Tumours of the carotid body are uncommon neoplasms that originate in the neuroectoderm. These tumours are slow growing but well vascularised and very destructive. Between 5% and 13% of carotid body tumours are malignant, behaving aggressively at the local level, invading the adjacent lymph nodes, and resulting in remote metastases. We present the case of a 60-year-old man who was examined for pain and paresthesias in his arm. Magnetic resonance imaging showed a large tumour in the left carotid space. Histologic study of a biopsy specimen from the tumour revealed that it was a paraganglioma. Further studies to determine the extent of disease detected metastases in bone and lung, confirming the tumor's malignancy.
Los tumores del cuerpo carotídeo son neoplasias poco frecuentes, de lento crecimiento, muy destructivos y vascularizados, que tienen un origen neuroectodérmico. Los tumores malignos representan el 5-13% de los casos y presentan un comportamiento agresivo local con infiltración de los ganglios linfáticos adyacentes o metástasis a distancia. Presentamos el caso de un varón de 60 años al que en el estudio por dolor y parestesias en miembro superior se le realiza una resonancia magnética donde se visualiza una gran tumoración en el espacio carotídeo izquierdo, la cual se biopsió obteniendo el diagnóstico histológico de paraganglioma. Al realizar el estudio de extensión se identificó la presencia de metástasis pulmonares y óseas, lo que confirma la malignidad del tumor.
Carotid body tumours are rare, slow-growing, highly destructive and vascularised neoplasms that have a neuroectodermal origin and are part of the diffuse neuroendocrine system. They are the most common extra-adrenal paragangliomas and represent 60% of all cervicocephalic glomus tumours and 0.6% of head and neck tumours.1 They are usually afunctional and are detected as a palpable mass. The presence of tachycardia, hypertension and tremors may indicate endocrine activity.2 Malignant glomus tumours account for 5–13% of cases, and exhibit aggressive local behaviour with infiltration of adjacent lymph nodes or distant metastases (liver, bone and lung).3 It is recommended to perform computed tomography (CT) and magnetic resonance imaging (MRI) for early detection and assessment of the extent and definitive treatment. Carotid angiography is highly sensitive to detecting small-size lesions. In recent years, the relationship between mutations in SDH genes and paragangliomas has become apparent, meaning that the genetic study of these patients is increasingly relevant for both diagnosis and treatment.4 Some nuclear imaging techniques such as somatostatin receptor scintigraphy (octreoscan) or positron emission tomography (PET) and the use of radiopharmaceuticals (F-DOPA, F-FDA and F-FDG) make it possible to detect these types of tumours to which they express high density of somatostatin receptors on the cell surface and due to their ability to capture amino acid precursors.5
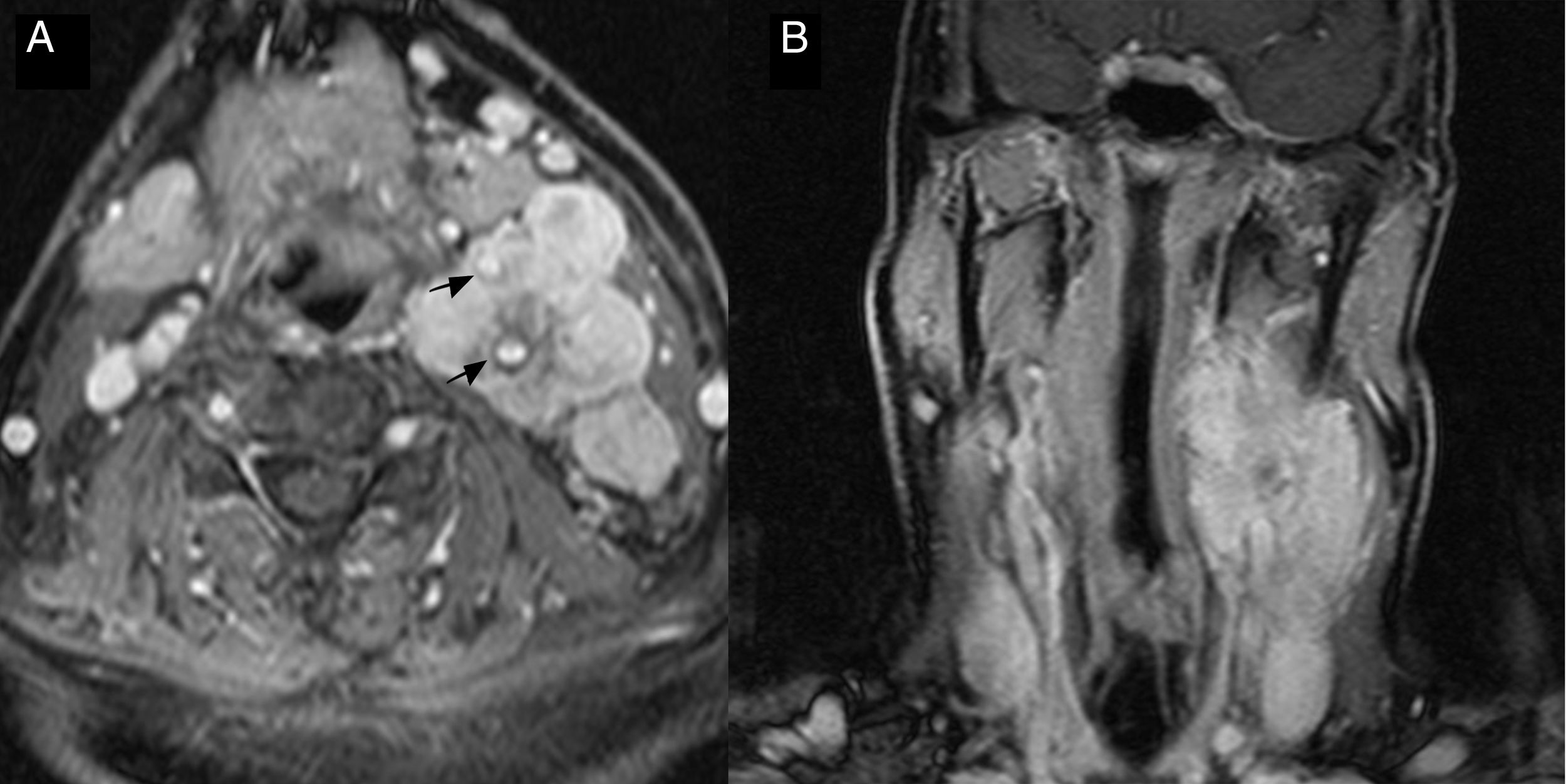
Presentation of the caseWe present the case of a 60-year-old man, undergoing follow-up for papillary carcinoma of the thyroid and disease-free transitional renal carcinoma, who presented with pain and paraesthesia in the right upper limb for several months. MRI of the cervical spine was performed, showing a voluminous well-defined tumour with intense enhancement in the left carotid space that encompassed the common carotid artery, as well as the proximal portion of the internal and external carotid arteries (Fig. 1). A biopsy was performed of the cervical tumour that reported infiltration by neuroendocrine tumour with histological signs of paraganglioma.
Cervical magnetic resonance. (A) Axial T1 with fat saturation and intravenous contrast. (B) Coronal T1 with fat saturation and intravenous contrast. Large tumour in the left carotid space that encompasses and separates the internal and external carotid arteries without reducing their calibre and showing homogeneous enhancement after administration of gadolinium.
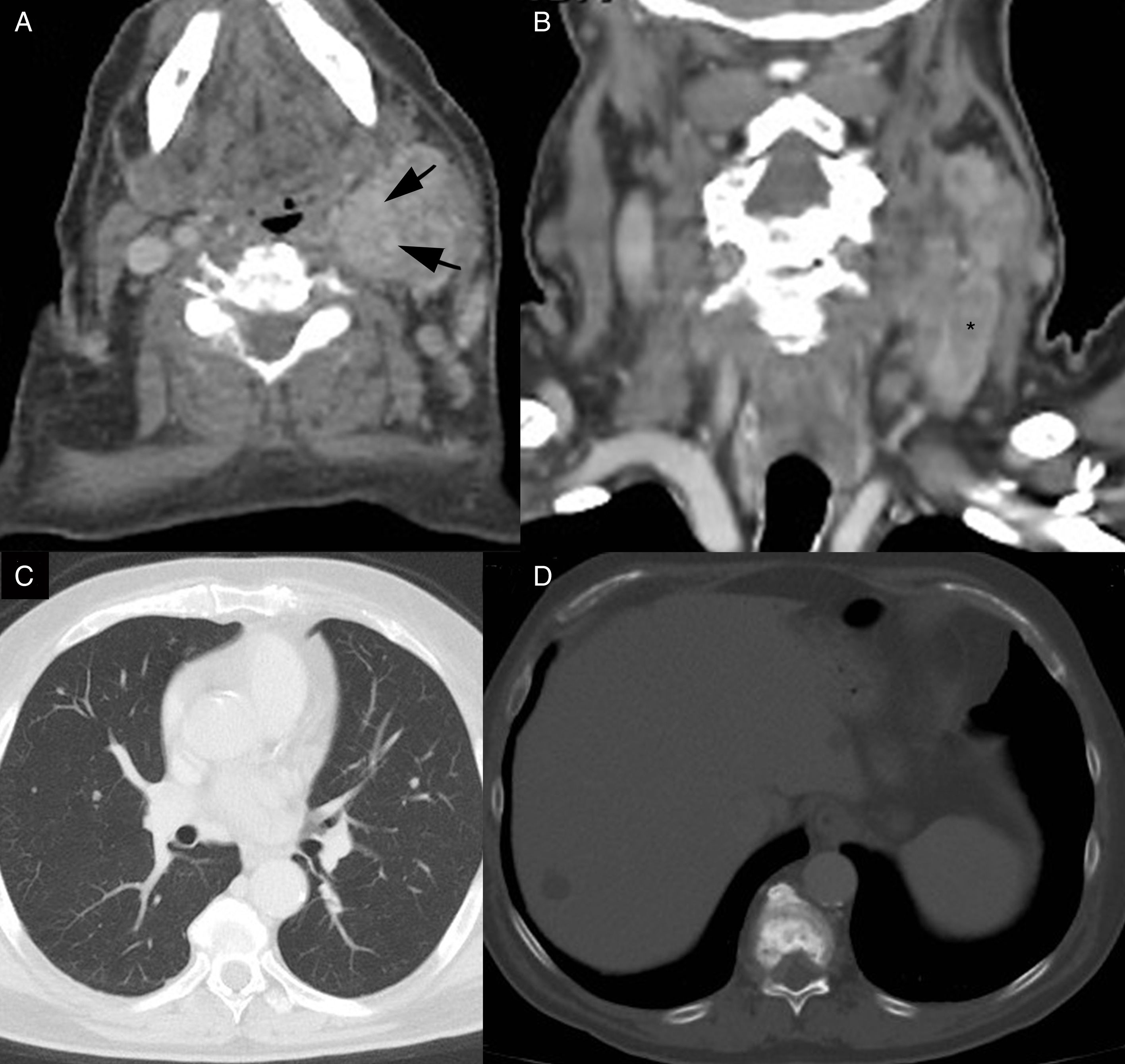
The study was completed with cervical CT scan with intravenous contrast in which thrombosis of the internal jugular vein was observed and multiple adenopathies with signs of necrosis. In addition, elevation of metanephrines in urine and noradrenaline in blood was observed. Given these findings, the extension study with a CT scan of the chest, abdomen and pelvis was performed, where multiple bilateral lung nodules compatible with metastasis and metastatic blast involvement of several dorsal vertebral bodies were visualised (Fig. 2).
Axial and coronal cervicothoracic computed tomography with IV contrast. (A and B) Voluminous left cervical tumour, heterogeneous, with intense uptake of contrast, which engulfs the carotid arteries (arrows) with thrombosis of the internal jugular vein (asterisk). (C) Multiple millimetric pulmonary nodules, of bilateral and diffuse distribution, compatible with metastasis. (D) Metastatic blastic involvement of dorsal vertebral body. Focal hepatic lesions corresponding to simple cysts, confirmed by hepatic magnetic resonance.
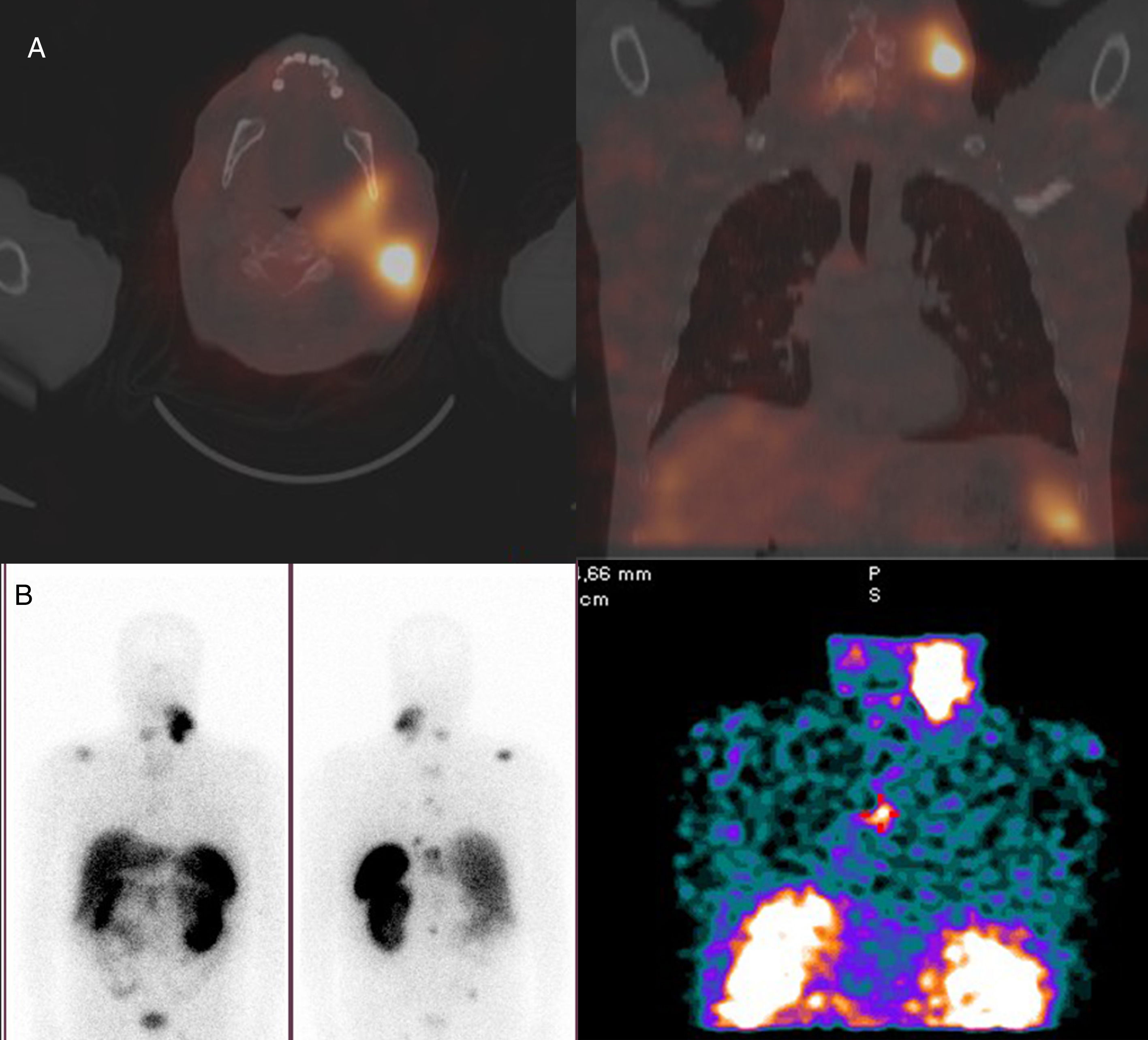
Single-photon emission computed tomography (SPECT) of somatostatin receptors was requested, in which hypercaptation in the left cervical region and foci compatible with multiple bone metastases were observed (Fig. 3). The genetic study was positive for the mutation in the SDHC gene (deletion of exons 4–6). The patient received three cycles of chemotherapy with cyclophosphamide–vincristine–dacarbazine regimen and radiation therapy at a dose of 30Gy, and remained stable for two years until the disease progressed, with the onset of peritoneal carcinomatosis and growth of the left cervical mass and the lung and bone metastases that caused a syndrome of spinal cord compression with evolution to bilateral paraparesis. Despite having a good initial response to a new cycle of chemotherapy, the patient died four years after the initial diagnosis.
(A) Axial and coronal cervicothoracic SPECT-CT. Increased uptake of the left cervical mass. (B) Somatostatin receptor scintigraphy study. Hyperuptake in the left cervical area corresponding to the tumour and adenopathies. Multiple foci of bone hyperuptake compatible with metastasis in the spine, right clavicle and right sacroiliac joint. Rest with normal scintigraphic pattern with uptake in the liver, spleen, left kidney (monorenal patient due to a right radical nephrectomy) and bladder with background activity.
Paragangliomas are tumours from the chemoreceptor tissue (paraganglia) that is part of the extra-adrenal neuroendocrine system and originate in the neural crest. They appear mainly in the abdomen (85%) and are less common in the chest (12%) and in the region of the head and neck (3%).5 Paragangliomas can be diagnosed by the biochemical determination of metanephrines and methoxytyramine, as in this case in which there was elevated metanephrine in urine and noradrenaline in blood. Histologically, these tumours contain the three elements that are found in paraganglionic tissue: granular cells or type I main cells, type II sustentacular cells and abundant capillaries. In immunohistochemical studies, type I cells are positive for neuron-specific enolase, chromogranin A, synaptophysin and serotonin, while type II cells are positive for S-100 protein and glial fibrillary acidic protein. This positivity of type II cells for the S-100 protein is considered useful for diagnosis, since it demonstrates the paraganglionic origin of the tumour.3
Paragangliomas have a high density of type 2 somatostatin receptors on the cell surface, so somatostatin receptor scintigraphy studies (octreoscan) are useful in the diagnosis and monitoring of these tumours. To carry out these studies, octreotide (active synthetic somatostatin analogue) labelled with the radioisotope indium-111 that will bind to somatostatin receptors is used.6 In addition, these tumours are able to capture and decarboxylate amino acid precursors such as phenylalanine, which is metabolised to dopamine, adrenaline and noradrenaline. Metaiodobenzylguanidine (MIBG) is a noradrenaline analogue that radioactively labelled with iodine was the gold standard for this type of tumour until the development of newer radiopharmaceuticals such as the F-18 FDG or Ga-68 DOTA peptides, which have shown greater sensitivity and better imaging characteristics in staging, especially in the detection of metastases in functioning tumours. Currently, there are three peptides in clinical use (DOTATATE, DOTANOC and DOTATOC), all showing an especially high affinity for the type 2 somatostatin surface receptor.7
In the head and neck region, the carotid body is the most common location, often followed by the jugulotympanic region, vagal, and other less common sites (including the larynx, pharynx, and ciliary ganglion in the orbit).1
Carotid paraganglioma, also called carotid glomus, a chemodectoma or tumour of the carotid body, is a very rare neoplasm with a prevalence of 1–2 per 100,000 inhabitants and accounting for 60% of cervicocephalic paragangliomas and 0.6% of head and neck tumours. It has its origin in the carotid type I cells and can appear along the embryological migratory path that extends from the base of the skull to the aortic arch.3 They are highly vascularised, slow-growing neoplasms, which on the CT scan show as a well-defined soft tissue mass that is usually located in the carotid bifurcation. They present intense and homogeneous enhancement after the administration of intravenous contrast and their extension to the internal and external carotid arteries is common, with the characteristic widening of the carotid bifurcation (lyre sign) as can be seen in our case (Figs. 1 and 2). In MRI, they are hyperintense, homogeneous lesions in sequences enhanced in T2 and iso-hypointense in T1 with enhancement after administering gadolinium. MRI makes it possible to determine the extent more accurately than the CT scan, and can also detect tumours smaller than 5mm and better demonstrate the involvement of adjacent vessels. In our case, the tumour engulfed the carotid arteries and caused thrombosis of the internal jugular vein. Depending on the relationship between the tumour and the carotid arteries, they can be divided into three types according to the Shamblin classification, which determines the surgical treatment, since there is more indication in types I and II due to the lower rate of complications.8 Type I paragangliomas are well localised tumours, which do not invade the larger adjacent vessels and can be easily dissected. Type II vessels partially surround the vessels and compress the carotid arteries, but they can be dissected. Those that present large size and widely invade the carotids and adjacent structures requiring a partial or total resection of these arteries are considered type III. MR angiography can be performed in tumours larger than 1.5cm to study tumour vascularisation, and time-of-flight (TOF) sequences can be very useful. Digital subtraction arteriography makes it possible to detect the vascular supply of the lesion and to assess the relationship of the tumour with the carotids and the internal jugular vein to plan embolisation and surgery. The paragangliomas will show up as hypervascular masses with enlarged nutrient arteries, intense enhancement and early drainage veins. The most common nutrient vessel is the ascending pharyngeal artery. PET-CT is useful for the detection of metastases that will appear as hypermetabolic foci, in our case bone and lung.3 Most paragangliomas are sporadic, benign and solitary, although they can be bilateral in up to 10% of cases and malignant in 5–10%. They usually appear in the fourth and fifth decades of life. Hyperplastic paragangliomas are related to situations of chronic hypoxia such as obstructive pulmonary disease or living at high altitudes, and are bilateral, but with little malignancy; in fact, they are not considered true neoplasms. Cases of multiple paragangliomas are related to familial syndromes, mainly multiple endocrine neoplasms types IIA and IIB2 and malignancy and bilateralism are more common. There is also a proven relationship with phakomatosis such as neurofibromatosis, Von Hippel-Lindau syndrome or tuberous sclerosis. Advances in genetic research have allowed the identification of multiple genes involved in the pathogenesis of these tumours, which can be responsible for up to 35–45% of cases. Mutations in the SDHB and SDHD genes have greater penetrance and frequency, contribute to 70% of familial cases and up to 8% of sporadic cases, and are associated with greater aggressiveness and malignancy. In the genetic study of our patient, we observed a mutation in the SDHC gene in heterozygous form (deletion of exons 4–6), which is more related to paragangliomas of the carotid body, although its frequency of mutations (10%) and penetrance is lower.4 It was recommended to the first-degree relatives of the patient that predictive genetic risk testing be done as well, since they have a 50% probability of being carriers of said mutation. The patient had two male children who underwent this testing; the same mutation was detected in both.
The incidence of malignancy in paragangliomas varies between 2% and 36%.1 Malignant carotid paraganglioma is a very rare entity. In general, 10% of all paragangliomas are malignant: 16–19% vagal tumours, 6% tumours of the carotid body and less common (2–4%) jugulotympanic tumours. Malignant paragangliomas are often functional. Metastases are limited to the lymph nodes in 69% of cases. 10% are multicentric and familial. In addition, 10% are diagnosed incidentally as they are clinically silent.1
The isolated histological study is insufficient to determine the benignity or malignancy in these tumours, and they are considered malignant if the presence of metastasis is demonstrated in non-neuroendocrine tissue (lymph nodes, lung, liver and skin).2 Our case was a malignant paraganglioma without endocrine activity, but with lymph node, pulmonary and bone metastases. It is also for this reason that genetic testing has increasingly greater diagnostic value, since those patients with mutations of the SDHB and SDHD genes will have a higher risk of malignancy than in the SDHC gene (10%). The fact that our patient had a history of papillary carcinoma of the thyroid and renal carcinoma could reveal the relationship of these two types of tumours with mutations in the SDHC gene, since in the specialised literature they are more related to SDHB in the renal tumour and to SDHB and SDHD in both papillary and medullary thyroid tumours.4,9
Functioning paragangliomas are often malignant. In these tumours, the size greater than 5cm and the presence of invasion or metastasis are prognostic factors of the evolution of the disease.10 In the cases with histological confirmation of malignancy and/or signs of local infiltration in the imaging test of the disease, an extension study with CT scan, nuclear medicine and genetic testing will be carried out.
As in the case of our patient, radiation therapy combined with chemotherapy is the treatment of choice in most cases since due to its location and size few patients are candidates for surgical treatment due to the serious vascular and neurological complications that may develop.3 Pre-operative percutaneous embolisation decreases the size of the lesion and the risk of haemorrhage in larger tumours (>3–4cm). Embolisation can be palliative when they are not candidates for surgery.8 The prognosis depends on the location of the tumour, which will determine the complete resection or not of it, and the presence of distant metastasis, and can range from 60% five-year survival in cases with the possibility of complete resection and without dissemination up to 12% at five years in those with distant metastases.1
In conclusion, carotid paraganglioma is a rare entity in which malignancy occurs in a small percentage of cases in the form of metastatic involvement in non-neuroendocrine tissues. They are neuroendocrine tumours with an important genetic base that allows for a better characterisation of these and that should be known in clinical practice, prioritising its performance according to clinical data, family history, biochemical phenotype and tumour location. Radiological imaging studies (CT scan, MRI, PET-CT, somatostatin receptor scintigraphy – octreoscan) combined with anatomopathological and genetic testing are essential for diagnosis, assessment of the extent and the decision of the definitive treatment.
Authorship- 1.
Responsible for the integrity of the paper: CRM, DDB, AFI and NN.
- 2.
Conception of the paper: CRM, DDB, AFI and NN.
- 3.
Study design: CRM, DDB, AFI and NN.
- 4.
Data collection:
- 5.
Analysis and interpretation of data:
- 6.
Statistical processing:
- 7.
Literature search:
- 8.
Drafting of the paper:
- 9.
Critical review of the manuscript with intellectually relevant contributions:
- 10.
Approval of the final version: CRM, DDB, AFI and NN.
The authors declare that they have no conflicts of interest.
Please cite this article as: Rubio Maicas C, Dualde Beltrán D, Ferrández Izquierdo A, Nersesyan N. Paraganglioma carotídeo maligno. A propósito de un caso. Radiología. 2019;61:171–176.