Traumatic brain injury (TBI) is a common reason for pediatric emergency room visits. Surgical intervention for mild TBI is rarely necessary in children aged <2 years, but the intracranial findings can influence the management of the patient. This paper aims to evaluate the impact of computed tomography (CT) in the management of children aged <2 years with mild TBI and linear skull fractures on plain-film X-rays.
Material and methodsThis retrospective descriptive study analyzed skull X-rays obtained in children <2 years old attended for mild TBI in the emergency room of our tertiary hospital over a 4-year period.
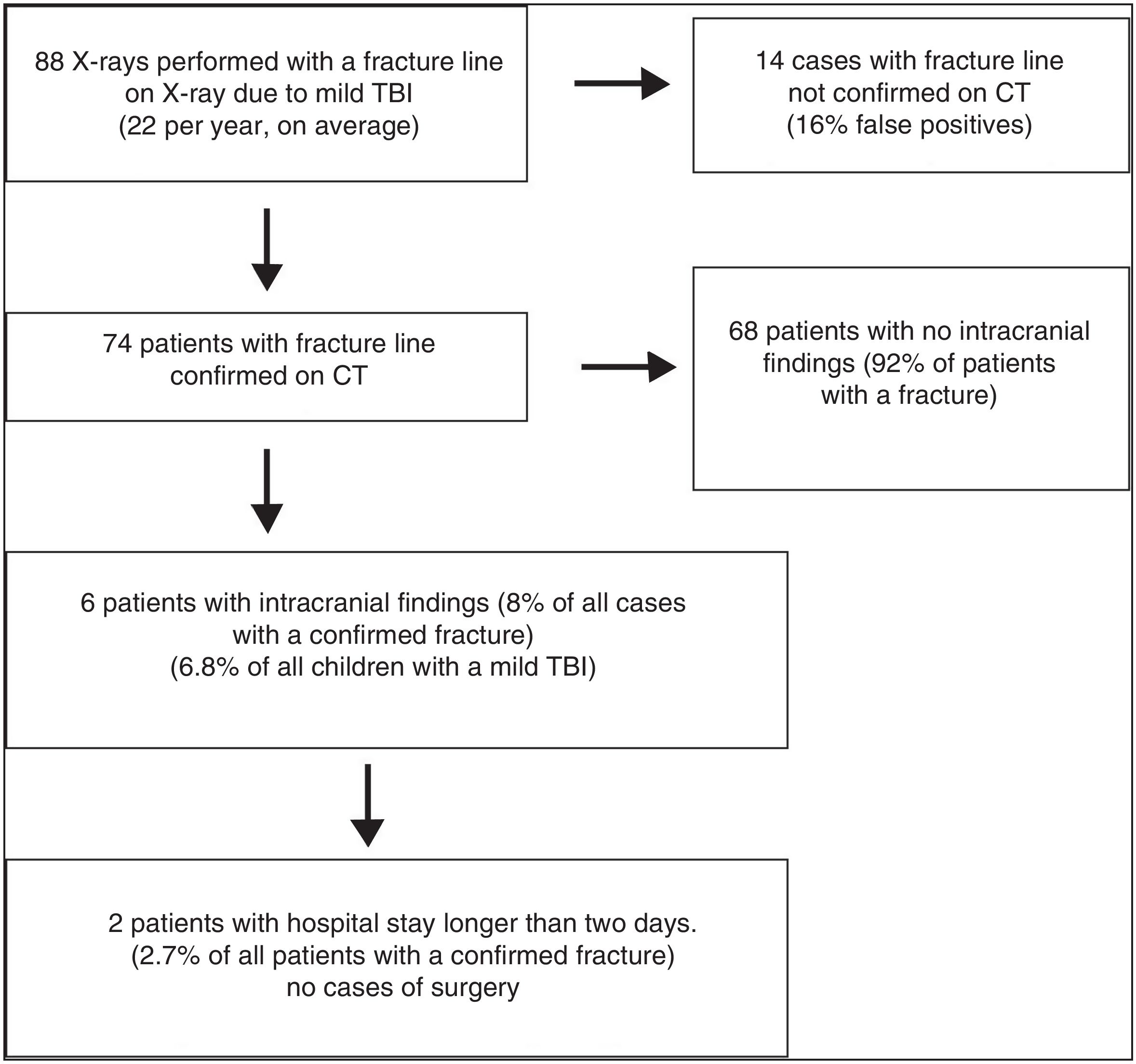
ResultsA total of 88 CT studies were done for suspicion of linear skull fractures on plain-film X-rays. Fractures were confirmed in 74, representing a false-positive rate of 16%. Of the 74 infants with confirmed fractures, intracranial CT findings were normal in 68 (92%) and abnormal in 6 (8%). Two patients (2.7% of all patients with confirmed fractures) required hospital stays longer than 2 days; the other four patients with abnormal intracranial findings were discharged within 48 h of admission. None of the cases required surgery.
ConclusionSystematic CT studies do not seem justified for all children aged <2 years with TBI and low/intermediate risk of intracranial lesions, even when they have linear skull fractures. In the absence of risk factors, we propose individualizing the imaging study based on clinical criteria.
El traumatismo craneoencefálico (TCE) constituye un motivo frecuente de consulta en urgencias pediátricas. La necesidad de intervención quirúrgica en pacientes menores de 2 años con TCE leve es mínima, pero los hallazgos intracraneales pueden influir en el manejo del paciente. El objetivo de este trabajo es valorar el impacto de la TC en el manejo de los niños menores de 2 años con TCE leve que presentan una fractura lineal de cráneo en la radiografía convencional.
Material y métodosEstudio descriptivo y retrospectivo en el que se analizan las radiografías de cráneo practicadas a pacientes menores de 2 años que fueron atendidos en el área de urgencias de nuestro hospital de nivel terciario por TCE leve en un período de 4 años.
ResultadosSe realizaron 88 exploraciones de tomografía computarizada (TC) realizadas por sospecha de fractura lineal de cráneo en radiografía. Se confirmó la fractura en 74 de ellos (16% de falsos positivos). De los 74 niños con diagnóstico confirmado de fractura, la TC fue normal en el 92% de los estudios y mostró hallazgos intracraneales en 6 casos (8% de los casos con fractura). Dos casos requirieron ingreso superior a 2 días (2,7% de todos los casos con fractura) y en los 4 casos restantes la estancia hospitalaria no superó las 48 horas. En ningún caso se requirió cirugía.
ConclusiónNo parece justificada la realización de una TC craneal de forma sistemática en niños menores de 2 años con TCE y bajo/intermedio riesgo de lesión intracraneal, incluso con fractura lineal de cráneo. En ausencia de factores de riesgo, proponemos individualizar el estudio de imagen basándose en el criterio clínico.
Traumatic brain injury (TBI) is defined as physical or functional abnormality of any magnitude, mechanism or severity inflicted on the cranial cavity and its contents.1 TBI represents a common reason for visits to paediatric emergency departments. It is estimated that one in ten children will suffer from a significant TBI at some point in childhood, especially before age two.2 Different factors promote traumatic injuries in infants, such as a larger ratio of skull surface to other body surfaces and relatively weak cervical musculature.3 A higher risk of intracranial damage has been reported in young children, especially under six months of age.3,4
A TBI is believed to be mild when it presents without any focal neurologic signs, the child responds to voice or touch and the child has a level of consciousness greater than 13 on the Glasgow Coma Scale.5,6 In the mechanism of injury of a mild TBI, traffic accidents are ruled out; most cases are due to falls from the child’s own height or from a maximum of a metre and a half. Given the inherent difficulty of taking medical histories in these patients, subtle signs such as lack of visual contact, irritability, somnolence and acute crying take on greater importance. All these signs are indicators of an increased likelihood of intracranial injury (ICI).2
Although a physical examination and medical history are essential in children under two years of age, an increased risk of ICI is assumed in the presence of a skull fracture; hence, the guidelines of the Sociedad Española de Pediatría [Spanish Paediatrics Association] call for a computed tomography (CT) scan. Regarding the clinical course of patients under two years of age with a mild TBI, series have agreed that the need for associated neurosurgery is less than 1%.6–9 In addition, the percentage of associated intracranial complications in this age group ranges from 8% to 20%.6–9
Beyond the need for neurosurgery and the detection of intracranial bleeding, we feel it is important to determine whether intracranial findings on CT are clinically significant. We are not aware of any publications confirming whether these complications are associated with a longer hospital stay or a substantial change in the patient’s clinical management and subsequent imaging follow-up.
The objective of this study was to assess the impact of CT on the management of children under two years of age with a mild TBI who present a linear skull fracture on conventional X-ray.
Material and methodsThis was a descriptive, retrospective study in which skull X-rays taken in patients under two years of age who had received care in the emergency department at our tertiary hospital due to a mild TBI in a four-year period between 2014 and 2017 were analysed.
For a TBI to be considered mild, it should occur as a result of low-energy mechanical trauma, i.e. a fall from one’s own height or from one and a half metres at most, and the patient should have a level of consciousness greater than 13 on the Glasgow Coma Scale. The imaging protocol at our centre included an anteroposterior and lateral X-ray of the skull in patients presenting parietal-temporal haematoma and in those with a TBI that had not been witnessed, to demonstrate the presence of cranial vault fracture. When a skull fracture was detected on X-ray, a cranial CT scan was performed on an emergency or early deferred basis (<10 h). In the event of spontaneous non-collaboration, sedation was administered with the help of an anaesthetist. CT scans were performed with two Philips scanners, one with 64 detectors and the other with 256 detectors (from the scheduled scan area and the emergency scan area, respectively) with helical acquisition (120 Kv, 200−250 mA, thickness of 3 mm and reconstruction interval of 1.5 mm), thus enabling 3D volumetric and maximum-intensity projection (MIP) reconstructions.
Patients with a linear cranial vault fracture line were included; patients with a diastatic fracture, a depressed fracture, impairment of the skull base or bleeding diathesis were excluded. All tests were reported by paediatric radiologists with 20 years of experience on average. Finally, medical histories were reviewed to determine the patient’s length of stay in the emergency department or on the hospital ward, subsequent neurosurgery (if any) and follow-up with imaging tests.
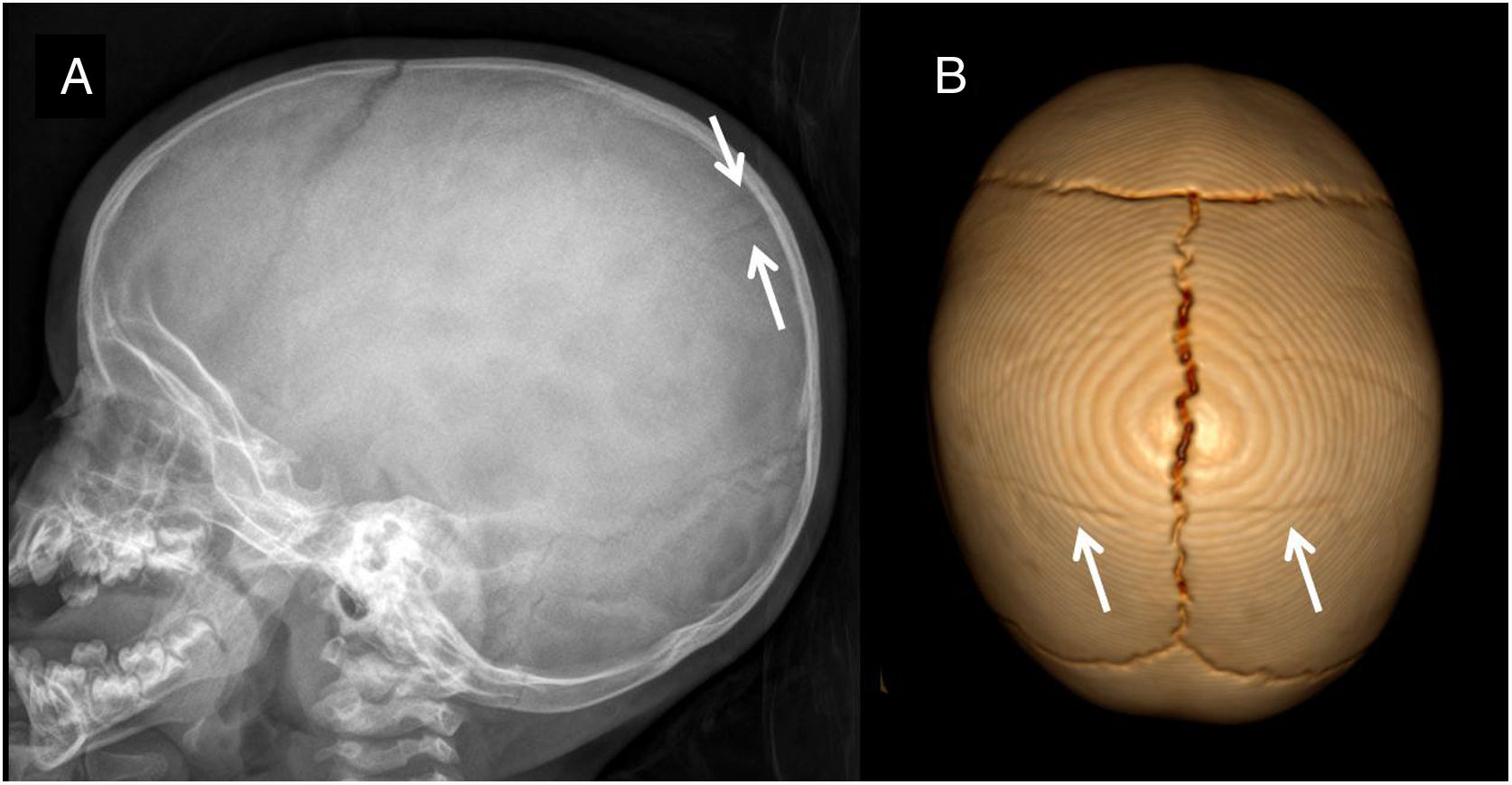
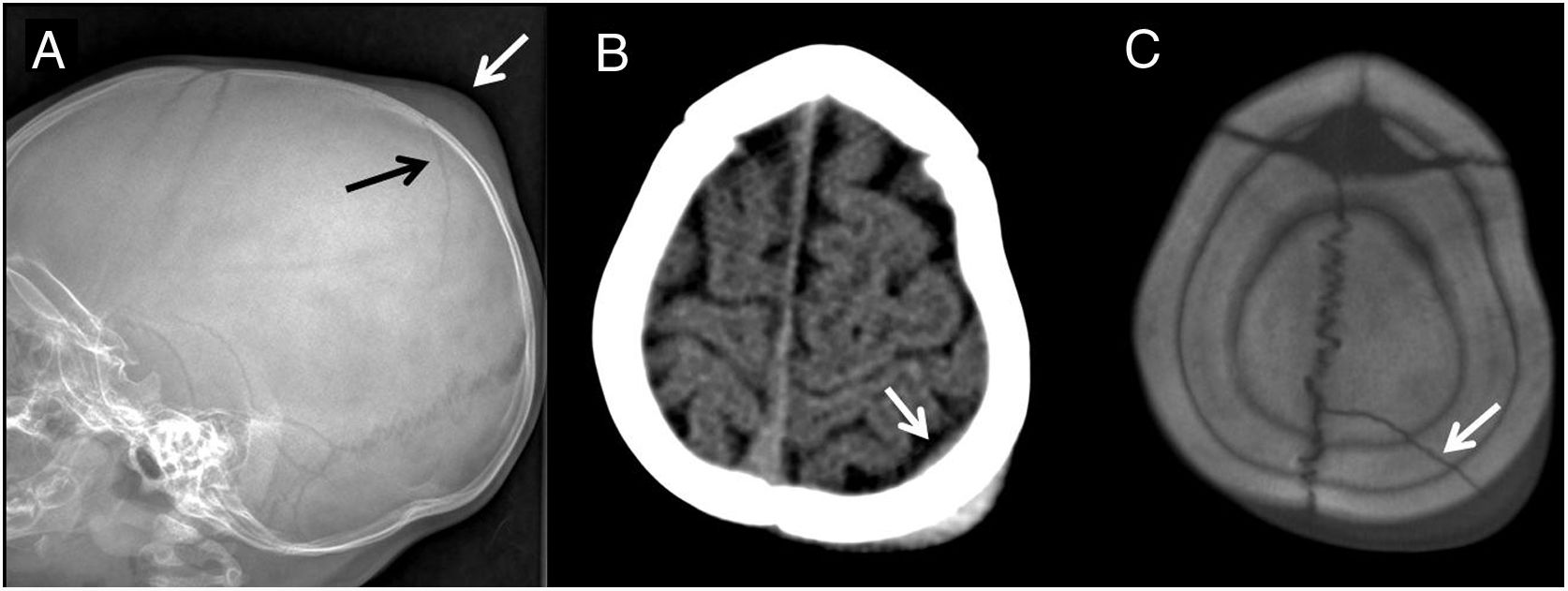
ResultsIn the period reviewed, 88 CT examinations were performed due to suspicion of a linear skull fracture on X-ray. The finding was confirmed in 74 of them; hence, there were 14 false positives with X-ray (16%) which corresponded to vascular grooves or accessory fissures (Fig. 1). CT did not show abnormalities in any of the false positives on X-ray. Among the 74 children with a confirmed diagnosis of linear skull fracture, the CT scan was normal in 92% of the studies and showed intracranial findings in six cases (8%). Linear extra-axial bleeding was demonstrated in the six children with a positive CT scan (Fig. 2). Just two children required hospital admission for more than two days (2.7% of all cases with fracture); the four remaining children had a hospital stay no longer than 48 h. None of the patients required emergency or trauma-related surgery (Fig. 3).
(A) Parietal fracture line marked with black arrow. Soft-tissue haematoma marked with white arrow. (B) Transverse computed tomography (CT) image showing extra-axial bleeding measuring a millimetre, marked with white arrow. (C) CT image with bone filter showing the fracture, marked with arrow.
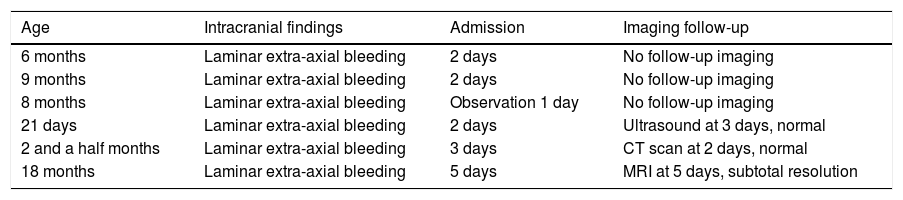
Regarding the imaging follow-up of the four patients with a stay lasting less than two days, three were discharged with no imaging tests, and the fourth was a 21-day-old neonate who, prior to discharge, had a transfontanellar ultrasound which showed no findings of pathological significance. As for the two patients with a longer stay, one was discharged after three days following a CT scan which showed resolution of the patient’s extra-axial bleeding; the other patient, following a five-day admission, underwent an MRI prior to discharge which identified subtotal resolution of the patient’s extra-axial bleeding. None of the patients subsequently made a visit to the emergency department in relation to the TBI (Table 1).
Follow-up for patients with intracranial findings.
| Age | Intracranial findings | Admission | Imaging follow-up |
|---|---|---|---|
| 6 months | Laminar extra-axial bleeding | 2 days | No follow-up imaging |
| 9 months | Laminar extra-axial bleeding | 2 days | No follow-up imaging |
| 8 months | Laminar extra-axial bleeding | Observation 1 day | No follow-up imaging |
| 21 days | Laminar extra-axial bleeding | 2 days | Ultrasound at 3 days, normal |
| 2 and a half months | Laminar extra-axial bleeding | 3 days | CT scan at 2 days, normal |
| 18 months | Laminar extra-axial bleeding | 5 days | MRI at 5 days, subtotal resolution |
CT: computed tomography; MRI: magnetic resonance imaging.
Patients with a linear skull fracture and a normal CT scan were kept under observation in the emergency department for at most a day. All patients with a confirmed fracture underwent clinical follow-up after a month in outpatient neurosurgery consultations.
DiscussionMild TBI is any abnormality on the skull surface due to a low-energy mechanism that presents no focal neurological symptoms and has a score of 14–15 on the Glasgow Coma Scale.1,2 Infants and young children are more vulnerable to fracture in TBI as they have a thinner, less rigid diploe. The higher water content and the lower degree of myelinisation promote diffuse axon damage in acceleration/deceleration mechanisms.2 A larger ratio of skull surface to other body surfaces and relatively weak cervical musculature in infants are other factors that must be borne in mind. These physiological and anatomical conditions decisively establish two major groups: those over and those under two years of age.
Transfontanellar ultrasound is not indicated in patients’ initial diagnosis or follow-up. Most traumatic brain injuries affect the extra-axial space and the brain tissue of the convexities is more complicated to assess using ultrasound. In our case, an outside-of-protocol ultrasound was performed on a neonate given the family’s anxiety to monitor parasagittal bleeding visualised on CT.
There is a consensus that a CT scan should be directly performed in fractures associated with a high risk of ICI such as penetrating, palpable, diastatic and depressed fractures; non-accidental trauma; suspected skull base impairment; focal neurological deficit; or seizures following a symptom-free period.6,10–12 It is a quick examination method and one that is highly available in hospital emergency departments. On the other hand, it carries the known disadvantages of ionising radiation and a frequent need for sedation in this age group.
A skull X-ray is a sensitive technique for identifying linear cranial vault fractures. However, even experienced radiologists face uncertainties around the differential diagnosis between fracture lines and vascular impressions or accessory sutures. In our series, the rate of false positives for a linear fracture line (suspected on X-ray but not demonstrated on the subsequent CT scan) was as high as 16% (Fig. 1). In the absence of an adjacent soft-tissue cephalohaematoma, radiolucency rarely corresponds to a fracture (Fig. 2).
Children under the age of two with a mild TBI associated with self-limiting vomiting, lethargy, irritability, behavioural changes, non-frontal scalp lesions and/or loss of consciousness lasting seconds are at intermediate risk of ICI. In these cases, those in which the traumatic event was not witnessed and those with an even lower suspicion of ICI, management is debated. Close clinical observation for no less than six hours and imaging tests are recommended.2,12 Regarding imaging, there has been a trend towards performing a CT scan of the skull with attention to clinical criteria, without including the initial X-ray of the skull.1,2,6,11,12 However, at our centre, the criteria were clinical and radiological. This protocol enabled us to compile all confirmed fractures in mild TBIs with low to intermediate suspicion of ICI in children under the age of two.
The percentage of intracranial findings related to skull fracture lines reported in the scientific literature has ranged from 8% to 20%, similar to what we found in our review, which in general dealt with cases featuring extra-axial bleeding with a thickness of a millimetre.6,8,9,11 The minimal percentage of cases requiring surgery reported in the literature, hovering around 1%,6–9 was also consistent with the fact that none of the cases in our series required surgery.
ConclusionWe report a series of 88 children with mild TBI in whom a linear skull fracture was suspected on X-ray. According to the criteria at our centre, all children underwent a CT scan, which demonstrated a rate of false positives for fracture on X-ray of 16%. This underscores the difficulty of distinguishing between fracture lines and vascular impressions or accessory sutures, even for experienced radiologists with a background in paediatrics. None of the false positives showed findings on CT. Among all other children with a confirmed fracture, just 8% had intracranial abnormalities, specifically extra-axial bleeding which was not taken as an indication for neurosurgery. Only two children remained admitted for more than two days; they were managed according to clinical criteria. Therefore, systematic cranial CT scanning does not appear to be justified in children under two years of age with a TBI and a low/intermediate risk of ICI, even with a linear skull fracture. In this age group, in the absence of risk factors such as clotting disorders and bleeding diathesis, we propose taking a personalised approach to imaging studies based on clinical discretion rather than subordinating them to the presence of a linear skull fracture.
Authors- 1.
Study integrity: AMF and FMS.
- 2.
Article concept: AMF and FMS.
- 3.
Article design: AMF and FMS.
- 4.
Data acquisition: AMF.
- 5.
Data analysis and interpretation: Not applicable.
- 6.
Statistical processing: Not applicable.
- 7.
Literature search: AMF, FMS, RLS, JAD, JJP and DVC.
- 8.
Drafting of the paper: AMF and FMS.
- 9.
Critical review of the manuscript with intellectually significant contributions: AMF, FMS, RLS, JAD, JJP and DVC.
- 10.
Approval of the final version: AMF, FMS, RLS, JAD, JJP and DVC.
The authors declare that they have no conflicts of interest.
Please cite this article as: Montoya-Filardi A, Menor Serrano F, Llorens Salvador R, Veiga Canuto D, Aragó Domingo J, Jurado Portero JC. Fractura lineal de cráneo en el lactante con traumatismo craneoencefálico leve: influencia de la tomografía computarizada en su manejo. Radiología. 2020;62:487–492.