesis and intestinal probes the duodenal–jejunal junction could be inferior or medially displaced too.6–8,26 Displacement is possible thanks to the suspensory muscle of duodenum making up the Treitz ligament and including smooth and skeletal muscular fibers.25 Malrotation should be taken into consideration in patients with an unusual redundant duodenum and differentiation can be made from normal variants like the M-shaped duodenum–also called “wandering duodenum”.3,6,7 The isolated location of proximal jejunum on the right section of the abdomen is not indicative of malrotation per se and this is why it needs to be accompanied by other suggestive findings.2,6,11 The incorrect interpretation of these signs can lead to both false positives (15%) and false negatives (3–6%) of malrotation.7,16
(A) Normal esophageal and gastroduodenal transit: to the left anterior–posterior projection (AP) in which the location of the angle of Treitz (arrow) to the left of the left pedicle of L1 can be seen; to the right–lateral projection with parallel orientation of the 2nd and 4th duodenal sections. (B) Esophageal and gastroduodenal transit in one patient with intestinal malrotation: to the left–AP with anomalous location of the angle of Treitz to the right of left vertebral pedicles and 1st jejunal loops located in the right hemiabdomen; to the right–lateral projection with one anomalously low location of duodenum.
The study was done with barium except in children in a poor state of health and suspicion of intestinal suffering to whom non-ionic hydro-soluble contrast was administered.2,6,7 We can use one nasogastric probe up to the duodenum to stretch and take a good look at the duodenal frame.6 The passing of contrast to the jejunum needs to be checked real time to be able to identify the location of the duodenum–jejunal junction and then register it in anterior–posterior and lateral projections.2,7 When contrast surpasses the duodenum the proximal jejunal loops overlap in both projections compromising the assessment of the duodenal course.2,7 Too much contrast should not be administered to avoid stretching the stomach completely and obstructing the duodenum or the displacement of the angle of Treitz.7 Manual displacement to the right of the duodenal–jejunal junction could help. In malrotations the angle of Treitz loses mobility or after the decompression maneuver would not go back to its initial position.6,24 Even though initially the angle of Treitz might be well positioned the fact that it might not return to its initial position after the decompression can be a mild sign of malrotation.6,24 The reliability of this sign is greater in children under 4 years since ligament laxitude is physiological and it is easier to confirm anomalies through the displacement of the angle of Treitz.3,7,16,24 In older children the reliability of this sign is lower due to the physiological reduction of duodenal mobility and the greater resistance of the abdominal wall musculature to duodenum–jejunal junction displacement.7,26,27 When in doubt late acquisitions can be performed to assess the cecum location.1,7,16
The typical image of the MI volvulus is the “corkscrew” or “spiral” image of distal duodenum and proximal jejunum right on the center of the abdomen2,11,18 (Fig. 7A). The intestinal lumen narrows with partial or complete obstruction.5 The duodenum proximal to the obstruction is usually mildly dilated and in the obstruction site can be cone shaped or peaked loop usually with caudal extension.6,18,24 If the obstruction is complete, barium will not pass to the volvulated loops so the “corkscrew” image just would not be seen.2,6 In cases of non-occlusive 180° volvulation especially in the absence of biliary vomiting–14% of IM volvuli of the digestive transit cannot be diagnosed since the torsion point transition does not cause transition in the caliber of loops.26
Ladd band without intestinal volvulus can also generate differences in the caliber of the duodenum proximal and distal to the obstruction usually between the second and third sections with a typical Z configuration of distal duodenum and proximal jejunum2,7 (Fig. 7B). Z-shape can be similar to the volvulus “corkscrew” image and associated or not with intestinal obstruction.2,6,11,27
Opaque enemaIt is not being used today2,6 and is reserved for cases with uncertain gastroduodenal transit only.2,6,16 The main reason is that the cecum location is more variable than the duodenum–jejunal junction both in normal patients and in cases of malrotation.16 Fifteen (15) per cent of the population has a mobile cecum2,6,7 and in 20% of malrotations the cecum is in a normal position.2,6,11,14 Both the variations of positioning and the mobility of the cecum are customary and the limit between normal and pathologic variations is not well defined since it is all part of a continuous spectrum.2,6 Loop distension of the small intestine can displace the location of both the cecum and proximal colon while leading to an erroneous diagnosis of malrotation.1
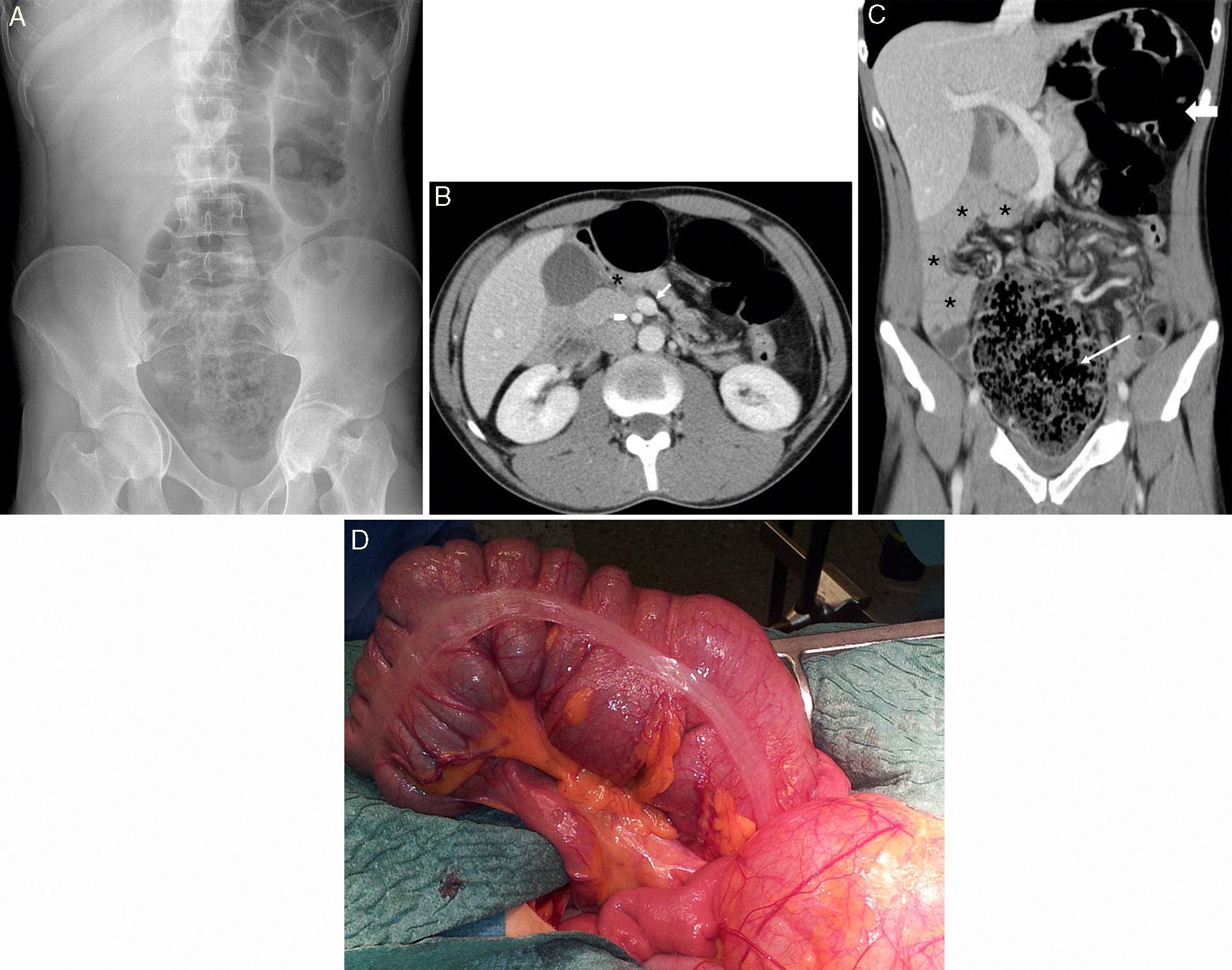
The cecum's excessive mobility associated with its mal-fixation predisposes it to volvulation.28 The obstruction of colon due to malrotation is rare and it can occur like an inverse rotation of the duodenum and colon in which the transverse colon passes behind the SMA while it can be partially occluded both by the mesenteric vessels and the peritoneal bands.6,11 There are times that the section of colon partially occluded volvulates usually in the right colon or transverse colon7,11 (Fig. 8).
Thirty-five-year-old patient without a significant pathological history presenting at ER with abdominal pain of 36-h duration–mainly hypogastric; sensation of dysthermia and no bowel movement in 48h. (A) The simple X-ray shows the anomalous location of the air of colon with the cecum apparently located in the middle line in the hypogastrium and the dilation of the loops of colon being immediately distal in the left hypochondrium. (B) CT scan shows one anomalous relation between the artery-superior mesenteric vein and the vein (arrow) located ahead of it and to the left of the artery (arrow point), and the angle of Treitz in an anomalous location (asterisk). (C) The small intestine loops (asterisk) are located to the right of the abdomen, the cecum in the middle line (narrow arrow) and left colon (wide arrow) in the left hemiabdomen. (D) Surgery confirmed one volvulus of right colon with multiple colon adhesions with the epiploon and the mesos.
Even though it is less sensitive (67–100%) and specific (75–83%) than the duodenal transit for the diagnosis of malrotation,16 it is very useful to find it early and then diagnose its complications rapidly and at a low cost.2
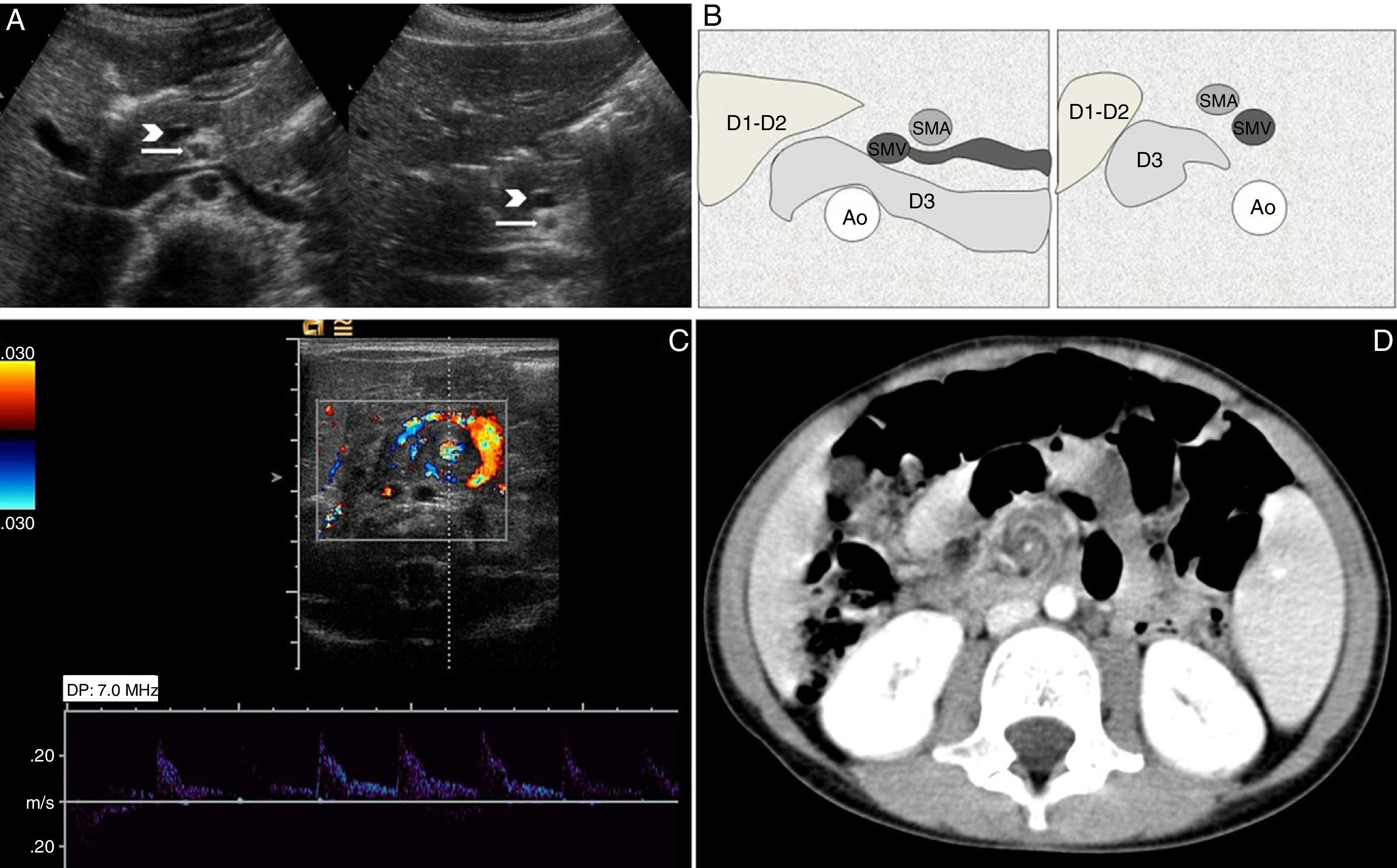
The diagnostic suspicion is established after assessing the location relative to the artery and the superior mesenteric vein (SMV).2,6,29 The SMA is constant while mesenteric veins show the growth and location of intestinal loops.6 The normal relation between the SMA and SMV is the same relation we can see between the aorta and the inferior cava vein, e.g. the vein is located to the right of the artery in the axial plane at the level of the junction between the SMV and the portal vein.2,3,6,23 Instead in the malrotation of the vein it can usually be found to the left of the artery,2,6,16 yet it is not a sign specific or sensitive enough to be able to diagnose malrotation; the association of inverted SMA/SMV has been reported in patients with normal rotation and 30% of patients show malrotation and a normal SMA/SMV relation.2,6,23,29,30 Diagnostic sensitivity is even lower when the SMV is located right ahead of the SMA26,31,32 (Fig. 9A). Thus an abnormal vascular relation is not pathognomonic and leads us to take another test preferably one intestinal transit test.2,6,8
(A) Ultrasound transverse images of two (2) patients the one on the left without malrotation showing one normal relation artery (arrow)-superior mesenteric vein (arrow head) and the one on the right showing intestinal malrotation with the vein (arrow head) located just ahead of the artery (arrow). (B) Scheme in axial cuts of the location of the third duodenal section (D3) both in normal situation (to the left of the image) as in intestinal malrotation (to the right of the image). (C and D) Ultrasound image and CT of whirlpool sign–typical of the middle intestine. Ao: aorta.
Some authors propose the use of ultrasounds with oral or injected liquid through a jejunal probe to assess the location of the angle of Treitz yet it is a complex proceeding in today's routine clinical practice and we do not have large studies comparing its diagnostic precision with that of gastrointestinal transit.1,6,33 Recently the fact of confirming the retroperitoneal position of the third duodenal section in its journey between the aorta and the SMA in the axial plane, caudal to the left renal vein and one jejunal vein through the aortomesenteric space3,23,34,35 has been described as the most reliable sign to preclude malrotation (Fig. 9B). This sign is not infallible since the retroperitoneal location of the third section makes malrotation to be an unlikely but not impossible event.36
Ultrasound is the chosen modality when being suspicious of MI volvulus (sensitivity 92%; specificity 100%).1,2,6,8,16,19 The most characteristic ultrasound sign is whirling vessels entering one central-abdominal solid mass that corresponds with the airless volvulated loops.2,6 This sign known as “whirlpool sign” translates the dragging of the mesos and its vascular structures from the loops surrounding the SMA that revolve around the SMA, clockwise being the direction of the mesenteric turn defined as cranial-caudal19,35,37 (Fig. 9C). It should not be mixed up with the anti-clockwise rotation of SMV around the SMA (barber pole sign)–non-specific sign that can be seen in the normal population due to one vascular variable–jejunal branch proximal to the SMV surrounding the SMA anti-clockwise before joining the SMV.35,38 Other ultrasound findings of the volvulus include one truncated SMA, one hyperdynamic and pulsatile SMA and one dilated distal SMV–all signs correlated with the classic findings of volvuli associated with malrotation as seen in the angiography.2,19,36
CT and MRIMost malrotations in adults are found incidentally in CT and MRI studies performed for other reasons.13 These modalities are not usually part of daily routines for the diagnosis of malrotation but they can be very useful in doubtful cases to be able to confirm the diagnosis and rule out other processes.2,6 They are not used in children due to the doses of radiation associated with CT and the low resolution of MRIs.6
Other than intestinal malposition and the SMA/SMV relation they allow us to assess extraintestinal non-evident signs in conventional studies.2,13 Situs or organ growth abnormalities like hypoplastic pancreatic uncinate processes are due to the interference of the rotation of the pancreatic primordium that usually rotates together with the duodenojejunal loop.2,6,39 In the case of volvulus other than the classical signs they can help us identify loop hypoperfusion in cases of intestinal necrosis.2,6,13,16,40
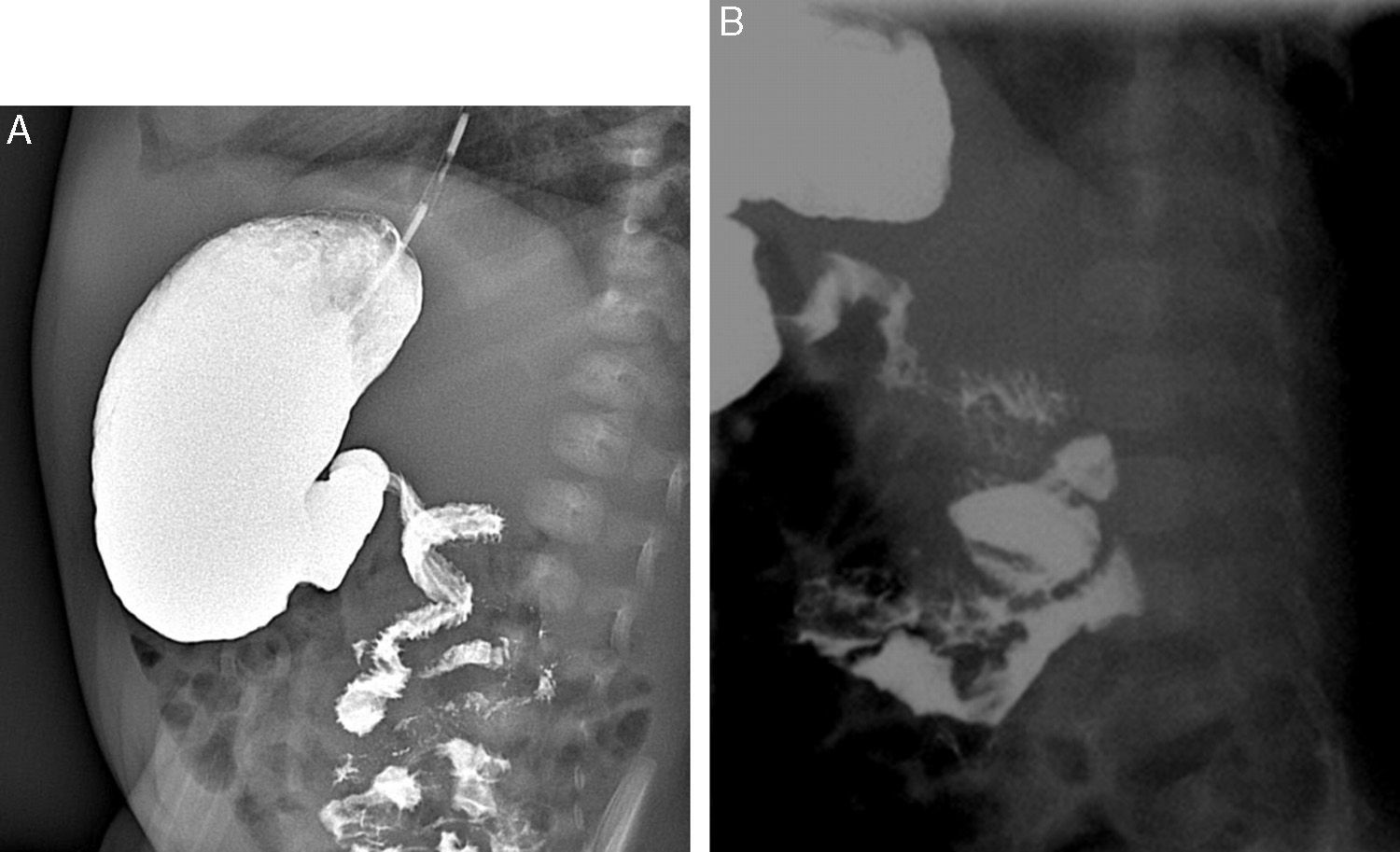
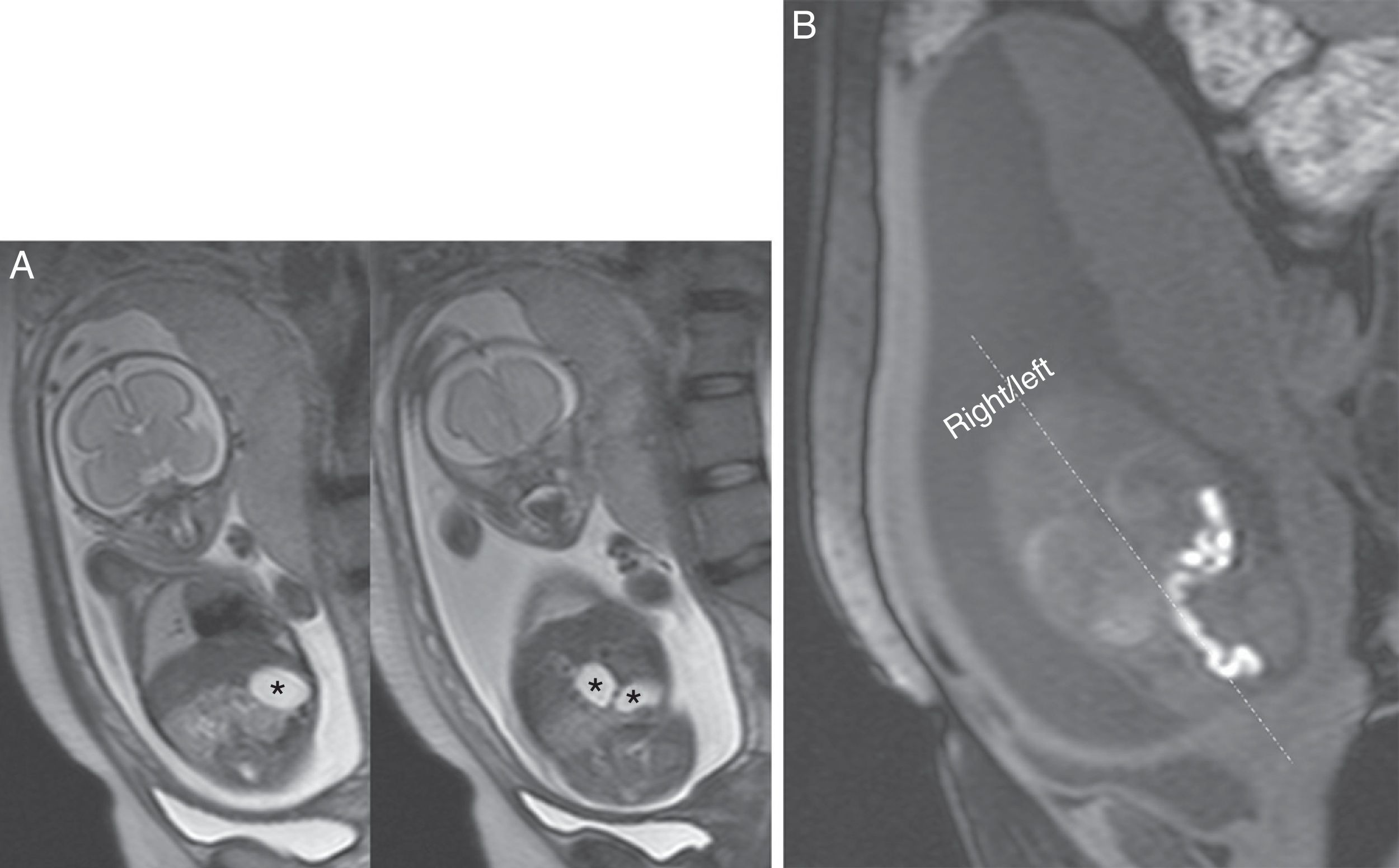
MRI is also an efficient complementary modality to ultrasound for prenatal studies.39,41 During growth the fetus swallows the amniotic liquid that acts upon the gastrointestinal tract like a natural contrast agent in the T2-weighted sequences allowing us to identify both the stomach and loops as hyperintense structures. While the viscosity of the intestinal content increases along the digestive tube the signal of meconium in T2 decreases but increases in T1. The loops of colon are seen hypointense in T2 and hyperintense in T1 and this is why it is possible to detect anomalous intrauterine location42 (Fig. 10). Similarly duodenal obstruction due to peritoneal bands can be suspected when two (2) big abdominal cavities filled with liquid representing the dilated stomach and duodenum–sign of double bubble–can be seen.6,20,42 Rarely the MI volvulus occurs weeks or months before delivery and is not usually lethally intrauterine fetal trauma.6,43 The radiologic findings of prenatal volvulus are usually non-specific like free peritoneal liquid and dilated loops that can be hypointense in T2 in cases of hemorrhagic necrosis.43,44 The intestinal content passing through the peritoneal cavity can create one pseudo-cyst, and originate one fibroadhesive peritonitis with calcifications or intestinal atresia seen at birth only. Some cases of syndrome of short intestine can be secondary to intrauterine volvuli with reabsorption of the infarcted loop and self-anastomosis of all those loops feasible to re-establish intestinal transit.6,45
MRI of a fetus with intestinal malrotation and upper intestinal occlusion due to Ladd bands. (A) T2-weighted sequences showing the sign of the double bubble can be seen. (B) T1-weighted sequence showing the anomalous location of colon seen as a hyperintese tubular structure in the left side of the abdomen. In the image it is seen to the right (right) and left (left) of the abdomen to the fetus.
When in presence of biliary vomiting in newborn babies in good health we should suspect intestinal malrotation. Initially it is recommended to take an X-ray and if the sign of double bubble is confirmed surgery should follow immediately. The next exploration indicated is ultrasound. In one patient with symptoms suggestive of volvulus the whirlpool sign is more than enough to establish the diagnosis without further delay in the intervention. The altered SMA/SMV relation is likely to be the only sign will make us complete the study with one gastrointestinal transit test. CT and abdominal MRI are reserved for children with exceptional cases. CT is one of the preferred diagnostic modalities when being suspicious of volvuli in adult patients.
Even though malrotations can be diagnosed in many cases with one image modality only in difficult cases the radiologist needs to perform several explorations or even repeat them to be able to confirm or rule out the diagnosis. When in doubt and once all diagnostic tools have been used surgery should be taken into consideration.
Ethical responsibilitiesProtection of humans and animalsAuthors confirm that in this investigation no experiments have been performed in human beings or animals.
Data confidentialityAuthors confirm that the protocols of their centers have been followed on matters concerning the publishing of data from patients.
Right to privacy and informed consentAuthors confirm that they have obtained the written informed prior consent from patients and/or subjects appearing in this article. This document is in the possession of the corresponding author.
Authors contributionsManager of the integrity of the study: EBG, ATA; Original Idea of the Study: EBG, ATA, CDF; Study Design: EBG, ATA; Data Mining: EBG, ATA, CDF, CMM, ACT; Data Analysis and Interpretation: EBG, ATA, CDF, CMM, ACT; Statistical Analysis: N/A; Reference Search: EBG, ATA, CDF, CMM; Writing: EBG, ATA, CDF, CMM, ACT; Manuscript critical review with intellectually relevant contributions: EBG, ATA, CDF, CMM, ACT; Final Version Approval: EBG, ATA, CDF, CMM, ACT.
Conflict of interestsNone declared.
The authors thank Dr. Toni Malet Munté, MD; Dr. Marta Andreu Magarolas, MD and Dr. Jordi Puig Domingo, MD from the unit of Radiology of the Hospital Universitario Parc Taulí de Sabadell for their collaboration during the final review of this article and to Prof. Jorge C. Berriatúa for translating this manuscript into medical English language.
Please cite this article as: Ballesteros Gómiz E, Torremadé Ayats A, Durán Feliubadaló C, Martín Martínez C, Caro Tarragó A. Malrotación-vólvulo intestinal: hallazgos radiológicos. Radiología. 2015;57:9–21.